Chapter: Medical Surgical Nursing: Assessment and Management of Patients With Hearing and Balance Disorders
Conditions of the Inner Ear
Conditions of the Inner Ear
Disorders of balance and the vestibular system
involving the inner ear afflict more than 30 million Americans 17 years of age
or older. Falls resulting from these disorders account for more than 100,000
hip fractures in elderly people each year (NIDCD, 1998).
The term dizziness
is used frequently by patients and health care providers to describe any
altered sensation of orientation in space. Vertigo
is defined as the misperception or illusion of mo-tion of the person or the
surroundings. Most people with vertigo describe a spinning sensation or say
they feel as though objects are moving around them. Ataxia is a failure of muscular
coordination and may be present in patients with vestibular disease. Syncope,
fainting, and loss of consciousness are not forms of vertigo, nor are they
characteristic of an ear problem; they usually indicate dis-ease in the
cardiovascular system.
Nystagmus is
an involuntary rhythmic movement of the eyes.Nystagmus occurs normally when a
person watches a rapidly moving object (eg, through the side window of a moving
car or train). However, pathologically it is an ocular disorder associated with
vestibular dysfunction. Nystagmus can be horizontal, verti-cal, or rotary and
can be caused by a disorder in the central or peripheral nervous system.
MOTION SICKNESS
Motion sickness is a disturbance of equilibrium
caused by constant motion. For example, it can occur aboard a ship, while
riding on a merry-go-round or swing, or in the back seat of a car.
Clinical Manifestations
The syndrome manifests itself in sweating, pallor,
nausea, and vomiting caused by vestibular overstimulation. These
manifesta-tions may persist for several hours after the stimulation stops.
Management
Over-the-counter
antihistamines used to treat vertigo, such as di-menhydrinate (Dramamine) or
meclizine hydrochloride (Bonine), provide some relief. Anticholinergic
medications, such as scopo-lamine patches, may be helpful. These must be
replaced every few days. Side effects such as dry mouth and drowsiness occur
with these medications, which may prove to be more troublesome than helpful.
Potentially hazardous activities such as driving a car or operating heavy
machinery should be avoided if the patient experiences drowsiness.
MÉNIÈRE’S DISEASE
Ménière’s disease is an abnormal inner ear fluid
balance caused by a malabsorption in the endolymphatic sac. Evidence indicates
that many people with Ménière’s disease may have a blockage in the
endolymphatic duct. Regardless of the cause, endolymphatichydrops, a dilation in the endolymphatic space,
develops. Eitherincreased pressure in the system or rupture of the inner ear
mem-branes occurs, producing symptoms of Ménière’s disease.
Ménière’s disease affects more than 2.4 million
people in the United States. More common in adults, it has an average age of
onset in the 40s, with symptoms usually beginning between the ages of 20 and 60
years. However, the disease has been reported in children as young as age 4
years and in adults up to the 90s. Ménière’s disease appears to be equally
common in both genders. The right and left ears are affected with equal
frequency; the dis-ease occurs bilaterally in about 20% of patients. About 20%
of the patients have a positive family history for the disease (Knox &
McPherson, 1997).
Clinical Manifestations
Ménière’s
disease involves the following symptoms: fluctuating, progressive sensorineural
hearing loss; tinnitus or a roaring
sound; a feeling of pressure or fullness in the ear; and episodic,
incapac-itating vertigo, often accompanied by nausea and vomiting. The effects
of these symptoms range from a minor nuisance to ex-treme disability,
especially if the attacks of vertigo are severe. At the onset of the disease,
perhaps only one or two of the symptoms are manifested.
Some
clinicians believe that there are two subsets of the dis-ease, known as
atypical Ménière’s disease: cochlear and vestibu-lar. Cochlear Ménière’s disease
is recognized as a fluctuating, progressive sensorineural hearing loss
associated with tinnitus and aural pressure in the absence of vestibular
symptoms or findings. Vestibular Ménière’s disease is characterized as the
occurrence of episodic vertigo associated with aural pressure but no cochlear
symptoms. In some patients, cochlear or vestibular Ménière’s dis-ease develops
first. In most patients, however, all of the symptoms develop eventually.
Assessment and Diagnostic Findings
Vertigo is usually the most troublesome complaint.
