Chapter: Medical Surgical Nursing: Assessment and Management of Patients With Breast Disorders
Diagnostic Evaluation of Patients With Breast Disorders
Diagnostic Evaluation
BREAST SELF-EXAMINATION
BSE
instruction can be performed during assessment as part of the physical
examination; it can be taught in any setting, either to individuals or groups.
Instructions about BSE are provided to men if they have a family history of
breast cancer because these men may be at higher risk for male breast cancer.
Variations
in breast tissue occur during the menstrual cycle, pregnancy, and menopause.
Therefore, normal changes must be distinguished from those that may signal
disease. Most women notice increased tenderness and lumpiness before their
menstrual period; therefore, BSE is best performed after menses (day 5 to day
7, counting the first day of menses as day 1), when less fluid is retained.
Also, many women have grainy-textured breast tissue, but these areas are
usually less nodular after menses.
Because
women themselves detect many breast cancers, prior-ity is given to teaching all
women how and when to examine their breasts (Chart 48-2). It is estimated that
only 25% to 30% of women perform BSE proficiently and regularly each month.
Younger women, who have normal lumps in their breasts, find it particularly
difficult to perform BSE because they have a harder time distinguishing normal
from abnormal lumps and are not sure of what they are feeling due to the
density of their breast tissue. Even women who perform BSE may delay seeking
medical atten-tion because of fear, economic factors, lack of education,
reluctance to act if no pain is involved, psychological factors, and modesty.
Women
should begin practicing BSE at the time of their first gynecologic examination,
which usually occurs in their late teens or early 20s. All health care
providers, aware of these implica-tions, should encourage women to examine
their own breasts and teach them to recognize early changes that may indicate
prob-lems. The nurse plays a pivotal role in preventive education. Almost all
settings lend themselves to teaching, providing infor-mation, and encouraging
appropriate care for prevention, detec-tion, and treatment of breast problems.
An individual teaching session with the patient can increase the frequency with
which she practices BSE.
A
lesson in BSE should include the following: optimal timing for BSE (5 to 7 days
after menses begin for premenopausal women and once monthly for postmenopausal
women), a demonstration of examination techniques, a review of what normal
breast tissue feels like, a discussion on identification of breast changes, and
a return demonstration on the patient and a breast model. Patients who have had
breast surgery for the treatment of breast cancer are carefully instructed to
examine themselves for any nodules or changes in their breasts or along the
chest wall that may indicate a recurrence of the disease.
Films
or videos about BSE, shower cards, and pamphlets can be obtained from local c
hapters of the American Cancer Society. The National Cancer Institute in
Bethesda, Maryland, offers a program that teaches nurses to instruct patients
in BSE and also provides teaching aids. The National Alliance for Breast Cancer
Organizations, a clearinghouse for lay materials on breast cancer education, is
another resource.
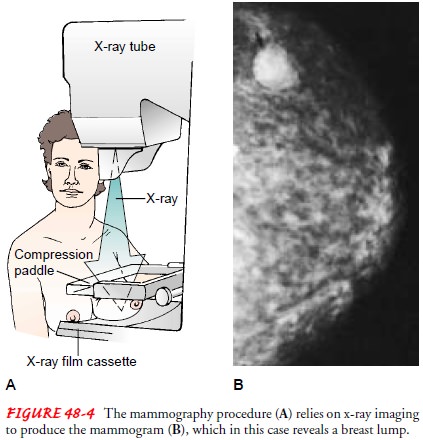
MAMMOGRAPHY
Mammography is a breast-imaging technique that can
detectnonpalpable lesions and assist in diagnosing palpable masses. The
procedure takes about 20 minutes and can be performed in an x-ray department or
independent imaging center. Two views are taken of each breast: a craniocaudal
view and a mediolateral oblique view. For these views, the breast is
mechanically com-pressed from top to bottom and side to side (Fig. 48-4). Women
may experience some fleeting discomfort because maximum compression is
necessary for proper visualization. The current mammograms are compared with
previous mammograms, and any changes indicate a need for further investigation.
Mammog-raphy may detect a breast tumor before it is clinically palpable (ie,
smaller than 1 cm); however, it has limitations and is not fool-proof. The false-negative
rate ranges between 5% and 10%; it is generally greater in younger women with
greater density of breast tissue. Some patients have very dense breast tissue,
making it dif-ficult to detect lesions with mammography.
