Chapter: Medical Surgical Nursing: Assessment and Management of Patients With Hearing and Balance Disorders
Nursing Process: The Patient Undergoing Mastoid Surgery
NURSING PROCESS: THE PATIENT
UNDERGOING MASTOID SURGERY
Although
several otologic surgical procedures are performed under moderate sedation,
mastoid surgery is performed using general anesthesia.
Assessment
The
health history includes a complete description of the ear problem, including
infection, otalgia, otorrhea, hearing loss, and vertigo. Data are collected
about the duration and intensity of the problem, its causes, and previous
treatments. Information is ob-tained about other health problems and all
medications that the patient is taking. Medication allergies and family history
of ear disease also should be obtained.
Physical assessment includes observation for
erythema, edema, otorrhea, lesions, and characteristics such as odor and color
of dis-charge. The results of the audiogram should be reviewed.
Nursing Diagnoses
Based
on the assessment data, the patient’s major nursing diag-noses may include the
following:
·
Anxiety related to surgical
procedure, potential loss of hear-ing, potential taste disturbance, and
potential loss of facial movement
·
Acute pain related to mastoid
surgery
·
Risk for infection related to
mastoidectomy, placement of grafts, prostheses, electrodes, and surgical trauma
to sur-rounding tissues and structures
·
Disturbed auditory sensory
perception related to ear dis-order, surgery, or packing
·
Risk for trauma related to
balance difficulties or vertigo dur-ing the immediate postoperative period
·
Disturbed sensory perception
related to potential damage to facial nerve (cranial nerve VII) and chorda
tympani nerve
·
Impaired skin integrity
related to ear surgery, incisions, and graft sites
·
Deficient knowledge about
mastoid disease, surgical proce-dure, and postoperative care and expectations
Planning and Goals
The
major goals of caring for a patient undergoing mastoidec-tomy include reduction
of anxiety; freedom from pain and dis-comfort; prevention of infection; stable
or improved hearing and communication; absence of injury from vertigo; absence
of or ad-justment to sensory or perceptual alterations; return of skin
in-tegrity; and increased knowledge regarding the disease, surgical procedure,
and postoperative care.
Nursing Interventions
REDUCING ANXIETY
Information that the otologic surgeon has discussed
with the pa-tient, including anesthesia, the location of the incision
(post-auricular), and expected surgical results (eg, hearing, balance, taste,
facial movement), is reinforced. The patient also is encour-aged to discuss any
anxieties and concerns about the surgery.
RELIEVING PAIN
Although most patients complain very little about
incisional pain after mastoid surgery, they do have some ear discomfort. Aural
fullness or pressure after surgery is caused by residual blood or fluid in the
middle ear. The prescribed analgesic may be taken for the first 24 hours after
surgery and then only as needed. The pa-tient is instructed in the use of and
side effects of the medication.
A tympanoplasty may also be performed at the time
of the mastoidectomy. A wick or external auditory canal packing is used after a
tympanoplasty to stabilize the tympanic membrane. Pa-tients should be informed
that they may experience intermittent sharp, shooting pains in the ear for 2 to
3 weeks after surgery as the eustachian tube opens and allows air to enter the
middle ear.
PREVENTING INFECTION
Measures
are initiated to prevent infection in the operated ear. The external auditory
canal wick, or packing, may be impreg-nated with an antibiotic solution before
instillation. Prophylac-tic antibiotics are administered as prescribed, and the
patient is instructed to prevent water from entering the external auditory
canal for 6 weeks. A cotton ball or lamb’s wool covered with a water-insoluble
substance (eg, petroleum jelly) and placed loosely in the ear canal usually
prevents water contamination. The post-auricular incision should be kept dry
for 2 days. Signs of infec-tion such as an elevated temperature and purulent
drainage are reported. Some serosanguineous drainage from the external
audi-tory canal is normal after surgery.
IMPROVING HEARING AND COMMUNICATION
Hearing in the operated ear may be reduced for
several weeks be-cause of edema, accumulation of blood and tissue fluid in the
mid-dle ear, and dressings or packing. Measures are initiated to improve
hearing and communication, such as reducing environ-mental noise, facing the
patient when speaking, speaking clearly and distinctly without shouting,
providing good lighting if the pa-tient relies on speech reading, and using nonverbal
clues (eg, facial expression, pointing, gestures) and other forms of
communica-tion. Family members or significant others are instructed about
ef-fective ways to communicate with the patient. If the patient uses assistive
hearing devices, one can be used in the unaffected ear.
PREVENTING INJURY
Vertigo may occur after mastoid surgery if the
semicircular canals or other areas of the inner ear are traumatized. This symptom
is relatively uncommon after this type of ear surgery and usually is temporary.
