Chapter: Medical Surgical Nursing: Assessment and Management of Patients With Breast Disorders
Nursing Process: The Patient With Breast Cancer
NURSING
PROCESS: THE PATIENT WITH BREAST CANCER
Assessment
The
health history includes an assessment of the patient’s reaction to the
diagnosis and her ability to cope with it. Pertinent ques-tions include the
following:
· How is the patient
responding to the diagnosis?
· What coping mechanisms
does she find most helpful?
· What psychological or
emotional supports does she have and use?
· Is there a partner,
family member, or friend available to assist her in making treatment choices?
· What are the most
important areas of information she needs?
· Is the patient
experiencing any discomfort?
Diagnosis
PREOPERATIVE NURSING DIAGNOSES
Based
on the health history and other assessment data, the patient’s major
preoperative nursing diagnoses may include the following:
· Deficient knowledge
about breast cancer and treatment options
· Anxiety related to
cancer diagnosis
· Fear related to specific
treatments, body image changes, or possible death
· Risk for ineffective
coping (individual or family) related to the diagnosis of breast cancer and
related treatment options
· Decisional conflict
related to treatment options
POSTOPERATIVE NURSING DIAGNOSES
Based
on the health history and other assessment data, the patient’s major
postoperative nursing diagnoses may include the following:
· Acute pain related to
surgical procedure
· Impaired skin integrity
due to surgical incision
· Risk for infection
related to surgical incision and presence of surgical drain
· Disturbed body image
related to loss or alteration of the breast related to the surgical procedure
· Risk for impaired
adjustment related to the diagnosis of cancer, surgical treatment, and fear of
death
· Self-care deficit
related to partial immobility of upper ex-tremity on operative side
· Disturbed sensory
perception (kinesthesia) related to sensa-tions in affected arm, breast, or
chest wall Risk for sexual dysfunction related to loss of body part, change in
self-image, and fear of partner’s responses
· Deficient knowledge:
drain management after breast surgery
· Deficient knowledge: arm
exercises to regain mobility of affected extremity
· Deficient knowledge:
hand and arm care after an axillary lymph node dissection
COLLABORATIVE PROBLEMS/ POTENTIAL COMPLICATIONS
Based
on the assessment data, potential complications may in-clude the following:
· Lymphedema
· Hematoma formation
· Infection
Planning and Goals
The major goals for the patient may include
increased knowledge about the disease and its treatment; reduction of
preoperative and postoperative fears, anxiety, and emotional stress;
improvement of decision-making ability; pain management; maintenance of skin
integrity; improved self-concept; improved sexual function; and the absence of
complications.
Preoperative Nursing Interventions
EXPLAINING BREAST CANCER AND TREATMENT OPTIONS
The
patient confronting the diagnosis of breast cancer reacts with fear, dread, and
anxiety. In view of the usually overwhelming emotional reactions to the
diagnosis, the patient must be given time to absorb the significance of the
diagnosis and any informa-tion that will help her to evaluate treatment
options.
The
nurse caring for the woman who has just received a diag-nosis of breast cancer
needs to be knowledgeable about current treatment options and able to discuss
them with the patient. The nurse should be aware of the information that has
been given to the patient by the physician.
Information
about the surgery, the location and extent of the tumor, and postoperative
treatments involving radiation therapy and chemotherapy are details that the
patient needs to enable her to make informed decisions. As appropriate, the
nurse discusses with the patient medications, the extent of treatment,
manage-ment of side effects, possible reactions after treatment, frequency and
duration of treatment, and treatment goals. Methods to compensate for physical
changes related to mastectomy (eg, pros-theses and plastic surgery) are also
discussed and planned. The amount and timing of the information provided are
based on the patient’s responses, coping ability, and readiness to learn.
REDUCING FEAR AND ANXIETY AND IMPROVING COPING ABILITY
The
patient’s emotional preparation begins when the tentative di-agnosis of cancer
is made. Patients who have lost close relatives to breast cancer (or any
cancer) may have difficulty coping with the possible diagnosis of breast cancer
because memories of loss and death can emerge during their own crisis.