A careful his-tory is taken to determine the frequency, duration, severity, and
character of the vertigo attacks. Typically, the patient reports that vertigo
lasts minutes to hours, possibly accompanied by nausea or vomiting. Patients
also complain of diaphoresis and a persis-tent feeling of imbalance or
disequilibrium, which may last for days. They may complain of attacks that
awaken them at night. Between attacks, however, they usually feel well. The
hearing loss may fluctuate, with tinnitus and aural pressure waxing and waning
with changes in hearing. The tinnitus and feeling of aural pressure may occur
only during or before attacks, or they may be constant.
Findings
of the physical examination are usually normal, with the exception of the
evaluation of cranial nerve VIII. Sounds from a tuning fork (ie, Weber test)
may lateralize to the ear opposite the hearing loss, the one affected with
Ménière’s disease. An audiogram typically reveals a sensorineural hearing loss
in the af-fected ear. This can be in the form of a “Pike’s Peak” pattern, which
looks like a hill or mountain, or it may show a sensori-neural loss in the low
frequencies. As the disease progresses, the hearing loss increases. The
electronystagmogram may be normal or may show reduced vestibular response.
There is, however, no absolute diagnostic test.
Medical Management
Most
patients with Ménière’s disease can be successfully treated with diet and
medication therapy. Many patients can control their symptoms by adhering to a
low-sodium (2,000 mg/day) diet. The amount of sodium is one of many factors
that regulate the balance of fluid within the body. Sodium and fluid retention
disrupts the delicate balance between endolymph and perilymph in the inner ear.
Psychological evaluation may be indicated if the patient is anxious, uncertain,
fearful, or depressed.
PHARMACOLOGIC THERAPY
Pharmacologic
therapy for Ménière’s disease consists of anti-histamines such as meclizine
(Antivert), which suppress the ves-tibular system. Tranquilizers such as
diazepam (Valium) may be used in acute instances to help control vertigo.
Antiemetics such as promethazine (Phenergan) suppositories help control the
nau-sea and vomiting and the vertigo because of their antihistamine effect.
Diuretic therapy (eg, hydrochlorothiazide) sometimes re-lieves symptoms by
lowering the pressure in the endolymphatic system. Intake of foods containing
potassium (eg, bananas, toma-toes, oranges) is necessary if the patient takes a
diuretic that causes potassium loss.
Vasodilators, such as nicotinic acid, papaverine
hydrochloride (Pavabid), and methantheline bromide (Banthine), have no
sci-entific basis for alleviating the symptoms, but they are often used in
conjunction with other therapies.
SURGICAL MANAGEMENT
Although
most patients respond well to conservative therapy, some continue to have
disabling attacks of vertigo. If these attacks reduce their quality of life,
patients may elect to undergo surgery for relief. However, hearing loss,
tinnitus, and aural fullness may continue, because the surgical treatment of
Ménière’s disease is aimed at eliminating the attacks of vertigo.
Endolymphatic Sac
Decompression.Endolymphatic sac
decom-pression, or shunting, theoretically equalizes the pressure in the
endolymphatic space. A shunt or drain is inserted in the en-dolymphatic sac
through a postauricular incision. This procedure is favored by many
otolaryngologists as a first-line surgical ap-proach to treat the vertigo of
Ménière’s disease because it is rela-tively simple and safe and can be
performed on an outpatient basis.
Middle and Inner Ear
Perfusion.Ototoxic medications,
such asstreptomycin or gentamicin, can be given to patients by infusion into
the middle and inner ear. These medications are used to de-crease vestibular
function and decrease vertigo. The success rate for eliminating vertigo is
high, about 85%, but the risk of signif-icant hearing loss is also high. This
procedure of inner ear perfu-sion usually requires an overnight stay in the
hospital. After the procedure, many patients have a period of imbalance that
lasts several weeks.
Intraotologic Catheters.In an attempt to deliver medication di-rectly to
the inner ear, catheters are being developed to provide a conduit from the
outer ear to the inner ear. The route of the catheter is from the external ear
canal through or around the tym-panic membrane and to the round window niche or
membrane. Medicinal fluids can be placed against the round window for a direct
route to the inner ear fluids.
