Chapter: Clinical Anesthesiology: Perioperative & Critical Care Medicine: Anesthetic Complications
Anesthetic Complications: Peripheral Nerve Injury
PERIPHERAL NERVE INJURY
Nerve injury is a complication of being hospital-ized, with or without
surgery, regional, or general anesthesia. Peripheral nerve injury is a frequent
and vexing problem. In most cases, these injuries resolve within 6–12 weeks,
but some are permanent. Because peripheral neuropathies are commonly associated
(often incorrectly!) with failures of patient positioning, a review of
mechanisms and prevention is necessary.
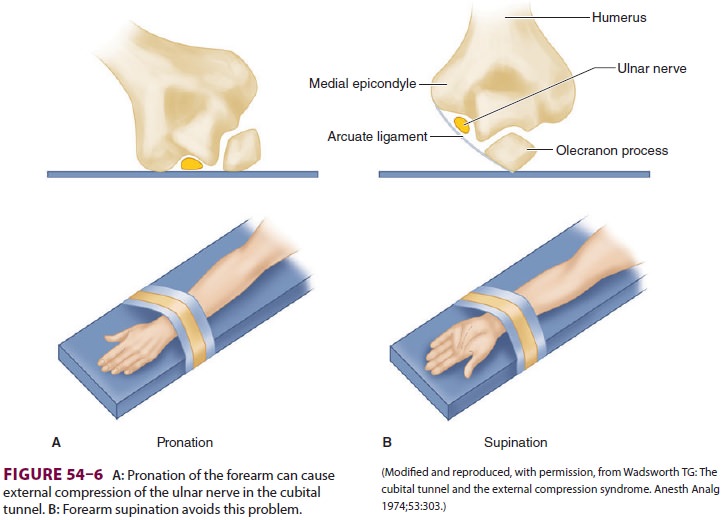
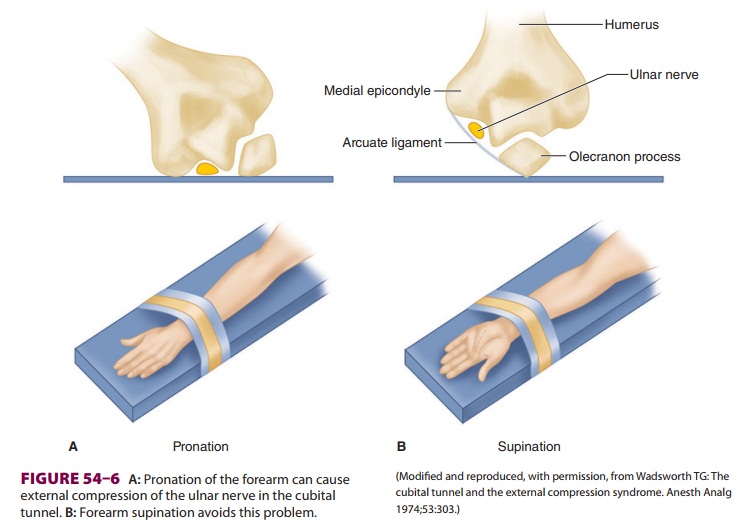
The most commonly injured peripheral nerve is
the ulnar nerve ( Figure 54–6).
In a retrospective study of over 1 million patients, ulnar neuropathy
(persisting for more than 3 months) occurred in approximately 1 in 2700
patients. Of interest, ini-tial symptoms were most frequently noted more than
24 hr after a surgical procedure. Risk factors included male gender, hospital
stay greater than 14 days, and very thin or obese body habitus. More than 50%
of these patients regained full sensory and motor function within 1 yr.
Anesthetic technique was not implicated as a risk factor; 25% of patients with
ulnar neuropathy underwent monitored care or lower extremity regional
technique. The ASA Closed Claims Project findings support most of these
results, including the delayed onset of symp-toms and the lack of relationship
between anesthe-sia technique and injury. This study also noted that many
neuropathies occurred despite notation of extra padding over the elbow area,
further negat-ing compression as a possible mechanism of injury. Finally, the
ASA Closed Claims Project investigators found no deviation from the standard of
care in the majority of patients who manifested nerve damage perioperatively.
The Role of Positioning
Other peripheral nerve injuries seem to be more closely related to positioning or surgical procedure. They may involve the peroneal nerve, the brachial plexus, or the femoral and sciatic nerves. External pressure on a nerve could compromise its perfusion, disrupt its cellular integrity, and eventually result in edema, ischemia, and necrosis. Pressure injuries are particularly likely when nerves pass through closed compartments or take a superficial course (eg, the peroneal nerve around the fibula). Lower extremity neuropathies, particularly those involving the pero-neal nerve, have been associated with such factors as extreme degrees (high) and prolonged (greater than 2 h) durations of the lithotomy position. But, these nerve injuries also sometimes occur when such con-ditions are not present. Other risk factors for lower extremity neuropathy include hypotension, thin body habitus, older age, vascular disease, diabetes, and cigarette smoking. An axillary (chest) “roll” is commonly used to reduce pressure on the inferior shoulder of patients in the lateral decubitus position. This roll should be located caudad to the axilla to prevent direct pressure on the brachial plexus and large enough to relieve any pressure from the mat-tress on the lower shoulder.