The
patient may have the diagnostic procedure performed in the surgeon’s office or
in the hospital when she is admitted for ambulatory or same-day surgery for a
biopsy. Fears and concerns are common and are discussed with the patient. If
she will un-dergo a mastectomy, information about various resources and
op-tions is provided. Such services include prostheses, reconstructive surgery,
and groups such as Reach to Recovery. Discussion with a plastic surgeon about
the various options for reconstructive surgery can be a valuable source of
information and support.
The
nurse provides anticipatory teaching and counseling at each stage of the
process and identifies the sensations that can be expected during additional
diagnostic procedures. The nurse also discusses the implications of each
treatment option and how it may affect various aspects of the patient’s
treatment course and lifestyle. The patient is introduced to other members of
the on-cology team (eg, radiation oncologist, medical oncologist, oncol-ogy
nurse, and social worker) and is acquainted with the role of each in her care.
After the treatment plan has been established, the nurse needs to promote
preoperative physical, psychological, social, and nutritional well-being. The
patient usually prefers to be active in her care and decision making. Some
women find it helpful and reassuring to talk to a breast cancer survivor,
some-one who has completed treatment and has been trained as a vol-unteer to
talk with newly diagnosed patients.
PROMOTING DECISION-MAKING ABILITY
At
times, a patient may demonstrate behavior that indicates she cannot make a
decision about treatment. Careful guidance and supportive counseling are the
interventions the nurse can use to help such a patient. Also, encouraging the
patient to take one step of the treatment process at a time can be helpful. The
advanced practice nurse or oncology social worker can be helpful for patients
and family members in discussing some of the personal issues that may arise in
relation to treatment. Some patients may need a men-tal health consultation
before surgery to assist them in coping with the diagnosis and impending
treatment. Such patients may have had a history of psychiatric problems or
demonstrate be-havior that leads the surgeon or nurse to initiate a referral to
the psychiatrist, psychologist, or psychiatric clinical nurse specialist.
Postoperative Nursing Interventions
RELIEVING PAIN AND DISCOMFORT
Ongoing
nursing assessment of pain and discomfort is important because patients
experience differing degrees of pain intensity. Some women may have more
generalized pain and discomfort of the chest wall, affected breast, or affected
arm. Moderate elevation of the involved extremity is one means of relieving
pain because it decreases tension on the surgical incision, promotes
circulation, and prevents venous congestion in the affected extremity.
Intra-venous or intramuscular opioid analgesic agents are another method to
manage pain in the initial postoperative phase. After the patient is taking
fluids and food and the anesthesia has cleared sufficiently (usually by the
next morning), oral analgesic agents can be effective in relieving pain.
Patient teaching before dis-charge then becomes important in managing
discomfort after surgery because pain intensity varies widely. Patients should
be encouraged to take analgesic agents (opioid or nonopioid anal-gesic
medications such as acetaminophen) before exercises or at bedtime and also to
take a warm shower twice daily (usually al-lowed on the second postoperative
day) to alleviate the discom-fort that comes from referred muscle pain.
MAINTAINING SKIN INTEGRITY AND PREVENTING INFECTION
In the
immediate postoperative period, the patient will have a snug but not tight
dressing or a surgical bra packed with gauze over the surgical site and one or
more drainage tubes in place. A particular concern is preventing fluid from
accumulating under the chest wall incision or in the axilla by maintaining the
patency of the sur-gical drains. The dressings and drains should be inspected
for bleeding and the extent of drainage monitored regularly.
