Chapter: Clinical Anesthesiology: Perioperative & Critical Care Medicine: Anesthetic Complications
Adverse Anesthetic Outcomes
ADVERSE ANESTHETIC OUTCOMES
Incidence
There are several reasons why it is difficult
to accurately measure the incidence of adverse anesthesia-related outcomes.
First, it is often difficult to determine whether the cause of a poor outcome
is the patient’s underlying disease, the surgical proce-dure, or the anesthetic
management. In some cases, all three factors contribute to a poor outcome.
Clini-cally important measurable outcomes are relatively rare after elective
anesthetics. For example, death isclear endpoint, and perioperative
deaths do occur with some regularity. But, because deaths attribut-able to
anesthesia are much rarer, a very large series of patients must be studied to
assemble conclusions that have statistical significance. Nonetheless, many
studies have attempted to determine the incidence of complications due to
anesthesia. Unfortunately, studies vary in criteria for defining an
anesthesia-related adverse outcome and are limited by retro-spective analysis.
Perioperative mortality is usually defined as
death within 48 hr of surgery. It is clear that most perioperative fatalities
are due to the patient’s preop-erative disease or the surgical procedure. In a
study conducted between 1948 and 1952, anesthesia mor-tality in the United
States was approximately 5100 deaths per year or 3.3 deaths per 100,000 popula-tion.
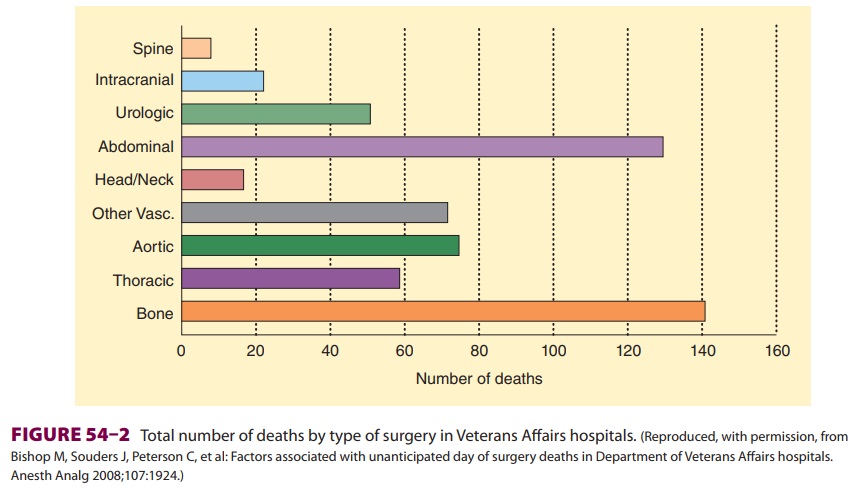
A review of cause of death files in the United States showed that the rate of
anesthesia-related deaths was 1.1/1,000,000 population or 1 anesthetic death
per 100,000 procedures between 1999 and 2005 (Figure 54–1). These results suggest a 97% decrease in anesthesia mortality since
the 1940s. However, a 2002 study reported an estimated rate of 1 death per
13,000 anesthetics. Due to differences in methodology, there are discrepancies
in the lit-erature as to how well anesthesiology is doing in achieving safe
practice. In a 2008 study of 815,077 patients (ASA class 1, 2, or 3) who
underwent elec-tive surgery at US Department of Veterans Affairs hospitals, the
mortality rate was 0.08% on the day of surgery. The strongest association with
periop-erative death was the type of surgery (Figure 54–2). Other factors associated with increased risk of death
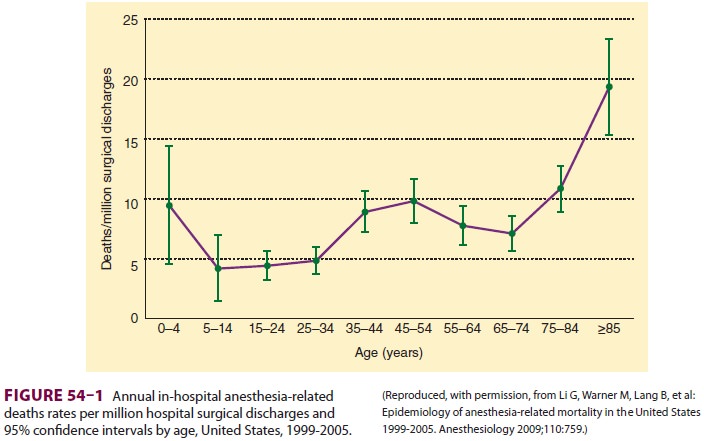
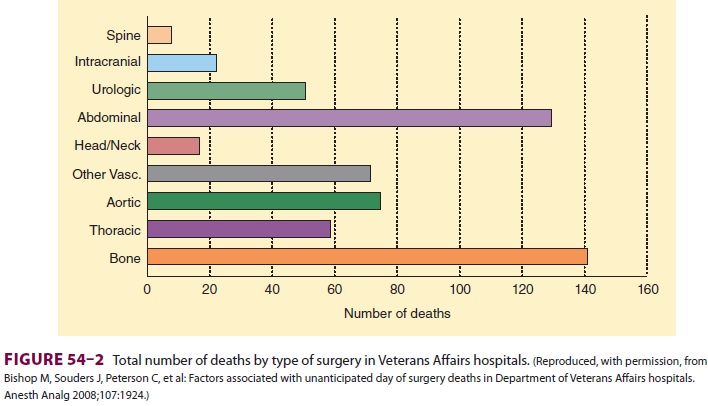
included dyspnea, reduced albumin concentrations, increased bilirubin, and increased creatinine con-centrations. A subsequent review of the 88 deaths that occurred on the surgical day noted that 13 ofthe patients might have benefitted from better anes-thesia care, and estimates suggest that death might have been prevented by better anesthesia practice in 1 of 13,900 cases. Additionally, this study reported that the immediate postsurgical period tended to be the time of unexpected mortality. Indeed, often missed opportunities for improved anesthetic care occur following complications when “failure to res-cue” contributes to patient demise.
