Chapter: Clinical Anesthesiology: Perioperative & Critical Care Medicine: Anesthetic Complications
Occupational Hazards in Anesthesiology
OCCUPATIONAL HAZARDS IN ANESTHESIOLOGY
Anesthesiologists spend much of their workday exposed to anesthetic
gases, low-dose ionizing radiation, electromagnetic fields, blood products,
and workplace stress. Each of these can
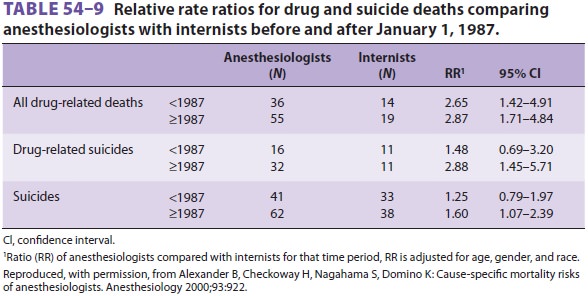
contribute to negative health effects in anesthesia practitio-ners. A 2000
paper compared the mortality risks of anesthesiologists and internists. Death
from heart disease or cancer did not differ between the groups; however,
anesthesiologists had an increased rate of suicides and drug-related deaths (Table
54–9). Anesthesiologists also had a greater
chance of death from external causes, such as boating, bicycling, and
aeronautical accidents compared with internists. Nevertheless, both
anesthesiologists and internists had lower mortality than the general
population, likely due to their higher socioeconomic status. Anesthesiologists’
access to intravenous opioids likely contributes to a 2.21 relative risk for
drug-related deaths compared with that of internists.
1. Chronic Exposure to Anesthetic Gases
There is no clear evidence that exposure to
trace amounts of anesthetic agents presents ahealth hazard to operating room
personnel. How-ever, because previous studies examining this issue have yielded
flawed but conflicting results, the US Occupational Health and Safety
Administration continues to set maximum acceptable trace concen-trations of
less than 25 ppm for nitrous oxide and 0.5 ppm for halogenated anesthetics (2
ppm if the halogenated agent is used alone). Achieving these low levels depends
on efficient scavenging equip-ment, adequate operating room ventilation, and
conscientious anesthetic technique. Most people cannot detect the odor of
volatile agents at a concen-tration of less than 30 ppm. If there is no
functioning scavenging system, anesthetic gas concentrations reach 3000 ppm for
nitrous oxide and 50 ppm for volatile agents.
Early studies indicated that female operating room staff might be at
increased risk of spontaneous abortion compared with other women. It is unclear
if other factors related to operating room activ-ity could also contribute to
the possibly increased potential for pregnancy loss.
2. Infectious Diseases
Hospital workers are exposed to many
infectious diseases prevalent in the community (eg, respiratory viral
infections, rubella, and tuberculosis).
Herpetic whitlow is an infection of the
finger with herpes simplex virus type 1 or 2 and usually involves direct
contact of previously traumatized skin with contaminated oral secretions.
Painful ves-icles appear at the site of infection. The diagnosis is confirmed
by the appearance of giant epithelial cells or nuclear inclusion bodies in a
smear taken from the base of a vesicle, the presence of a rise in herpes
simplex virus titer, or identification of the virus with antiserum. Treatment
is conservative and includes topical application of 5% acyclovir ointment.
Pre-vention involves wearing gloves when contacting oral secretions. Patients
at risk of harboring the virus include those suffering from other infections,
immunosuppression, cancer, and malnutrition. The risk of this condition has
virtually disappeared now that anesthesia personnel routinely wear gloves
dur-ing manipulation of the airway, which was not the case in the 1980s and
earlier.
Viral DNA has been identified in the smoke plume generated during laser
treatment of condy-lomata. The theoretical possibility of viral transmis-sion
from this source can be minimized by using smoke evacuators, gloves, and
appropriate OSHA approved masks.
More disturbing is the potential of acquiring
serious blood-borne infections, such as hepatitis B, hepatitis C, or human
immunodeficiency virus (HIV). Although parenteral transmission of these
diseases can occur following mucous membrane, cutaneous, or percutaneous
exposure to infected body fluids, accidental injury with a needle contami-nated
with infected blood represents the most com-mon occupational mechanism. The
risk of transmission can be estimated if three factors are known: the
prevalence of the infection within the patient population, the incidence of
exposure (eg, frequency of needlestick), and the rate of serocon-version after
a single exposure. The seroconversion rate after a specific exposure depends on
several fac-tors, including the infectivity of the organism, the stage of the
patient’s disease (extent of viremia), the size of the inoculum, and the immune
status of the healthcare provider. Rates of seroconversion fol-lowing a single
needlestick are estimated to rangebetween 0.3% and 30%. Hollow (hypodermic)
needles pose a greater risk than do solid (surgical) needles because of the
potentially larger inoc-ulum. The use of gloves, needleless systems, or
protected needle devices may decrease the incidence of some (but not all) types
of injury.