If a
hematoma develops, it usually occurs within the first 12 hours after surgery;
thus, monitoring the incision is important. A hematoma could cause necrosis of
the surgical flaps, although this complication is rare in breast surgery
patients. If either of these complications occurs, the surgeon should be
notified, and the patient should have an Ace wrap placed around the incision
and an ice pack applied. Initially, the fluid in the surgical drain appears
bloody, but it gradually changes to a serosanguinous and then a serous fluid
during the next several days. The drain is usu-ally left in place for 7 to 10
days and is then removed after the output is less than 30 mL in a 24-hour
period. The patient is dis-charged home with the drains in place; therefore,
teaching of the patient and family is important to ensure correct management of
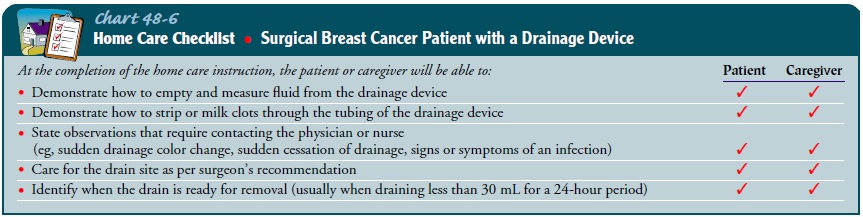
the drainage system (Chart 48-6).
Dressing
changes present an opportunity for the nurse and pa-tient to discuss the
incision, particularly how it looks and feels and the progressive changes in
its appearance. The nurse explains the care of the incision, sensations to
expect, and the possible signs and symptoms of an infection. Generally, the
patient may shower on the second postoperative day and wash the incision and
drain site with soap and water to prevent infection. A dry dressing should be
applied to the incision each day for 7 days. The patient needs to know that
sensation is decreased in the op-erative area because the nerves were disrupted
during surgery and that gentle care is needed to avoid injury. After the
incision is completely healed (usually 4 to 6 weeks), lotions or creams may be
applied to the area to increase skin elasticity. After the incision is fully
healed, the patient may again use deodorant on the af-fected side, although
many women note that they no longer per-spire as much as before the surgery.
PROMOTING POSITIVE BODY IMAGE
During teaching sessions, the nurse can address the patient’s per-ception of the body image changes and physical alteration of the breast.
Patients may initially be uncomfortable looking at the sur-gical incision. No
matter how prepared a patient may be, the view of her incision and absence of
her breast is often difficult for her. Exploring this sensitive area must be a
careful nursing action, and cues provided by the patient must be respected and
sensitively handled. Privacy is a consideration when assisting the woman to
view her incision fully for the first time and allows the patient to express
her feelings safely to the nurse. Asking the patient what she perceives,
acknowledging her feelings, and allowing her to ex-press her emotions are
important nursing actions. Explaining that her feelings are a normal response
to breast cancer surgery may be reassuring to the patient. Ideally, she will
see the incision for the first time when she is with the nurse or another
health care pro-vider who is available for support. With short hospital stays,
many women will view the incision for the first time with the home care nurse
or ambulatory care nurse at the time of postoperative follow-up visits.
PROMOTING POSITIVE ADJUSTMENT AND COPING
Ongoing
assessment of the patient’s concerns related to the diag-nosis of cancer, the
consequences of surgical treatment, and fear of death is important in
determining her progress in adjusting and the effectiveness of her coping
strategies. Assisting the patient in identifying and mobilizing her support
systems is important. The patient’s spouse or partner may need guidance,
support, and education as well. The patient and spouse may benefit from a wide
network of available community resources, including the American Cancer
Society’s Reach to Recovery program, advocacy groups, or a spiritual advisor.
Encouraging the patient to discuss issues and concerns with other patients who
have had breast can-cer may help her to understand that her feelings are normal
and that other women who have had breast cancer can provide in-valuable support
and understanding.
Another
important aspect of promoting the patient’s adjust-ment and coping includes
answering questions and addressing her concerns about the treatment options
that may follow sur-gery. After the surgery has been completed, thoughts about
what lies in the future in terms of additional treatment are normal, and this
topic can cause understandable anxiety. Refocusing the pa-tient on the recovery
from surgery, while addressing her concerns and answering her questions, can be
helpful. Being knowledge-able about the plan of care and encouraging the
patient to ask questions of the appropriate members of the health care team
will also promote coping during recovery.