Antiemetics or antivertiginous medica-tions (eg, antihistamines) can be
prescribed if a balance distur-bance or vertigo occurs. The patient should be
instructed about the expected effects and potential side effects. Safety
measures such as assisted ambulation are implemented to prevent falls. Safety
measures must also be implemented at home to prevent falls and injury.
PREVENTING ALTERED SENSORY PERCEPTION
Facial nerve injury is a potential, although rare,
complication of mastoid surgery. The patient is instructed to report
immediately any evidence of facial nerve (cranial nerve VII) weakness, such as
drooping of the mouth on the operated side. A more frequent oc-currence is a
temporary disturbance in the chorda tympani nerve, a small branch of the facial
nerve that runs through the middle ear. Patients experience a taste disturbance
and dry mouth on the side of surgery for several months until the nerve
regenerates.
PROMOTING WOUND HEALING
The
patient is instructed to avoid heavy lifting, straining, exer-tion, and nose
blowing for 2 to 3 weeks after surgery to prevent dislodging the tympanic
membrane graft or ossicular prosthesis.
INCREASING KNOWLEDGE
The
patient is informed about the surgery and operating room environment.
Discussing postoperative expectations helps to de-crease anxiety about the
unknown. Because postoperative in-structions for mastoid surgery vary among
otologic surgeons, it is important for the nurse to be aware of the surgeon’s
preferences when teaching the patient.
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care
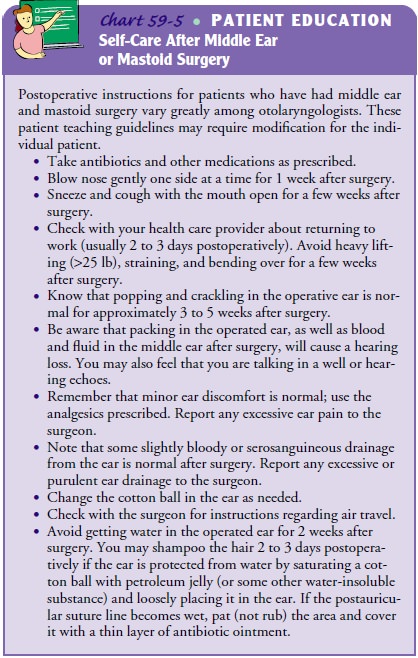
Patients require instruction about prescribed
medication therapy, such as analgesics, antivertiginous agents, and
antihistamines pre-scribed for balance disturbance. Teaching includes
information about the expected effects and potential side effects of the
medica-tion. Patients also need instruction about any activity restrictions.
Possible complications such as infection, facial nerve weakness, or taste
disturbances, including the signs and symptoms to report immediately, should be
addressed (see Chart 59-5).
Continuing Care
Some
patients, particularly elderly patients, who have had mas-toid surgery may
require the services of a home care nurse for a few days after returning home.
However, most people find that assistance from a family member or a friend is
sufficient. The care-giver and patient are cautioned that the patient may
experience some vertigo and will therefore require help with ambulation to
avoid falling. Any symptoms of complications are to be reported promptly to the
surgeon. The importance of scheduling and keeping follow-up appointments is
also stressed.
Evaluation
EXPECTED PATIENT OUTCOMES
Expected
patient outcomes may include:
1) Demonstrates
reduced anxiety about surgical procedure
a) Verbalizes
and exhibits less stress, tension, and irritability
b) Verbalizes acceptance of the results of surgery and ad-justment to possible hearing impairment
2) Remains
free of discomfort or pain
i) Exhibits
no facial grimacing, moaning, or crying, and reports absence of pain
ii) Uses
analgesics appropriately
3) Demonstrates
no signs or symptoms of infection
i) Has
normal vital signs, including temperature
ii) Demonstrates
absence of purulent drainage from the external auditory canal
iii) Describes
method for preventing water from contami-nating packing
4) Exhibits
signs that hearing has stabilized or improved
i) Describes
surgical goal for hearing and judges whether the goal has been met
ii) Verbalizes
that hearing has improved
5) Remains
free of injury and trauma because of vertigo
i) Reports
absence of vertigo or balance disturbance
ii) Experiences
no injury or fall
iii) Modifies
environment to avoid falls (eg, night light, no clutter on stairs)
6) Adjusts
to or remains free from altered sensory perception
i) Reports
no taste disturbance, mouth dryness, or facial weakness
7) Demonstrates
no skin breakdown
i) Lists
ways to prevent dislodging graft or prosthesis
8) Is
aware of limitations in activities (eg, bathing, lifting, air travel) and for
how long Verbalizes the reasons for and methods of care and treatment
a) Shares
knowledge with family about treatment protocol
b) Describes
treatment and the time frame for the recov-ery phase
c) Discusses
the discharge plan formulated with the nurse with regard to rest periods,
medication, and activities permitted and restricted
d) Lists
symptoms that should be reported to health care personnel
e) Keeps
follow-up appointments
Related Topics