American Society of Anesthesiologists Closed Claims Project
The goal of the ASA Closed Claims Project is
to identify common events leading to claims in anes-thesia, patterns of injury,
and strategies for injury prevention. It is a collection of closed malpractice
claims that provides a “snapshot” of anesthesia liabil-ity rather than a study
of the incidence of anesthetic complications, as only events that lead to the
filing of a malpractice claim are considered. The Closed Claims Project
consists of trained physicians who review claims against anesthesiologists
represented by some US malpractice insurers. The number of claims in the
database continues to rise each year as new claims are closed and reported. The
claims are grouped according to specific damaging events and complication type.
Closed Claims Project analyses have been reported for airway injury, nerve
injury, awareness, and so forth. These analyses provide insights into the
circumstances that result in claims; however, the incidence of a complication
cannot be determined from closed claim data, because we know neither the actual
incidence of the complica-tion (some with the complication may not file suit),
nor how many anesthetics were performed for which the particular complication
might possibly develop. Other similar analyses have been performed in the
United Kingdom, where National Health Service (NHS) Litigation Authority claims
are reviewed.
Causes
Anesthetic mishaps can be categorized as
preventable or unpreventable. Examples ofthe latter include sudden death
syndrome, fatal idiosyncratic drug reactions, or any poor outcome that occurs
despite proper management. How-ever, studies of anesthetic-related deaths or
near misses suggest that many accidents are prevent-able. Of these preventable
incidents, most involve human error (Table 54–1), as opposed to equipment
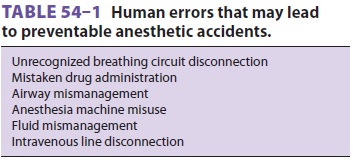
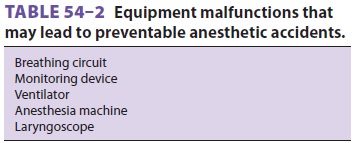
malfunctions (Table 54–2). Unfortunately, some rate of human error is inevitable, and a prevent-able
accident is not necessarily evidence of incom-petence. During the 1990s, the
top three causes for claims in the ASA Closed Claims Project were death (22%),
nerve injury (18%), and brain damage (9%). In a 2009 report based on an
analysis of NHS liti-gation records, anesthesia-related claims accounted for
2.5% of total claims filed and 2.4% of the value of all NHS claims. Moreover,
regional and obstetri-cal anesthesia were responsible for 44% and 29%,
respectively, of anesthesia-related claims filed. The authors of the latter
study noted that there are two ways to examine data related to patient harm:
critical incident and closed claim analyses. Clinical (or criti-cal) incident
data consider events that either cause harm or result in a “near-miss.” Comparison
between clinical incident datasets and closed claims analyses demonstrates that
not all critical events generate claims and that claims may be filed in the
absence of negligent care. Consequently, closed claims reports must always be
considered in this context.
Related Topics