A few
women require additional support to adjust to the di-agnosis and the changes
that it brings. If a woman displays in-effective coping, counseling or
consultation with a mental health practitioner may be indicated.
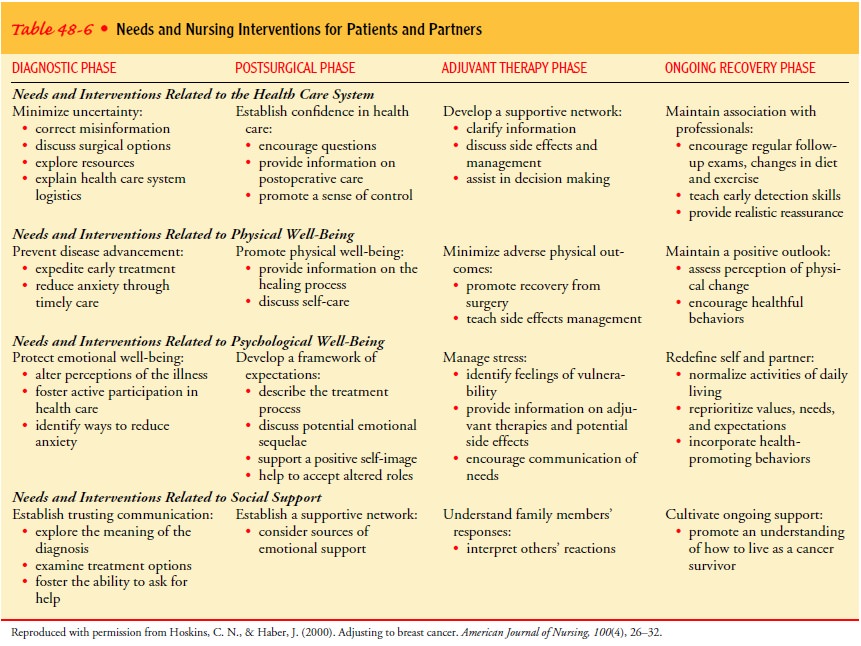
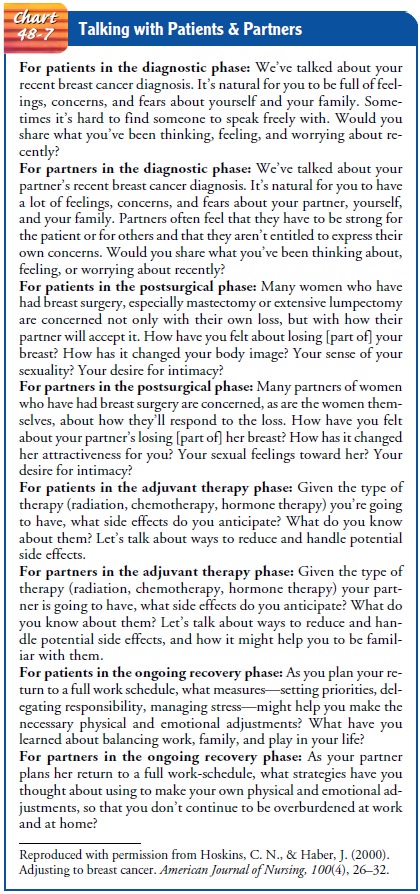
Table 48-6 summarizes the needs of and nursing interventions for patients and their partners at various stages of the breast can cer experience. Chart 48-7 provides insights into ways to initiate conversations with patients and their partners in different phases of therapy.
