Chapter: Medical Surgical Nursing: Assessment and Management of Patients With Hearing and Balance Disorders
Hearing Loss
Hearing Loss
More
than 26 million people in the United States have some form of hearing
impairment (Larson et. al., 2000). Most can be helped with medical or surgical
therapies or with a hearing aid. By the year 2050, about one of every five
people in the United States, or almost 58 million people, will be 55 years of
age or older. Of this population, almost one half can expect a hearing
impairment (U.S. Public Health Service, 2000).
Approximately 10 million persons in the United
States have irreversible hearing loss (National Strategic Research Plan of the
National Institute on Deafness and Other Communication Dis-orders [NIDCD],
1998). It is estimated that more than 30 mil-lion people are exposed to noise
levels that produce hearing loss on a daily basis. Occupations such as
carpentry, plumbing, and coal mining have the highest risk of noise-induced
hearing loss. Researchers report greater than 90% of coal miners are estimated
to have hearing loss by the age of 52 years (Franks, 1996).
Conductive
hearing loss usually results from an external ear disorder, such as impacted
cerumen, or a middle ear disorder, such as otitis media or otosclerosis. In
such instances, the effi-cient transmission of sound by air to the inner ear is
interrupted. A sensorineural loss involves damage to the cochlea or
vestibu-locochlear nerve.
Mixed
hearing loss and functional hearing loss also may occur. The patient with mixed
hearing loss has conductive loss and sensorineural loss, resulting from
dysfunction of air and bone conduction. A functional (or psychogenic) hearing
loss is nonorganic and unrelated to detectable structural changes in the
hearing mechanisms; it is usually a manifestation of an emo-tional disturbance.
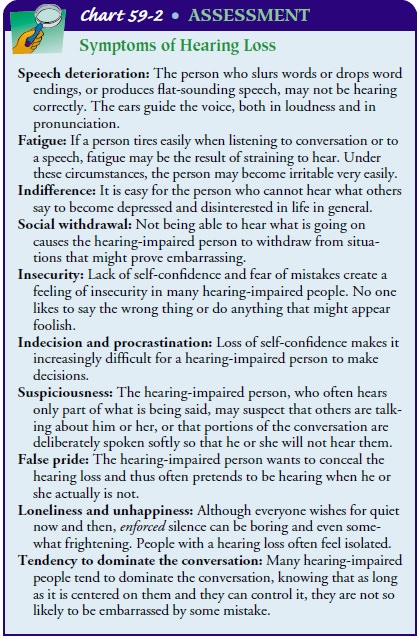
Clinical Manifestations
Early manifestations of hearing impairment and loss
may include tinnitus, increasing inability to hear in groups, and a need to
turn up the volume of the television. Hearing impairment can also trig-ger
changes in attitude, the ability to communicate, the awareness of surroundings,
and even the ability to protect oneself, affecting the person’s quality of
life. In a classroom, a student with impaired hearing may be disinterested and
inattentive and have failing grades. A person at home may feel isolated because
of an inability to hear the clock chime, the refrigerator hum, the birds sing,
or the traffic pass. A hearing-impaired pedestrian may attempt to cross the
street and fail to hear an approaching car. Hearing-impaired people may miss
parts of a conversation. Many people are unaware of their gradual hearing
impairment. Often, it is not the person with the hearing loss, but the people
with whom he or she is com-municating who recognize the impairment first (see
Chart 59-2).
For various reasons, some people with hearing loss
refuse to seek medical attention or wear a hearing aid. Others feel
self-conscious wearing a hearing aid. Insightful patients generally ask those
with whom they are trying to communicate to let them know whether difficulties
in communication exist. These attitudes and behaviors should be taken into
account when counseling patients who need hearing assistance. The decision to
wear a hearing aid is a personal one that is affected by these attitudes and
behaviors.
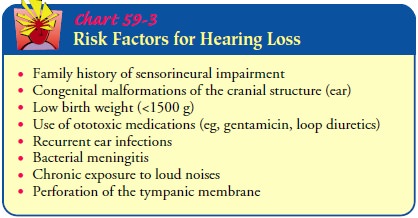
Prevention
Many environmental factors have an adverse effect on the audi-tory system and, with time, result in permanent sensorineural hearing loss. The most common is noise Noise
(ie, unwanted and unavoidable sound) has been identi-fied as one of the
environmental hazards of the 20th century. The sheer volume of noise that
surrounds us daily has increased from a simple annoyance into a potentially
dangerous source of phys-ical and psychological damage.
In terms of physical impact, loud, persistent noise
has been found to cause constriction of peripheral blood vessels, increased
blood pressure and heart rate (because of increased secretion of adrenalin),
and increased gastrointestinal activity. Additional re-search is needed to
address the overall effects of noise on the human body. It seems certain,
however, that a quiet environment is more conducive to peace of mind. A person
who is ill feels more at ease when noise is kept to a minimum. There are
numerous factors that contribute to hearing loss (see Chart 59-3).
The
term noise-induced hearing loss is
used to describe hearing loss that follows a long period of exposure to loud
noise (eg, heavy machinery, engines, artillery). Acoustic trauma refers to the hear-ing loss caused by a single
exposure to an extremely intense noise, such as an explosion. Usually,
noise-induced hearing loss occurs at a high frequency (around 4,000 Hz).