Patients scheduled for a mammogram may voice concern about exposure to radiation. The radiation exposure is equivalent to about 1 hour of exposure to sunlight, so patients would have to have many mammograms in a year to increase their cancer risk.
The benefits of
this test outweigh the risks. Because the quality of mammography varies widely
from one setting to the next, it is important for women to find accredited
breast care centers that produce reliable mammograms.
Current
mammographic screening guidelines from the Amer-ican Cancer Society recommend a
mammogram every year start-ing at the age of 40 years. A baseline mammogram
should be obtained after the age of 35 years and by the age of 40. Younger
women who are identified as at a higher risk for breast cancer by family
history should seek the opinion of a breast specialist about when to begin
screening mammograms. Several studies suggest that screening for high-risk
women should begin about 10 years before the age of diagnosis of the family
member with breast can-cer (Hartmann, Sellers, Schaid et al., 1999). In
families with a history of breast cancer, a downward shift in age of diagnosis
of about 10 years is seen (eg, grandmother diagnosed with breast cancer at age
48, mother diagnosed with breast cancer at age 38, then daughter should begin
screening at age 28). Nurses need to provide teaching about screening
guidelines for women in the general population and those at high risk so that
these women can make informed choices about screening.
The
combination of screening mammography, physical ex-amination, and BSE has
reduced overall mortality from breast cancer by 63% among women ages 40 to 69
years (Tabar, Vitak, Tony et al., 2001). Despite the decreased mortality
associated with mammographic screening, it has not been used equitably across
the U.S. population. Current statistics indicate that 67% of women 40 years of
age and over have had a mammogram within the past 2 years (CDC Database, 2000).
Women with fewer resources (eg, elderly, poor, minority women, women with-out
health insurance) often do not have the means to undergo mammography or the
resources for follow-up treatment when le-sions are detected. Recent studies
have shown that social support contributes to adherence to mammographic
screening guidelines (Anderson, Urban & Etzioni, 1999; Faccione, 1999;
Lauver, Kane, Bodden et al., 1999). Many nurses direct their efforts at
educating women about the benefits of mammography. Work-ing to overcome
barriers to screening mammography, especially among the elderly and women with
disabilities, is an important nursing intervention in the community, and nurses
have an im-portant role in the development of educational materials targeted to
specific literacy levels and ethnic groups.
Galactography
Galactography is a mammographic diagnostic procedure that
in-volves injection of less than 1 mL of radiopaque material through a cannula
inserted into a ductal opening on the areola, followed by a mammogram. It is
performed when the patient has a bloody nipple discharge on expression,
spontaneous nipple discharge, or a solitary dilated duct noted on mammography.
These symptoms may indicate a benign lesion or a cancerous one.
ULTRASONOGRAPHY
Ultrasonography (ultrasound) is used in conjunction with
mam-mography to distinguish fluid-filled cysts from other lesions. A transducer
is used to transmit high-frequency sound waves through the skin and into the
breast, and an echo signal is measured. The echo waves are interpreted
electronically and then displayed on a screen. This technique is 95% to 99%
accurate in diagnosing cysts but does not definitively rule out a malignant
lesion.
For
women with dense breasts, the introduction of screening ultrasound examinations
has been researched during this past decade. The addition of ultrasonography to
breast cancer screen-ing can increase the sensitivity of screening for this
population of women, who tend to be either young or on hormone replacement
therapy. The largest study showed an increase in cancer detection by 17% with
the addition of screening ultrasonography (Kolb, Lichy & Newhouse, 1998).
Further research will help provide information on the usefulness of ultrasound
as a screening modality.
MAGNETIC RESONANCE IMAGING
Magnetic
resonance imaging (MRI) of the breast is a promising tool for use in diagnosing
breast conditions. It is a highly sensi-tive, although not specific, test and
serves as an adjunct to mam-mography. A coil is placed around the breast, and
the patient is placed inside the MRI machine for about 2 minutes. An injection
of gadolinium, a contrast dye, is given intravenously. MRI of the breast can be
helpful in determining the exact size of a lesion or the presence of multiple
foci more precisely than mammography. It also can determine more precisely than
a CT scan if a lesion is fixed to the chest wall. Other uses include
identifying occult (undetectable) breast cancer, determining the tumor’s
response to chemotherapy, and determining the integrity of saline or sili-cone
breast implants. The cost of breast MRI, however, is high; therefore, it is not
currently used for routine screening. However, the sensitivity of the MRI may
be beneficial for cancer detection in higher-risk women, and the results from
preliminary studies are encouraging (Schnall, 2001).