PROMOTING PARTICIPATION IN CARE
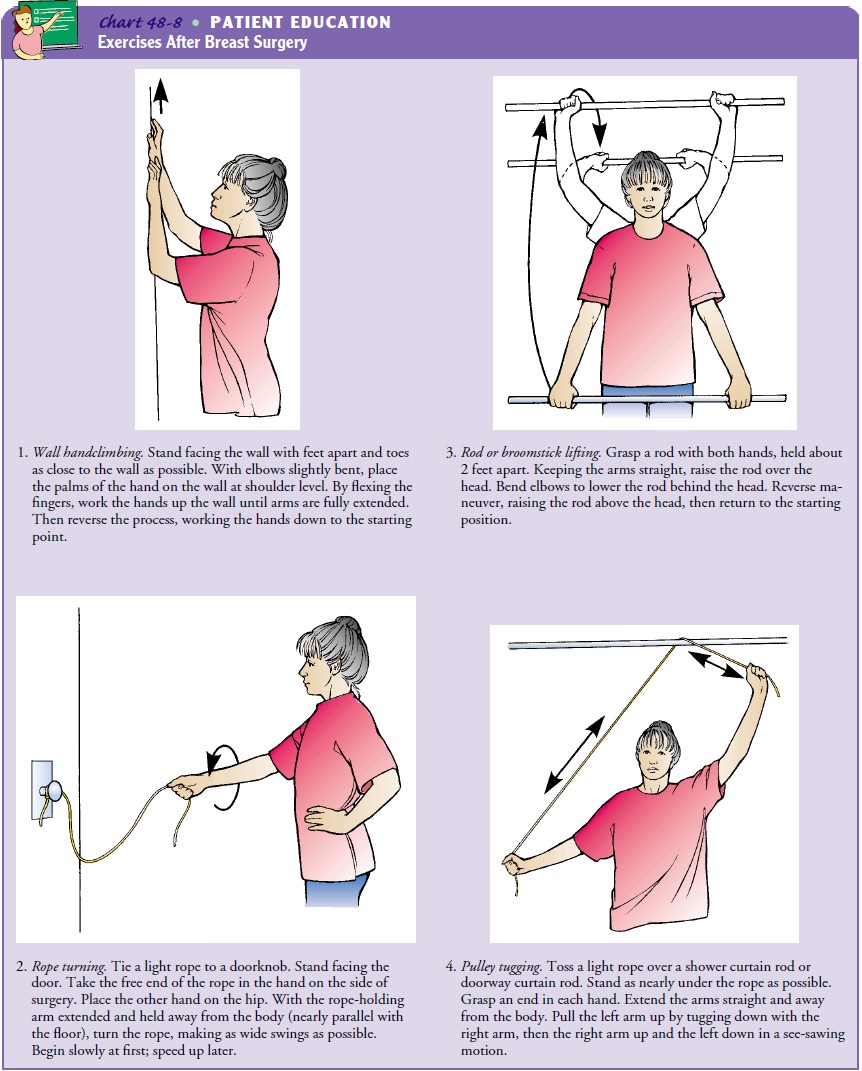
Ambulation is encouraged when the patient is free of postanes-thesia nausea and is tolerating fluids. The nurse supports the pa-tient on the nonoperative side. Exercises (hand, shoulder, arm, and respiratory) are initiated on the second postoperative day, al-though instruction occurs on the first postoperative day. The goals of the exercise regimen are to increase circulation and mus-cle strength, prevent joint stiffness and contractures, and restore full range of motion. Hand exercises are also important for the same reasons.
Postmastectomy
exercises (Chart 48-8) are usually performed three times daily for 20 minutes
at a time until full range of mo-tion is restored (generally 4 to 6 weeks).
Showering before exercis-ing loosens stiff muscles, and taking an analgesic
agent 30 minutes before beginning exercise increases the patient’s ability to
comply with the regimen. Also, self-care activities, such as brushing the
teeth, washing the face, and combing and brushing the hair, are physically and
emotionally therapeutic because they aid in restor-ing arm function and a sense
of normalcy for the patient.
