Chapter: Medical Surgical Nursing: Assessment and Management of Patients With Hearing and Balance Disorders
Conditions of the Middle Ear
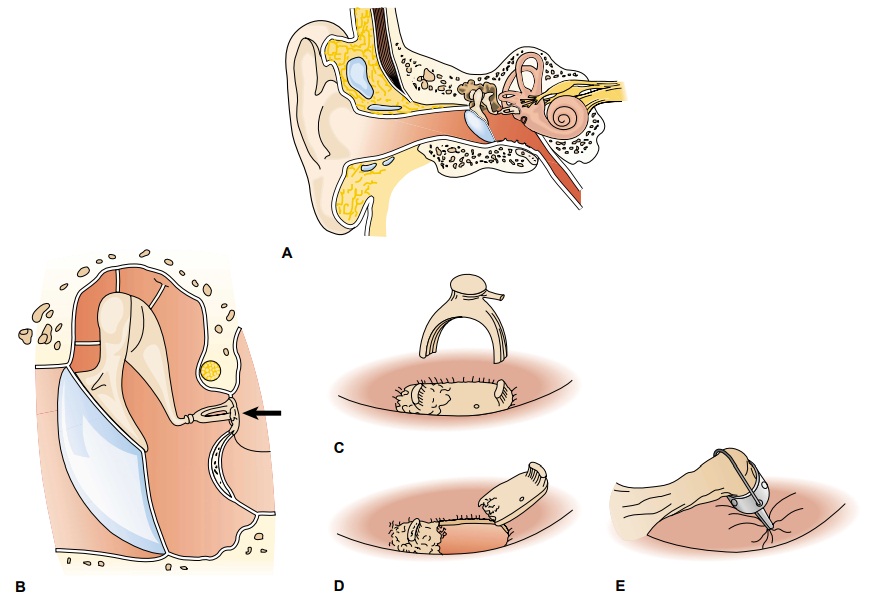
Conditions of the Middle Ear
TYMPANIC MEMBRANE PERFORATION
Perforation of the tympanic membrane is usually
caused by infec-tion or trauma. Sources of trauma include skull fracture,
explosive injury, or a severe blow to the ear. Less frequently, perforation is
caused by foreign objects (eg, cotton-tipped applicators, bobby pins, keys)
that have been pushed too far into the external audi-tory canal. In addition to
tympanic membrane perforation, injury to the ossicles and even the inner ear
may result from this type ofaction. Attempts by patients
to clear the external auditory canal should be discouraged. During infection,
the tympanic membrane can rupture if the pressure in the middle ear exceeds the
atmo-spheric pressure in the external auditory canal.
Medical Management
Although most tympanic membrane perforations heal
sponta-neously within weeks after rupture, some may take several months to
heal. Some perforations persist because scar tissue grows over the edges of the
perforation, preventing extension of the epithe-lial cells across the margins
and final healing. In the case of a head injury or temporal bone fracture, a
patient is observed for evi-dence of cerebrospinal fluid otorrhea or rhinorrhea—a
clear, watery drainage from the ear or nose, respectively. While healing, the
ear must be protected from water.
SURGICAL MANAGEMENT
Perforations
that do not heal on their own may require surgery. The decision to perform a tympanoplasty (ie, surgical repair of
the tympanic membrane) is usually based on the need to prevent potential
infection from water entering the ear or the desire to im-prove the patient’s
hearing. Performed on an outpatient basis, tympanoplasty may involve a variety
of surgical techniques. In all techniques, tissue is placed across the
perforation to allow heal-ing. Surgery is usually successful in closing the
perforation per-manently and improving hearing.
ACUTE OTITIS MEDIA
Acute otitis media is
an acute infection of the middle ear, usu-ally lasting less than 6 weeks. The
primary cause of acute otitis media is usually Streptococcus pneumoniae, Haemophilus influen-zae, and Moraxella catarrhalis, which enter the
middle ear aftereustachian tube dysfunction caused by obstruction related to
upper respiratory infections, inflammation of surrounding struc-tures (eg,
sinusitis, adenoid hypertrophy), or allergic reactions (eg, allergic rhinitis).
Bacteria can enter the eustachian tube from contaminated secretions in the
nasopharynx and the middle ear from a tympanic membrane perforation. A purulent
exudate is usually present in the middle ear, resulting in a conductive
hear-ing loss.
