Chapter: Medical Surgical Nursing: Assessment and Management of Patients With Hearing and Balance Disorders
Diagnostic Evaluation of Patients With Hearing and Balance Disorders
Diagnostic Evaluation
Many
diagnostic procedures are available to measure the auditory and vestibular
systems indirectly. These tests are usually performed by an audiologist who is
recognized by the American Speech-Language-Hearing Association with a
certificate of clinical com-petence in audiology.
AUDIOMETRY
In detecting hearing loss, audiometry is the single most impor-tant diagnostic instrument. Audiometric testing is of two kinds: pure-tone audiometry, in which the sound stimulus consists of a pure or musical tone (the louder the tone before the patient per-ceives it, the greater the hearing loss), and speech audiometry, in which the spoken word is used to determine the ability to hear and discriminate sounds and words.
When
evaluating hearing, three characteristics are important: frequency, pitch, and
intensity. Frequency refers to the
number of sound waves emanating from a source per second, measured as cycles
per second, or Hertz (Hz). The normal human ear perceives sounds ranging in
frequency from 20 to 20,000 Hz. The fre-quencies from 500 to 2,000 Hz are
important in understanding everyday speech and are referred to as the speech
range or speech frequencies. Pitch is
the term used to describe frequency; a tone with 100 Hz is considered of low
pitch, and a tone of 10,000 Hz is considered of high pitch.
The unit for measuring loudness (ie, intensity of sound) is the decibel (dB), the pressure exerted by sound. Hearing loss is mea-sured in decibels, a logarithmic function of intensity that is not eas-ily converted into a percentage. The critical level of loudness is approximately 30 dB. The shuffling of papers in quiet surroundings is about 15 dB; a low conversation, 40 dB; and a jet plane 100 feet away, about 150 dB. Sound louder than 80 dB is perceived by the human ear to be harsh and can be damaging to the inner ear.
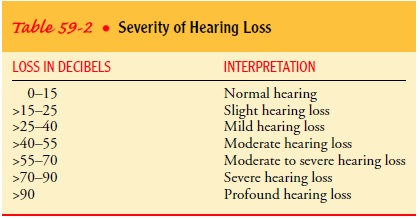
Table 59-2
classifies hearing loss based on decibel level. In surgi-cal treatment of
patients with hearing loss, the aim is to improve the hearing level to 30 dB or
better within the speech frequencies.
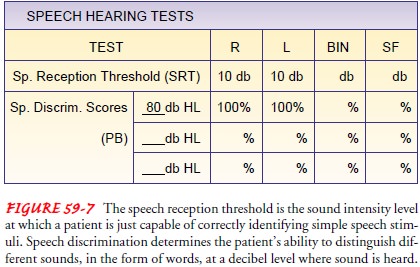
With audiometry, the patient wears earphones and
signals to the audiologist when a tone is heard. When the tone is applied
di-rectly over the external auditory canal, air conduction is measured. When
the stimulus is applied to the mastoid bone, bypassing the conductive mechanism
(ie, ossicles), nerve conduction is tested. For accuracy, audiometric
evaluations are performed in a sound-proof room. Responses are plotted on a
graph known as an audio-gram, which differentiates conductive from
sensorineural hearing loss. Speech discrimination is also measured (Fig. 59-7).
TYMPANOGRAM
A
tympanogram, or impedance audiometry, measures middle ear muscle reflex to
sound stimulation and compliance of the tym-panic membrane by changing the air
pressure in a sealed ear canal. Compliance is impaired with middle ear disease.
AUDITORY BRAIN STEM RESPONSE
The auditory brain stem response is a detectable
electrical poten-tial from cranial nerve VIII and the ascending auditory
pathways of the brain stem in response to sound stimulation. Electrodes are
placed on the patient’s forehead. Acoustic stimuli, usually in the form of
clicks, are made in the ear. The resulting electrophysio-logic measurements can
determine at which decibel level a patient hears and whether there are any
impairments along the nerve pathways (eg, tumor on cranial nerve VIII).
ELECTRONYSTAGMOGRAPHY
Electronystagmography is the measurement and graphic recording of the changes in electrical potentials created by eye movements during spontaneous, positional, or calorically evoked nystagmus.
It
is also used to assess the oculomotor and vestibular systems and their
corresponding interaction. It helps in diagnosing conditions such as Ménière’s disease and tumors of the
internal auditory canal or posterior fossa. Any vestibular suppressants, such
as seda-tives, tranquilizers, antihistamines, and alcohol are withheld for 24
hours before testing. Prior to the test the procedure is explained to the
patient.
PLATFORM POSTUROGRAPHY
Platform posturography is used to investigate
postural control capabilities. The integration of visual, vestibular, and
propriocep-tive cues (ie, sensory integration) with motor response output and
coordination of the lower limbs is tested. The patient stands on a platform,
surrounded by a screen, and different conditions such as a moving platform with
a moving screen or a stationary plat-form with a moving screen are presented.
The responses from the patient on six different conditions are measured and
indicate which of the anatomic systems may be impaired. Preparation for the
testing is the same as for electronystagmography.
SINUSOIDAL HARMONIC ACCELERATION
Sinusoidal harmonic acceleration, or a rotary
chair, is used to assess the vestibulo-ocular system by analyzing compensatory
eye movements in response to the clockwise and counterclockwise ro-tation of
the chair. Although such testing cannot identify the side of the lesion in
unilateral disease, it helps identify disease and evaluate the course of
recovery. The same patient preparation is required as for
electronystagmography.
MIDDLE EAR ENDOSCOPY
With
endoscopes with very small diameters and acute angles, the ear can be examined
endoscopically by an endoscopist spe-cializing in otolaryngology. Middle ear
endoscopy is performed safely and effectively as an office procedure to
evaluate sus-pected perilymphatic fistula and new-onset conductive hearing
loss, the anatomy of the round window before transtympanic treatment of
Ménière’s disease, and the tympanic cavity before ear surgery to treat chronic
middle ear and mastoid infections. The tympanic membrane is anesthetized
topically for about
10
minutes. Then, the external auditory canal is irrigated with sterile normal
saline solution. With the aid of a microscope, a tympanotomy is created with a
laser beam or a myringotomy knife, so that the endoscope can be inserted into
the middle ear cavity. Video and photo documentation can be accomplished
through the scope.
Related Topics