The
nurse encourages the patient to use the muscles in both arms and to maintain
proper posture. If a patient is favoring or splinting the affected side, or not
standing up straight, any exer-cise will be ineffective. If a patient has skin
grafts, a tense, tight surgical incision, or immediate reconstruction,
exercises may need to be prescribed specifically and introduced gradually. Most
patients find that after the drain is removed, range of motion re-turns quickly
if they have been compliant with their exercise pro-grams. This reinforcement
may be provided in the outpatient setting by the ambulatory care nurse or the
home care nurse.
Patients
are instructed regarding activity limitations while healing postoperatively.
Generally, heavy lifting is avoided, al-though normal household and
work-related activities are pro-moted to maintain muscle tone. Driving may
begin after the drain is removed and when the patient has full range of motion
and is no longer taking opioid analgesic agents. General guide-lines for
activity focus on gradually introducing previous activi-ties (eg, bowling,
weight-training) when fully healed, although checking with the physician
beforehand is usually indicated.
Transient
edema in the affected extremity is common during the healing period, and women
are encouraged to elevate the arm above the level of the heart on a pillow for
45 minutes at a time three times daily to promote circulation. Performing the
pre-scribed exercises also assists in reducing the transient edema. Pre-vention
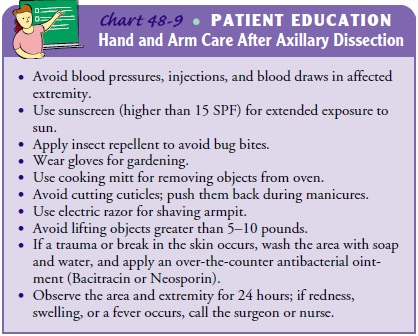
of lymphedema is taught to patients before discharge. Hand and arm care after
an axillary lymph node dissection fo-cuses on the prevention of injury or
trauma to the affected ex-tremity, which increases the likelihood of developing
lymphedema (Chart 48-9).
MANAGING POSTOPERATIVE SENSATIONS
Because
nerves in the skin are cut during breast surgery, patients experience a variety
of sensations. Common sensations are tight-ness, pulling, burning, and tingling
along the chest wall, in the axilla, and along the inside aspect of the upper
arm. They tend to become more noticeable and increase as the patient begins to
heal. They usually persist for several months up to a year and then begin to
diminish. Explaining to the patient that this is a normal part of healing helps
to reassure her that these sensations are not indicative of a problem.
Performing the exercises may decrease the sensations. Acetaminophen (Tylenol),
taken as needed, also assists in managing the discomfort. Many breast surgery
patients report these sensations as one of the most bothersome aspects of
having the surgery.
IMPROVING SEXUAL FUNCTION
Most breast surgery patients are physically allowed to engage in sexual activity once discharged from the hospital. However, any change in the patient’s body image and self-esteem or the part-ner’s response may increase the couple’s anxiety level and may af-fect sexual function. Some partners may have difficulty looking at the incision, whereas others appear to be unaffected and comfortable.
Either response affects the patient’s self-image, sexual-ity, and acceptance.
Open discussion and clear communication about how the patient sees herself and
about possible decreased libido related to fatigue, anxiety, or nausea may help
to clarify is-sues for her and her partner. Encouraging discussion about fears,
needs, and desires may reduce the couple’s stress. Suggestions regarding
varying the time of day for sexual activity (when the patient is less tired) or
assuming positions that are more com-fortable can be helpful, as are other
options for expressing affec-tion (eg, hugging, kissing, manual stimulation).
Most
patients and their partners adjust with minimal diffi-culty if they openly
discuss their concerns; however, if problems develop or persist, referral to a
psychosocial resource (psycholo-gist, psychiatrist, or psychiatric clinical
nurse specialist, social worker, or sex therapist) can be helpful for the woman
and her partner. To identify difficulty in sexual relationships, the
ambu-latory care nurse and home care nurse must be sensitive to this issue
following treatment for breast cancer and must initiate dis-cussion with the
patient.