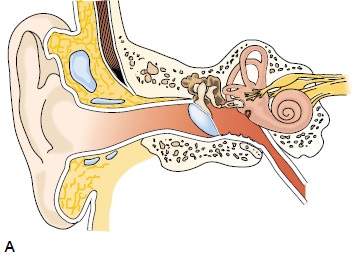
Clinical Manifestations
The
symptoms of otitis media vary with the severity of the in-fection. The
condition, usually unilateral in adults, may be ac-companied by otalgia. The
pain is relieved after spontaneous perforation or therapeutic incision of the
tympanic membrane. Other symptoms may include drainage from the ear, fever, and
hearing loss. On otoscopic examination, the external auditory canal appears
normal. The patient reports no pain with move-ment of the auricle. The tympanic
membrane is erythematous and often bulging. Table 59-3 differentiates acute
external otitis from acute otitis media.
Medical Management
The outcome of acute otitis media depends on the efficacy of ther-apy (ie, the prescribed dose of an oral antibiotic and the duration of therapy), the virulence of the bacteria, and the physical status of the patient. With early and appropriate broad-spectrum anti-biotic therapy, otitis media may resolve with no serious sequelae.
If drainage occurs, an antibiotic otic preparation
is usually pre-scribed. The condition may become subacute (lasting 3 weeks to 3
months), with persistent purulent discharge from the ear. Rarely does permanent
hearing loss occur. Secondary complications in-volving the mastoid and other
serious intracranial complications, such as meningitis or brain abscess,
although rare, can occur.
SURGICAL MANAGEMENT
An
incision in the tympanic membrane is known as myringot-omy or tympanotomy.
The tympanic membrane is numbedwith a local anesthetic such as phenol or by
iontophoresis (ie, electrical current flows through a lidocaine-and-epinephrine
solution to numb the ear canal and tympanic membrane). The procedure is
painless and takes less than 15 minutes. Under mi-croscopic guidance, an
incision is made through the tympanic membrane to relieve pressure and to drain
serous or purulent fluid from the middle ear.
Normally,
this procedure is unnecessary for treating acute oti-tis media, but it may be
performed if pain persists. Myringotomy also allows the drainage to be analyzed
(by culture and sensitivity testing) so that the infecting organism can be
identified and ap-propriate antibiotic therapy prescribed. The incision heals
within 24 to 72 hours.
If
episodes of acute otitis media recur and there is no con-traindication, a
ventilating, or pressure-equalizing, tube may be inserted. The ventilating
tube, which temporarily takes the place of the eustachian tube in equalizing pressure,
is retained for 6 to 18 months. The ventilating tube is then extruded with
normal skin migration of the tympanic membrane, with the hole healing in nearly
every case. Ventilating tubes are more commonly used to treat recurrent
episodes of acute otitis media in children than in adults.
SEROUS OTITIS MEDIA
Serous otitis media (ie, middle ear effusion) implies fluid, with-out evidence of active
infection, in the middle ear. In theory, this fluid results from a negative
pressure in the middle ear caused by eustachian tube obstruction. This
condition is found primarily in children. When it occurs in adults, an
underlying cause for the eustachian tube dysfunction must be sought. Middle ear
effusion is frequently seen in patients after radiation therapy or baro-trauma
and in patients with eustachian tube dysfunction from a concurrent upper
respiratory infection or allergy. Barotrauma re-sults from sudden pressure
changes in the middle ear caused by changes in barometric pressure, as in scuba
diving or airplane de-scent. A carcinoma (eg, nasopharyngeal cancer)
obstructing theeustachian tube should be ruled out in an adult with persistent
unilateral serous otitis media.
Clinical Manifestations
Patients
may complain of hearing loss, fullness in the ear or a sen-sation of
congestion, and perhaps even popping and crackling noises, which occur as the
eustachian tube attempts to open. The tympanic membrane appears dull on
otoscopy, and air bubbles may be visualized in the middle ear. Usually, the
audiogram shows a conductive hearing loss.
Management
Serous
otitis media need not be treated medically unless infection occurs (ie, acute
otitis media). If the hearing loss associated with middle ear effusion is a
problem for the patient, a myringotomy can be performed, and a tube may be
placed to keep the middle ear ventilated. Corticosteroids in small doses
sometimes decrease the edema of the eustachian tube in cases of barotrauma.
Decon-gestants have not proved effective. A Valsalva maneuver, which forcibly
opens the eustachian tube by increasing nasopharyngeal pressure, may be
cautiously performed. Performing the Valsalva maneuver may cause worsening pain
or perforation of the tym-panic membrane.
CHRONIC OTITIS MEDIA
Chronic otitis media is
the result of repeated episodes of acute oti-tis media causing irreversible
tissue pathology and persistent per-foration of the tympanic membrane. Chronic
infections of the middle ear damage the tympanic membrane, destroy the
ossicles, and involve the mastoid. Before the discovery of antibiotics,
infec-tions of the mastoid were life-threatening. The use of medications in
acute otitis media has made acute mastoiditis a rare condition in developed
countries.