The data are convincing that some periph-eral
nerve injuries are not preventable. The risk of peripheral neuropathy should be
included in discussions leading to informed consent. When reasonable, patients
with contractures (or other causes of limited flexibility) can be positioned
before induction of anesthesia to check for feasibility and discomfort. Final
positioning should be evaluated prior to draping. In most circumstances, the
head and neck should be kept in a neutral position. Shoul-der braces to support
patients maintained in a Tren-delenberg position should be avoided if possible,
and shoulder abduction and lateral rotation should be minimized. The upper
extremities should not be extended greater than 90° at any joint. (There should
be no continuous external compression on the knee, ankle, or heel.) Although
injuries may still occur, additional padding may be helpful in vulnerable
areas. Documentation should include information on positioning, including the
presence of padding. Finally, patients who complain of sensory or motor
dysfunction in the postoperative period should be reassured that this is
usually a temporary condition. Motor and sensory function should be documented.
When symptoms persist for more than 24 hr, the patient should be referred to a
neurologist (or a physiatrist or hand surgeon) who is knowledgeable about
perioperative nerve damage for evaluation. Physiological testing, such as nerve
conduction and electromyographic studies, can be useful to docu-ment whether
nerve damage is a new or chronic condition. In the latter case, fibrillations
will be observed in chronically denervated muscles.
Complications Related to Positioning
Changes of body position have physiological
con-sequences that can be exaggerated in disease states. General and regional
anesthesia may limit the car-diovascular response to such a change. Even
posi-tions that are safe for short periods may eventually lead to complications
in persons who are not able to move in response to pain. For example, the
alco-holic patient who passes out on a hard floor or a park bench may awaken
with a brachial plexus injury. Similarly, regional and general anesthesia
abolish protective reflexes and predispose patients to injury.
Complications of postural hypotension, the most common physiological
consequence of posi-tioning, can be minimized by avoiding abrupt or extreme
position changes (eg, sitting up quickly), reversing the position if vital
signs deteriorate, keep-ing the patient well hydrated, and having vasoac-tive
drugs available to treat hypotension. Whereas maintaining a reduced level of
general anesthesia will decrease the likelihood of hypotension, light general
anesthesia will increase the likelihood that movement of the endotracheal tube
during posi-tioning will cause the patient to cough and become hypertensive.
Many complications, including air embolism, blindness from sustained
pressure on the globe, and finger amputation following a crush injury, can be
caused by improper patient positioning ( Table 54–4). These
complications are best prevented by evaluat-ing the patient’s postural
limitations during the pre-anesthetic visit; padding pressure points,
susceptible nerves, and any area of the body that will possibly be in contact with the operating table or its
attach-ments; avoiding flexion or extension of a joint to its limit; having an
awake patient assume the position
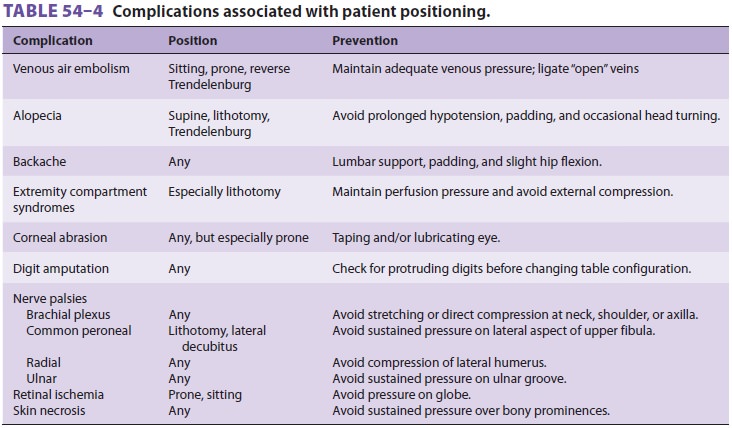
to ensure comfort; and understanding the poten-tial complications of
each position. Monitors must often be disconnected during patient
repositioning, making this a time of greater risk for unrecognized hemodynamic derangement.
Compartment syndromes can result from
hemorrhage into a closed space following a vascu-lar puncture or prolonged
venous outflow obstruc-tion, particularly when associated with hypotension. In
severe cases, this may lead to muscle necrosis, myoglobinuria, and renal
damage, unless the pres-sure within the extremity compartment is relieved by
surgical decompression (fasciotomy) or in the abdominal compartment by
laparotomy.
Related Topics