MONITORING AND MANAGING POTENTIAL COMPLICATIONS
Lymphedema
Lymphedema
can occur any time after an axillary lymph node dissection. Lymphedema results
if functioning lymphatic chan-nels are inadequate to ensure a return flow of
lymph fluid to the general circulation. After removal of axillary nodes,
collateral or auxiliary circulation must take over their function. Transient
edema in the postoperative period occurs until this collateral cir-culation has
fully assumed functioning for the removed nodes, which generally occurs within
a month by moving and exercising the affected arm. Patients need reassurance
that this transient swelling is not lymphedema. Education about how to prevent
lymphedema is an important part of hand and arm care after an axillary
dissection. Lymphedema occurs in about 10% to 20% of patients who undergo an
axillary dissection. Risk factors for lym-phedema are increasing age, obesity,
presence of extensive axillary disease, radiation treatment, and injury or
infection to the ex-tremity. Patients should follow these guidelines to prevent
injury to the affected extremity because lymphedema is subsequently associated
with a trauma of some type.
If
lymphedema occurs, the patient should contact the surgeon or nurse to discuss
management because she may need a course of antibiotics or specific exercises
to decrease the swelling. Em-phasis should be placed on early intervention
because lymphe-dema can be manageable if treated early; however, if allowed to
progress without treatment, the swelling can become painful and difficult to
reverse. Management consists of arm elevation with the elbow above the shoulder
and the hand higher than the elbow, along with specific exercises, such as hand
pumps. A referral to a physical therapist or rehabilitation specialist may be
necessary for a custom-made elastic sleeve, exercises, manual lymph drainage,
or a special pump to decrease swelling.
Hematoma Formation
Hematoma
formation may occur after either mastectomy or breast conservation. The nurse
monitors the surgical site for excessive swelling and monitors the drainage
device, if present. Gross swelling or output from the drain may indicate
hematoma for-mation, and the surgeon should be notified promptly. Depend-ing on
the surgeon’s assessment, an Ace wrap may be applied for compression of the
surgical site along with ice packs for 24 hours, or the patient may be returned
to surgery to identify the source of bleeding. The nurse monitors the site and
reassures the patient that this complication is rare but does occur and that
she will be assisted through its management. A calm demeanor on the part of the
nurse helps prevent anxiety and panic on the part of the patient.
Infection
Infection
follows breast surgery in about 1 in 100 patients. In-fection can occur for a
variety of reasons, including concurrent conditions (diabetes, immune
disorders, advanced age) and ex-posure to pathogens. In addition, cellulitis
may occur after breast surgery. Both preoperatively and before discharge,
patients are taught to monitor for signs and symptoms of infection (redness,
foul-smelling drainage, temperature greater than 100.4°F) and
to contact the surgeon or nurse for evaluation. Treatment consists of oral or
intravenous antibiotics for 1 or 2 weeks, depending on the severity of the
infection. Cultures are taken of any foul-smelling discharge. Infections are a
serious threat to women who have had breast reconstruction because they may
lose the breast mound if the infection persists; there is a risk of lymphedema
in women who develop an infection and have had an axillary lymph node
dissection.
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care
Patients
who undergo breast surgery receive a tremendous amount of information before
and after surgery. Additional teaching is necessary to prepare the patient and
family to manage aspects of care after home discharge. Even though the
ambulatory care nurse prepares the patient for what to expect postoperatively,
the details often appear less important to the patient in light of the
diagno-sis of breast cancer. Thus, teaching may need to be repeated and
reinforced postoperatively. Most patients are discharged 1 or 2 days after the
surgery with the drains in place. The inpatient nurse as-sesses the patient’s
readiness to assume self-care and focuses on teaching the patient incision
care; signs to report, such as an in-fection; pain management; arm exercises;
hand and arm care; and management of the drainage system at home. Family
members may be included in the discharge teaching, and many women find it
reassuring and helpful to have another person assist them with management of the
drainage system. The ambulatory care nurse reinforces teaching by telephone
follow-up and during postoper-ative visits in the office.