Clinical Manifestations
Symptoms may be minimal, with varying degrees of
hearing loss and the presence of a persistent or intermittent, foul-smelling
otor-rhea. Pain is not usually experienced, except in cases of acute
mas-toiditis, when the postauricular area is tender to the touch and may be
erythematous and edematous. Otoscopic evaluation of the tympanic membrane may
show a perforation, and cholesteatoma can be identified as a white mass behind
the tympanic membrane or coming through to the external canal from a
perforation.
Cholesteatoma
is an ingrowth of the
skin of the external layerof the eardrum into the middle ear. It is generally
caused by a chronic retraction pocket of the tympanic membrane, creating a
persistently high negative pressure of the middle ear. The skin forms a sac
that fills with degenerated skin and sebaceous ma-terials. The sac can attach
to the structures of the middle ear or mastoid, or both. Cholesteatoma alone
usually does not cause pain; however, if treatment or surgery is delayed, the
cholestea-toma may destroy structures of the temporal bone. In cases of
cholesteatoma, audiometric tests often show a conductive or mixed hearing loss.
Medical Management
Local
treatment of chronic otitis media consists of careful suc-tioning of the ear
under microscopic guidance. Instillation of antibiotic drops or application of
antibiotic powder is used to treat a purulent discharge. Systemic antibiotics
are usually not prescribed except in cases of acute infection.
SURGICAL MANAGEMENT
Surgical
procedures, including tympanoplasty, ossiculoplasty, and mastoidectomy, are
used after medical treatments are deter-mined to be ineffective. Chronic otitis
media can cause chronic mastoiditis and lead to the formation of cholesteatoma.
It can occur in the middle ear, mastoid cavity, or both, often dictating the
type of surgery to be performed. If untreated, cholesteatoma will continue to
enlarge, possibly causing damage to the facial nerve and horizontal canal and
destruction of other surrounding structures.
Tympanoplasty.The most common surgical procedure forchronic otitis media is a
tympanoplasty, or surgical reconstruc-tion of the tympanic membrane.
Reconstruction of the ossicles may also be required. The purposes of a
tympanoplasty are to reestablish middle ear function, close the perforation,
prevent recurrent infection, and improve hearing.
There
are five types of tympanoplasties. The simplest surgical procedure, type I
(myringoplasty), is designed to close a perfora-tion in the tympanic membrane.
The other procedures, types II through V, involve more extensive repair of middle
ear structures. The structures and the degree of involvement can differ, but
all tympanoplasty procedures include restoring the continuity of the sound
conduction mechanism.
Tympanoplasty
is performed through the external auditory canal with a transcanal approach or
through a postauricular in-cision. The contents of the middle ear are carefully
inspected, and the ossicular chain is evaluated. Ossicular interruption is most
frequent in chronic otitis media, but problems of recon-struction can also occur
with malformations of the middle ear and ossicular dislocations due to head
injuries. Dramatic improve-ment in hearing can result from closure of a
perforation and reestablishment of the ossicles. Surgery is usually performed
in an outpatient environment under moderate sedation or general anesthesia.
Ossiculoplasty.Many people use the termtympanoplastyto
in-clude ossiculoplasty, or surgical
reconstruction of the middle ear bones to restore hearing. Prostheses made of
materials such as Teflon, stainless steel, and hydroxyapatite are used to
reconnect the ossicles, thereby reestablishing the sound conduction mecha-nism.
However, the greater the damage, the lower the success rate for restoring
normal hearing.
Mastoidectomy.The objectives of mastoid surgery are to removethe cholesteatoma, gain
access to diseased structures, and create a dry and healthy ear. If possible,
the ossicles are reconstructed dur-ing the initial surgical procedure.
Occasionally, extensive disease dictates that this be performed as part of a
planned second-stage operation.
A
mastoidectomy is usually performed through a postauricu-lar incision. Infection
is eliminated by removing the mastoid air cells. Although infrequently injured,
the facial nerve, which runs through the middle ear and mastoid, is at some
risk for injury during mastoid surgery. As the patient awakens from anesthesia,
any evidence of facial paresis should be reported to the physician. A second
mastoidectomy may be necessary to check for recur-rent or residual cholesteatoma.
The hearing mechanism may be reconstructed at this time. The success rate for
correcting this conductive hearing loss is approximately 75%. Surgery is
usually performed in an outpatient setting. The patient has a mastoid pressure
dressing, which can be removed 24 to 48 hours after surgery.
