Chapter: Clinical Anesthesiology: Perioperative & Critical Care Medicine: Anesthetic Complications
Anesthetic Complications: Equipment Problems
EQUIPMENT PROBLEMS
“Equipment problems” is probably a misnomer;
the ASA Closed Claims Project review of 72 claims involving gas delivery
systems found that equipment misuse was
three times more commonthanequip-ment malfunction.
The majority (76%) of adverse
outcomes associated with gas delivery
problems were either death or permanent neurological damage.
Errors in drug administration also typically involve human error. It has
been suggested that as many as 20% of the drug doses given to hospitalized
patients are incorrect. Errors in drug administration account for 4% of cases
in the ASA Closed Claims Project, which found that errors resulting in claims
were most frequently due to either incorrect dosage or unintentional
administration of the wrong drug (syringe swap). In the latter category,
accidental administration of epinephrine proved particularly dangerous.
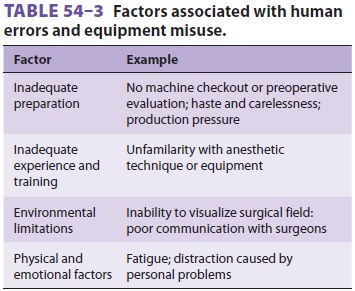
Another type of human error occurs when the
most critical problem is ignored because attention is inappropriately focused
on a less important problem or an incorrect solution (fixation error). Serious
anesthetic mishaps are often associated with distrac-tions and other factors
(Table 54–3). The impact of most equipment failures is decreased or avoided
when the problem is identified during a routine preoperative checkout performed
by adequatelytrained personnel. Many anesthetic fatalities occur only after a
series of coincidental circumstances, misjudgments, and technical errors
coincide (mishap chain).
Prevention
Strategies to reduce the incidence of serious anes-thetic complications
include better monitoring and anesthetic techniques, improved education, more
comprehensive protocols and standards of prac-tice, and active risk management
programs. Better monitoring and anesthetic techniques imply more comprehensive
monitoring and ongoing patient assessments and better designed anesthesia equip-ment
and workspaces. The fact that most accidents occur during the maintenance phase
of anesthesia— rather than during induction or emergence—implies a failure of
vigilance.
Inspection, palpation, percussion, and
ausculta-tion of the patient provide important information. Instruments should
supplement (but never replace) the anesthesiologist’s own senses. To minimize
errors in drug administration, drug syringes and ampoules in the workspace
should be restricted to those needed for the current specific case. Drugs
should be consistently diluted to the same concen-tration in the same way for
each use, and they should be clearly labeled. Computer systems for scanning
bar-coded drug labels are available that may help to reduce medication errors.
The conduct of all anes-thetics should follow a predictable pattern by which
the anesthetist actively surveys the monitors, the surgical field, and the
patient on a recurrent basis. In particular, patient positioning should be
frequently reassessed to avoid the possibility of compression or stretch
injuries. When surgical necessity requires patients to be placed in positions
where harm may occur or when hemodynamic manipulations (eg, deliberate
hypotension) are requested or required, the anesthesiologist should note on the
record the surgical request and remind the surgeon of any potential risks to
the patient.
Related Topics