However, with contin-ued noise exposure, the hearing loss can become more
severe and include adjacent frequencies. The minimum noise level known to cause
noise-induced hearing loss, regardless of duration, is about 85 to 90 dB.
Noise exposure is inherent in many jobs (eg, mechanics, print-ers, pilots, musicians) and in hobbies such as woodworking and hunting.
The Occupational Safety and Health Administration re-quires that workers wear
ear protection to prevent noise-induced hearing loss when exposed to noise
above the legal limits. There are no medications that protect against
noise-induced hearing loss; hearing loss is permanent because the hair cells in
the organ of Corti are destroyed. Ear protection against noise is the most
effective preventive measure available.
Gerontologic Considerations
About
30% of people 65 years of age and older and 50% of peo-ple 75 years and older
have hearing difficulties. The cause is un-known; linkages to diet, metabolism,
arteriosclerosis, stress, and heredity have been inconsistent (Cruickshanks et
al., 1998).
With aging, changes occur in the ear that may
eventually lead to hearing deficits. Although few changes occur in the external
ear, cerumen tends to become harder and drier, posing a greater chance of
impaction. In the middle ear, the tympanic membrane may atrophy or become
sclerotic. In the inner ear, cells at the base of the cochlea degenerate. A
familial predisposition to sensori-neural hearing loss is also seen, manifested
by a loss in the ability to hear high-frequency sounds, followed in time by the
loss of middle and lower frequencies. The term presbycusis is used to describe
this progressive hearing loss.
In
addition to age-related changes, other factors can affect hearing in the
elderly population, such as lifelong exposure to loud noises (eg, jets, guns,
heavy machinery, circular saws). Cer-tain medications, such as aminoglycosides
and aspirin, have oto-toxic effects when renal changes (eg, in the older person)
result in delayed medication excretion and increased levels of the medica-tions
in the blood. Many older people take quinine for treatment of leg cramps;
quinine can cause a hearing loss. Psychogenic fac-tors and other disease
processes (eg, diabetes) also may be partially responsible for sensorineural
hearing loss.
When
a hearing problem occurs, an evaluation is warranted. Even with the best
medical care, the person must learn to adjust to various degrees of hearing
loss. Care of elderly patients includes recognizing emotional reactions related
to hearing loss, such as suspicion of others because of an inability to hear
adequately; frustration and anger, with repeated statements such as, “I didn’t
hear what you said”; and feelings of insecurity because of the in-ability to
hear the telephone or alarms.
Medical Management
If a hearing loss is permanent or untreatable with medical or sur-gical intervention or if the patient elects not to have surgery, aural rehabilitation may be beneficial.
Nursing Management
The nurse who understands the different types of hearing loss will be more successful in adopting a communication style to fit the patient’s needs. Trying to speak in a loud voice to a person who cannot hear high-frequency sounds only makes understanding more difficult. However, strategies such as talking into the less impaired ear and using gestures and facial expressions can help (see Chart 59-4).major issue for many deaf and hearing-impaired people is that they have other health problems that often do not receive at-tention, in large part because of communication problems with their health care practitioners.
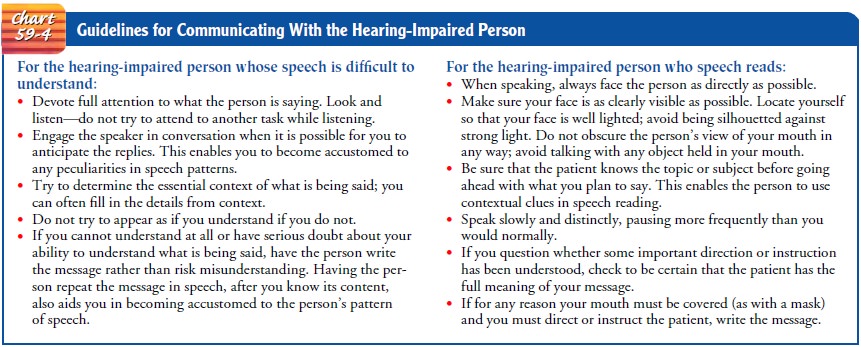
To effectively meet the health care needs of these patients, practitioners are legally obligated to make accommodations
for the patient’s inability to hear. Providing the services of interpreters or
those who can communicate through sign language is essential in many situations
so that the practi-tioner can effectively communicate with the patient.
During
health care and screening procedures, the practitioner (eg, dentist, physician,
nurse) must be aware that patients who are deaf or hearing impaired are unable
to read lips, see a signer, or read written materials in dark rooms required
during some diag-nostic tests. The same situation exists if the practitioner is
wear-ing a mask or not in sight (eg, x-ray studies, magnetic resonance imaging
[MRI], colonoscopy).
Nurses
and other health care practitioners must work with deaf and hearing-impaired
patients and their families to identify workable and effective means of
communication. Nurses can serve as catalysts throughout the health care system
to ensure that accommodations are made to meet the communication needs of these
patients.
Related Topics