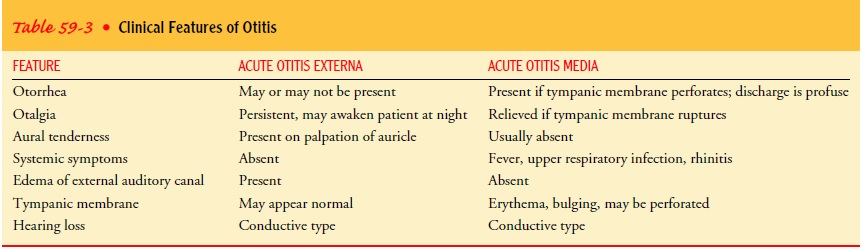
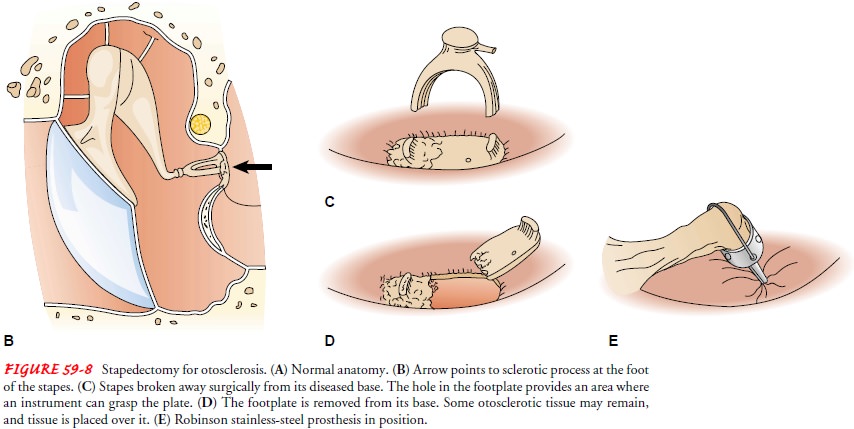
OTOSCLEROSIS
Otosclerosis
involves the stapes and
is thought to result from theformation of new, abnormal spongy bone, especially
around the oval window, with resulting fixation of the stapes. The efficient
transmission of sound is prevented because the stapes cannot vibrate and carry
the sound as conducted from the malleus and incus to the inner ear. More common
in women and frequently hereditary, otosclerosis may be worsened by pregnancy.
Clinical Manifestations
The condition can involve one or both ears and
manifests as a pro-gressive conductive or mixed hearing loss. The patient may
or may not complain of tinnitus. Otoscopic examination usually reveals a normal
tympanic membrane. Bone conduction is better than air conduction on Rinne
testing. The audiogram confirms conduc-tive hearing loss or mixed loss,
especially in the low frequencies.
Medical Management
There
is no known nonsurgical treatment for otosclerosis. However, some physicians
believe the use of Florical (a fluoride supplement) can mature the abnormal
spongy bone growth. Amplification with a hearing aid also may help.
SURGICAL MANAGEMENT
A
stapedectomy, performed through the canal, involves removing the stapes
superstructure and part of the footplate and inserting a tissue graft and a
suitable prosthesis (Fig. 59-8). Some surgeons elect to remove only a small
part of the stapes footplate (ie, stape-dotomy). Regardless of the method used,
the prosthesis bridges the gap between the incus and the inner ear, providing
better sound conduction. Stapes surgery is very successful in improving
hearing. Balance disturbance or true vertigo, which rarely occurs in other
middle ear surgical procedures, can occur for a short time after stapedectomy.
MIDDLE EAR MASSES
Other
than cholesteatoma, masses in the middle ear are rare. Glo-mus jugulare is a
tumor that arises from the jugular bulb. A his-tologically identical tumor that
arises from Jacobson’s nerve and remains limited to the middle ear is known as
a glomus tympan-icum. On otoscopy, a red blemish on or behind the tympanic
membrane is indicative of a glomus tumor. The treatment for glomus tumors is
surgical excision, except in poor surgical candi-dates, in whom radiation
therapy is used.
A facial nerve neuroma is a tumor on cranial nerve VII, the fa-cial nerve. These types of tumors are usually not visible on oto-scopic examination but are suspected when a patient presents with a facial nerve paresis. X-ray evaluation is necessary to determine the site of the tumor along the facial nerve. The treatment is sur-gical removal.
Other
less common problems of the middle ear include cho-lesterin granuloma and
tympanosclerosis. Cholesterin granuloma is an immune system reaction to the
byproducts of blood (ie, cho-lesterol crystals) within the middle ear.
Tympanosclerosis is a de-posit of collagen and minerals within the middle ear
that can harden around the ossicles as a result of repeated infections. It can
also be found as plaque on the tympanic membrane; this can de-crease hearing.
Related Topics