PROCEDURES FOR TISSUE ANALYSIS
Fine-Needle Aspiration
Fine-needle aspiration (FNA) is an outpatient procedure usu-ally
initiated when mammography, ultrasonography, or palpa-tion detects a lesion. A
surgeon performs the procedure when there is a palpable lesion, or a
radiologist performs it under x-ray guidance for nonpalpable lesions. Injection
of a local anesthetic may or may not be used, but most times the surgeon or
radiol-ogist inserts a 21- or 22-gauge needle attached to a syringe into the
site to be sampled. The syringe is then used to withdraw tis-sue or fluid into
the needle. This cytologic material is spread on a slide and sent to the
laboratory for analysis. FNA is less expen-sive than other diagnostic methods,
and results are usually avail-able quickly; however, this diagnostic test is
often not 100% accurate, and the false-negative rate is substantial.
False-negative or false-positive results are possible, and clinical follow-up
depends on the level of suspicion about the breast lesion.
Stereotactic Biopsy
Stereotactic biopsy, also an outpatient procedure, is
performedfor nonpalpable lesions found on mammography. The patient lies prone
on a special table, and the breast is positioned through an opening in the
table and compressed for a mammogram. The lesion to be sampled is then located
with the aid of a computer. Next, a local anesthetic is injected into the entry
site on the breast, a core needle is inserted, and samples of the tissue are
taken for pathologic examination. If the lesion is small, a clip is placed at
the site of the biopsy, so that a specific area can be visualized again as
another mammogram is performed. This technique allows accurate diagnosis and
often allows the patient to avoid a surgical biopsy, although some patients may
end up needing a surgical biopsy, depending on the pathologic diagnosis.
Surgical Biopsy
Surgical biopsy is the most common outpatient surgical
proce-dure. Eight of 10 lesions are benign on biopsy. The procedure is usually
done using local anesthesia, moderate sedation, or both. The biopsy involves
excising the lesion and sending it to the lab-oratory for pathologic
examination.
EXCISIONAL BIOPSY
Excisional
biopsy is the usual procedure for any palpable breast mass. The entire lesion,
plus a margin of surrounding tissue, is re-moved. This type of biopsy may also
be referred to as a lumpec-tomy. Depending on the clinical situation, a frozen
section may be done at the time of the biopsy (a small piece of the mass or
le-sion is given a provisional diagnosis by the pathologist), so that the
surgeon can provide the patient with a diagnosis in the re-covery room.
INCISIONAL BIOPSY
Incisional
biopsy is performed when tissue sampling alone is re-quired; this is done both
to confirm a diagnosis and to determine the hormonal receptor status. Complete
excision of the area may not be possible or immediately beneficial to the
patient, depend-ing on the clinical situation. This procedure is often
performed in women with locally advanced breast cancer or in cancer pa-tients with
a suspicion of recurrent disease, whose treatment may depend on the tumor’s
estrogen and progesterone receptor status. These receptors are identified
during pathologic examination of the tissue.
TRU-CUT CORE BIOPSY
In a
Tru-Cut core biopsy, the surgeon uses a special large-lumen needle to remove a
core of tissue. This procedure is used when a tumor is relatively large and
close to the skin surface and the sur-geon strongly suspects that the lesion is
a carcinoma. If cancer is diagnosed, the tissue is also tested for hormone
receptor status.
WIRE NEEDLE LOCALIZATION
Wire needle localization is a technique used when
mammogra-phy detects minute, pinpoint calcifications (indicating a poten-tial
malignancy) or nonpalpable lesions and a biopsy is necessary. A long, thin wire
is inserted, usually painlessly, through a needle before the excisional biopsy
under mammographic guidance to ensure that the wire tip designates the area to
undergo biopsy. The wire remains in place after the needle is withdrawn to ensure
a precise biopsy. The patient is then taken to the operating room, where the
surgeon follows the wire down and excises the area around the wire tip. The
tissue removed is x-rayed at the time of the procedure; these specimen x-rays,
along with follow-up mammograms taken several weeks later (after the site has
healed), verify that the area of concern was located and removed.
Related Topics