Potential
uses of these catheters include treatment for sudden hearing loss and various
disorders causing intractable vertigo. Fu-ture applications may include
tinnitus and slowly progressing sensorineural hearing loss. Intratympanic
injections of ototoxic medications for round window membrane diffusion can be
used to decrease vestibular function. Established surgical techniques can be
used for the patient with vertigo who has not responded to medical or physical
therapeutic modalities.
Vestibular Nerve Section.Vestibular nerve section provides thegreatest success rate (approximately
98%) in eliminating the at-tacks of vertigo. It can be performed by a
translabyrinthine ap-proach (ie, through the hearing mechanism) or in a manner
that can conserve hearing (ie, suboccipital or middle cranial fossa), depending
on the degree of hearing loss. Most patients with in-capacitating Ménière’s
disease have little or no effective hearing. Cutting the nerve prevents the
brain from receiving input from the semicircular canals. This procedure
requires a brief hospital stay. Nursing care for the patient with vertigo is
presented in Plan of Nursing Care 59-1.
LABYRINTHITIS
Labyrinthitis,
an inflammation of the inner ear, can be bacterialor viral in origin. Although
rare because of antibiotic therapy, bacterial labyrinthitis usually occurs as a
complication of otitis media. The infection can enter the inner ear by
penetrating the membranes of the oval or round windows. Viral labyrinthitis is
a common medical diagnosis, but little is known about this dis-order, which
affects hearing and balance. The most commonly identified viral causes are
mumps, rubella, rubeola, and influenza. Viral illnesses of the upper
respiratory tract and herpetiform dis-orders of the facial and acoustic nerves
(ie, Ramsay Hunt syn-drome) also cause labyrinthitis.
Clinical Manifestations
Labyrinthitis
is characterized by a sudden onset of incapacitating vertigo, usually with
nausea and vomiting, various degrees of hearing loss, and possibly tinnitus.
The first episode is usually the worst; subsequent attacks, which usually occur
over a period of several weeks to months, are less severe.
Management
Treatment of bacterial labyrinthitis includes
intravenous antibiotic therapy, fluid replacement, and administration of a
vestibular sup-pressant, such as meclizine, and antiemetic medications.
Treat-ment of viral labyrinthitis is tailored to the patient’s symptoms.
BENIGN PAROXYSMAL POSITIONAL VERTIGO
Benign paroxysmal positional vertigo (BPPV) is a
brief period of incapacitating vertigo that occurs when the position of the
pa-tient’s head is changed with respect to gravity, typically by plac-ing the
head back with the affected ear turned down. The onset is sudden and followed
by a predisposition for positional vertigo, usually for hours to weeks but
occasionally for months or years.
It is speculated to be caused by the disruption of
debris within the semicircular canal. This debris is formed from small crystals
of calcium carbonate from the inner ear structure, the utricle. This is
frequently stimulated by head trauma, infection, or other events. In severe
cases, vertigo may easily be induced by any head movement. The vertigo is
usually accompanied by nausea and vomiting; how-ever, hearing impairment does
not generally occur (Hain, 2002).
Bed rest is recommended for patients with acute
symptoms. Canalith repositioning procedures (CRP) may be used to provide
resolution of vertigo. The Epley procedure is a repositioning tech-nique that
is safe, inexpensive, and easy to perform for these patients. However, this
procedure is not recommended for patients with acute vertigo or for patients
diagnosed with vestibular neuronitis (a paroxysmal attack of severe vertigo).
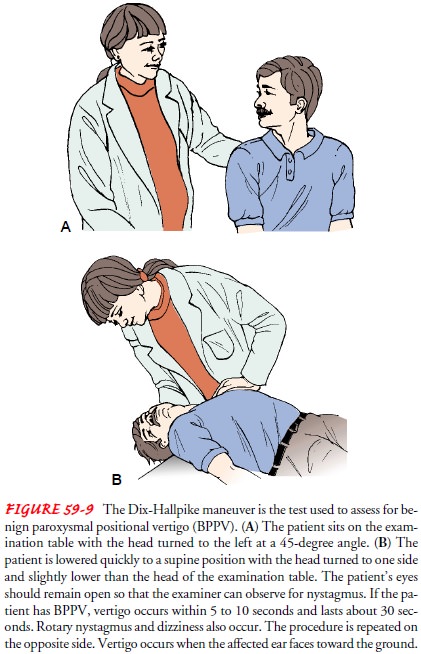
Patients with acute vertigo may be medicated with
meclizine for 1 to 2 weeks. After this time, the meclizine is stopped and the
patient is reassessed. Patients who continue to have severe posi-tional vertigo
may be premedicated with prochloperazine (Com-pazine) 1 hour before performing
the CRP. The Dix-Hallpike test is used to assess for BPPV. When the
Dix-Hallpike test results are positive on the right side, a left-sided CRP is
used (Fig. 59-9).