Continuing Care
Referral
for home care may be indicated to assist the patient and family caregiver with
postoperative care at home. The home care nurse assesses the patient’s incision
and drainage system, physical and psychological status, adequacy of pain
management, and ad-herence to the exercise plan. In addition, the home care
nurse reinforces previous teaching and communicates important phy-siologic
findings or psychosocial issues to the patient’s primary care provider, nurse,
or surgeon.
Follow-up
visits to the physician after diagnosis and treatment of breast cancer depend
on the individual and on postoperative treatments, stage of disease at
diagnosis, late effects from cancer, and the patient’s adaptation. Visits every
3 months for 2 years, followed by every 6 months up to 5 years, may be then
extended to annual examinations, depending on the patient’s progress and the
physician’s preference. A disease-free state for as long as pos-sible is the
goal. Patients are also encouraged to do BSE on the re-maining breast (and
operative side if breast-conserving surgery was done) and the chest wall (after
mastectomy) between ap-pointments because the risk for cancer in the remaining
breast (or recurrence in the operative breast) is about 1% per year after the
original diagnosis. Additional screening is done with annual mammography.
Ultrasound and MRI are being used more com-monly with women who have survived
breast cancer. Because it is common to ignore routine health care when a major
health issue arises, the woman is reminded of the importance of partic-ipating
in health promotion activities and other health screening. Because some
problems with coping may not occur until the woman has returned to more usual
routines, the ambulatory care nurse needs to be sensitive to this issue and
encourage discussion throughout the recovery period.
Evaluation
EXPECTED PREOPERATIVE PATIENT OUTCOMES
Expected preoperative patient outcomes may include:
1) Exhibits knowledge about
diagnosis and treatment options
a) Asks relevant questions
about diagnosis and available treatments
b) States rationale for
surgery and other treatment options
c) Describes advantages and
disadvantages of treatment options
2) Verbalizes willingness
to deal with anxiety and fears re-lated to the diagnosis and the effects of
surgery on self-image and sexual functioning
3) Demonstrates ability to
cope with diagnosis and treatment
a) Verbalizes feelings
appropriately and recognizes nor-malcy of mood lability
b) Proceeds with treatment
in timely fashion
c) Discusses impact of
diagnosis and treatment on family and work
4) Demonstrates ability to
make decisions regarding treat-ment options in timely fashion
EXPECTED POSTOPERATIVE PATIENT OUTCOMES
Expected postoperative patient outcomes may include:
1) Reports that pain has
decreased and states pain and dis-comfort management strategies are effective
2) Exhibits clean, dry, and
intact surgical incisions without signs of inflammation or infection
3) Lists the signs and
symptoms of infection to be reported to the nurse or surgeon
4) Verbalizes feelings
regarding change in body image
5) Discusses meaning of the
diagnosis, surgical treatment, and fears (especially of death) appropriately
6) Participates actively in
self-care activities
a) Performs exercises as
prescribed
b) Participates in
self-care activities as prescribed
7) Recognizes that
postoperative sensations are normal and identifies management strategies
8) Discusses issues of
sexuality and resumption of sexual relations
9) Demonstrates knowledge
of postdischarge recommenda-tions and restrictions
a) Describes follow-up care
and activities
b) Demonstrates appropriate
care of incisions and drainage system
c) Demonstrates arm exercises
and describes exercise regimen and activity limitations during postoperative
period
d) Describes care of
affected arm and hand and lists indi-cations to contact the surgeon or nurse
10) Experiences no
complications
a) Identifies signs and
symptoms of reportable complica-tions (ie, redness, heat, pain, edema)
b) Describes side effects
of chemotherapy and strategies to cope with possible side effects
c) Explains how to contact
appropriate health care pro-viders in case of complications
Care
of the patient with breast cancer is summarized in the Plan of Nursing Care.
Related Topics