The initial management of needlesticks involves cleaning the wound and
notifying the appropriate authority within the health care facil-ity. After an
exposure, anesthesia workers should report to their institution’s emergency or
employee health department for appropriate counseling on postexposure
prophylaxis options. All OR staff should be made aware of the institution’s
employee health notification pathway for needle stick and other injuries
Fulminant hepatitis B (1% of acute
infections) carries a 60% mortality rate. Chronic active hepati-tis (<5% of all cases) is
associated with an increased incidence of cirrhosis of the liver and hepatocellu-lar
carcinoma. Transmission of the virus is primar-ily through contact with blood
products or body fluids. The diagnosis is confirmed by detection of hepatitis B
surface antigen (HBsAg). Uncompli-cated recovery is signaled by the
disappearance of HBsAg and the appearance of antibody to the surface antigen
(anti-HBs). A hepatitis B vaccine is available and is strongly recommended
prophylac-tically for anesthesia personnel. The appearance of anti-HBs after a
three-dose regimen indicates suc-cessful immunization.
Hepatitis C is another important occupational hazard in anesthesiology;
4% to 8% of hepatitis C infections occur in healthcare workers. Most (50% to
90%) of these infections lead to chronic hepatitis, which, although often
asymptomatic, can progress to liver failure and death. In fact, hepatitis C is
the most common cause of nonalcoholic cirrhosis in the United States. There is
currently no vaccine to pro-tect against hepatitis C infection.
Anesthesia personnel seem to be at a low, but
measureable, risk for the occupational contraction of HIV. The risk of
acquiring HIV infection follow-ing a single needlestick contaminated with blood
from an HIV-infected patient has been estimated at 0.4% to 0.5%. Because there
are documented reports of transmission of HIV from infected patients to
healthcare workers (including anesthesiologists), the Centers for Disease
Control and Prevention proposed guidelines that apply to all categories of
patient contact. These universal precautions, which are equally valid for protection
against hepatitis B orinfection, are as follows:
·
No recapping and the immediate
disposal of contaminated needles
·
Use of gloves and other barriers
during contact with open wounds and body fluids
·
Frequent hand washing
·
Use of proper techniques for
disinfection or the disposal of contaminated materials
·
Particular caution by pregnant
healthcare workers, and no contact with patients by workers who have exudative
or weeping skin lesions
3. Substance Abuse
Anesthesiology is a high-risk medical spe-cialty
for substance abuse. Probable reasonsfor this include the stress of anesthetic
practice and the easy availability of drugs with addiction poten-tial
(potentially attracting people at risk of addiction to the field). The
likelihood of developing substance abuse is increased by coexisting personal
problems (eg, marital or financial difficulties) or a family his-tory of
alcoholism or drug addiction.
The voluntary use of nonprescribed
mood-altering pharmaceuticals is a disease. If left untreated, substance abuse
often leads to death from drug overdose—intentional or unintentional. One of
the greatest challenges in treating drug abuse is identify-ing the afflicted
individual, as denial is a consistent feature. Unfortunately, changes evident
to an out-side observer are often both vague and late: reduced involvement in
social activities, subtle changes in appearance, extreme mood swings, and
altered work habits. Treatment begins with a careful, well-planned
intervention. Those inexperienced in this area would be well advised to consult
with their local medical society or licensing authority about how to proceed.
The goal is to enroll the individual in a formal reha-bilitation program. The
possibility that one may lose one’s medical license and be unable to return to
practice provides powerful motivation. Some diver-sion programs report a
success rate of approximately 70%; however, most rehabilitation programs
reportrecurrence rate of at least 25%. Long-term compli-ance often involves
continued participation in sup-port groups (eg, Narcotics Anonymous), random
urine testing, and oral naltrexone therapy (a long-acting opioid antagonist).
Effective prevention strat-egies are difficult to formulate; “better” control
of drug availability is unlikely to deter a determined individual. It is
unlikely that education about the severe consequences of substance abuse will
bring new information to the potential drug-abusing physician. There remains
controversy regarding the rate at which anesthesia staff will experience recidi-vism.
Many experts argue for a “one strike and you’re out” policy for anesthesiology
residents who abuse injectable drugs. The decision as to whether a fully
trained and certified physician who has been dis-covered to abuse injectable
drugs should return to anesthetic practice after completing a rehabilitation
program varies and depends on the rules and tra-ditions of the practice group,
the medical center, the relevant medical licensing board, and the per-ceived
likelihood of recidivism. Physicians return-ing to practice following
successful completion of a program must be carefully monitored over the long
term, as relapses can occur years after apparent suc-cessful rehabilitation.
Alcohol abuse is a common problem among physicians and nurses, and anes-thesia
personnel are no exception. Interventions for alcohol abuse, as is true for
injectable drug abuse, must be carefully orchestrated. Guidance from the local
medical society or licensing authority is highly recommended.
4. Ionizing Radiation Exposure
The use of imaging equipment (eg,
fluoroscopy) during surgery and interventional radiologic proce-dures exposes
the anesthesiologist to the potentialrisks of ionizing radiation. The three
most important methods of minimizing radiationdoses are limiting total exposure
time during pro-cedures, using proper barriers, and maximizing the distance
from the source of radiation. Anesthesiolo-gists who routinely perform
fluoroscopic image guided invasive procedures should consider wearing
protective eyeware incorporating radiation shield-ing. Lead glass partitions or
lead aprons with thyroid shields are mandatory protection for all personnel who
are exposed to ionizing radiation. The inverse square law states that the
dosage of radiation varies inversely with the square of the distance. Thus, the
exposure at 4 m will be one-sixteenth that at 1 m. The maximum recommended
occupational whole-body exposure to radiation is 5 rem/yr. This can be
monitored with an exposure badge. The health impact on operating room personnel
of exposure to electromagnetic radiation remains unclear.
Related Topics