Vestibular
rehabilitation can be used in the management of vestibular disorders. This
strategy promotes active use of the vestibular system through a
multidisciplinary team approach, in-cluding medical and nursing care, stress
management, biofeed-back, vocational rehabilitation, and physical therapy. A
physical therapist prescribes balance exercises that help the brain com-pensate
for the impairment to the balance system.
OTOTOXICITY
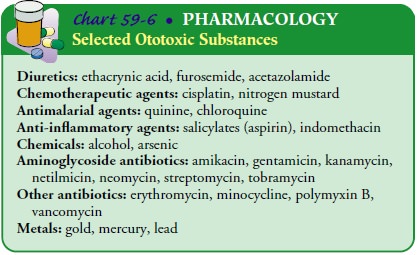
A
variety of medications may have adverse effects on the cochlea, vestibular
apparatus, or cranial nerve VIII. All but a few, such as aspirin and quinine,
cause irreversible hearing loss. At high doses, aspirin toxicity also can
produce tinnitus. Intravenous medica-tions, especially the aminoglycosides, are
the most common cause of ototoxicity, and they destroy the hair cells in the
organ of Corti (see Chart 59-6).
To
prevent loss of hearing or balance, patients receiving po-tentially ototoxic
medications should be counseled about the side effects of these medications.
Blood levels of the medications should be monitored and patients receiving
long-term intra-venous antibiotics should be monitored with an audiogram twice
each week during therapy.
ACOUSTIC NEUROMA
An acoustic neuroma is a slow-growing, benign tumor of cranial nerve VIII, usually arising from the Schwann cells of the vestibu-lar portion of the nerve. Most acoustic tumors arise within the in-ternal auditory canal and extend into the cerebellopontine angle to press on the brain stem. Acoustic neuromas account for 5% to 10% of all intracranial tumors and seem to occur with equal fre-quency in men and women at any age, although most occur during middle age. Most acoustic neuromas are unilateral, except in von Recklinghausen’s disease (ie, neurofibromatosis type 2), in which bilateral tumors occur.
Assessment and Diagnostic Findings
The most common findings of assessment of patients with an acoustic neuroma are unilateral tinnitus and hearing loss with or without vertigo or balance disturbance. It is important to iden-tify asymmetry in audiovestibular test results so that further workup can be performed to rule out an acoustic neuroma.
MRI with a paramagnetic contrast agent (ie, gadolinium or Magnevist)
is the imaging study of choice. If the patient is claustrophobic or cannot
tolerate an MRI or if the scan is unavailable, a computed tomography (CT) scan
with contrast dye is performed. However, MRI is more sensitive in delineating a
small tumor than is CT.
Management
Surgical removal of acoustic tumors is the
treatment of choice be-cause these tumors do not respond well to irradiation or
chemo-therapy. Because treatment of acoustic tumors crosses several
specialties, the multidisciplinary treatment approach involves a neurotologist
and a neurosurgeon. The objective of the surgery is to remove the tumor while
preserving facial nerve function. Most acoustic tumors have damaged the
cochlear portion of cranial nerve VIII, and no serviceable hearing exists before
surgery. In these patients, the surgery is performed using a translabyrinthine
approach, and the hearing mechanism is destroyed. If hearing is still good
before surgery, a suboccipital or middle cranial fossa ap-proach to removing
the tumor may be used, and intraoperative monitoring of cranial nerve VIII is
performed to save the hearing.
Complications
of surgery for acoustic neuroma include facial nerve paralysis, cerebrospinal
fluid leak, meningitis, and cerebral edema. Death from acoustic neuroma surgery
is rare.
Related Topics