Morphology, Cultural Characteristics, Pathogenesis, Clinical Symptoms, Laboratory Diagnosis, Treatment, Prophylaxis and Control Measures - Mycobacterium Tuberculosis (Tubercle Bacillus) | 12th Microbiology : Chapter 7 : Medical Bacteriology
Chapter: 12th Microbiology : Chapter 7 : Medical Bacteriology
Mycobacterium Tuberculosis (Tubercle Bacillus)
Mycobacterium Tuberculosis (Tubercle
Bacillus)
The genus
Mycobacterium is distinguished by its
thick, complex, lipidrich waxy cell walls. This high lipid content (Mycolic
acids) imparts the characteristic of acid fastness or resistance to decolorizationby
a strong acid after staining with carbol fuchsin. Many of the Mycobacterial
species are saprophytes but several species are highly significant human
pathogens. Mycobacterium tuberculosis
is the causative agent of tuberculosis (TB) It is a killer disease and ranks as
one of the most serious infection diseases of the developing countries. TB is
primarily a disease of the lungs but may spread to other sites of the body.
The name Mycobacterium tuberculosis is derived
form,
• Mycobacterium (Greek) – Fungus like bacterium
• Tuberculosis
(Latin) – Swelling or Knob
Morphology
They are
acid fast bacilli, slightly curved rods, it may occur singly or in small
clumps. They are non–motile, non–sporing, and non-capsulated.
Cultural Characteristics
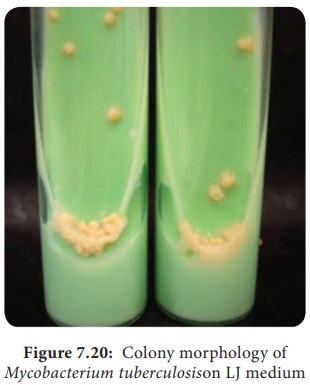
They are
obligate aerobe, optimum temperature is 37°C and optimum pH is 6.4–7.0. The
pathogen grows on an enriched culture media – Lowenstein Jensen medium. The
colonies appear in about 2–3 weeks. The colonies are dry, rough, raised,
irregular colonies with a wrinkled surface. Initially creamy white and becoming
yellowish later (Figure 7.19).
Pathogenesis
Human tuberculosis is divisible into two form, they are Primary TB and Secondary TB. The pathogenesis of Primary Tuberculosis is described in flowchart 7.8.
Source of
infection – Airborne droplets.
Route of entry – Respiratory tract .
Incubation
period – 3–6 weeks..
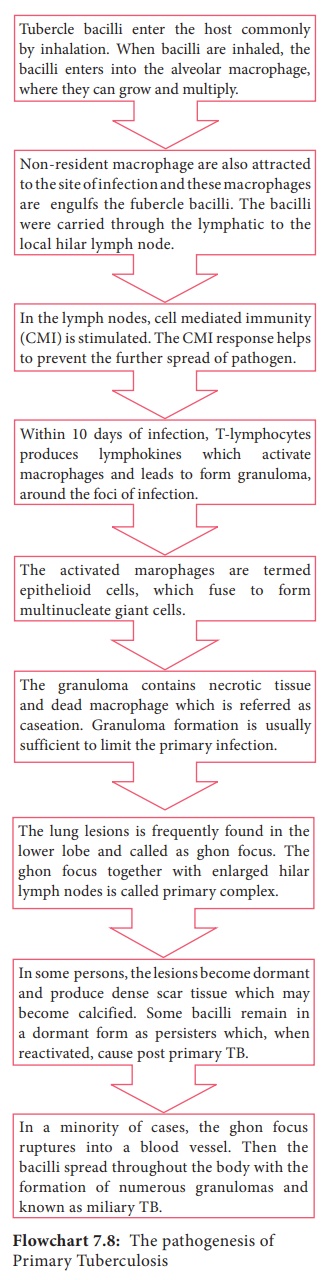
Secondary TB – (Post primary TB) It is caused by reactivation of the
primary lesion or by exogenous reinfection. Granulomas of secondary TB most
often occur in the apex of the lungs. The necrotic element of the reaction
causes tissue destruction and the formation of large area of caseation termed
tuberculomas. The presence of caseous necrosis and cavities are two important
clinical manifestations of secondary TB. The cavities may rupture into blood
vessels, spreading the bacilli throughout the body and break into airways,
releasing the pathogen in aerosols and sputum - called as open tuberculosis
(Figure 7.20).
Clinical Symptoms
It includes, cough that lasts for more than 2–3 weeks, weight loss, fever, night sweat and loss of appetite.
HOTS: M. tuberculosis the
world’s most deadly pathogen why?
Laboratory Diagnosis
Specimen: In case of pulmonary tuberculosis the most usual specimen is sputum.
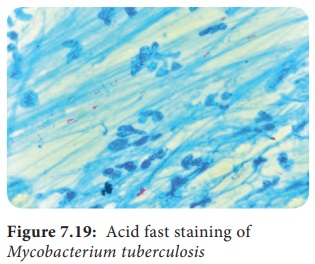
Direct Microscopy: Smear is
made from the sputum specimen and
stained by Ziehl Neelson technique. It is examined under oil immersion
objective lens. The acid fast bacilli appear as bright red bacilli against a blue
background.
Culture: The specimen is inoculated nto LJ – medium and
incubated at 37°C f2 weeks the tubercle bacilli usuallrow in 2–8 weeks. The
bacterial growth is confirmed by Ziehl – Neelsonstaining.
1. Tuberculin Skin test
Mantoux test: This method has been used
routinely. In thistest 0.1 ml of PPD (Purified protein deivative) containing 5
TU (Tuberculin unit) is injected intradermally on the flexor aspect of forearm
(Figure 7.21) Theite is examined after 48–72 hours and induration are measured
(diameter in mm)

Positive test: Indurations of diameter d10 mm
or more is considered positive.
Negative test: Indurations of 5 mm or less is
negative.
2. Gene Xpert MTB
It is an
automated diagnosis test it detects DNA sequences specific for M. tuberculosis and rifampicin
resistance by PCR. Results can be obtained within 2 hours.
Treatment
The
antitubercular drugs include two types of agents which are Bactericidal agents
– Rifampicin (R), Isoniazid (H), Pyrazinamide (z), Streptomycin.
Bacteriostatic
agents – Ethambutol (E). The regimen for treating TB consists of an intensive
phase of 2 months of isoniazid, rifampin, pyrazinamide and ethambutol, followed
by a continuation phase of 4 months of isonizid and Rifampin.
Prophylaxis and Control Measures
The BCG
(Bacille – Calmette – Guerin) administered
by intradermal injection of the
live attenuated vaccine. The immunity may last for about 10 years.
The
prevention of TB can be done by the following general measures such as
1. Adequate
nutrition.
2. Practicing good hygiene (washing hands)
3. Health
education.
4.Cover
the mouth with a tissue when you cough or sneeze.
Infobits
Drug Resistance Tuberculosis
MDR-TB: Multidrug resistance tuberculosis refers to resistance
to rifampian and Isoniazid. MDR-TB is a global problem especially in
HIV-patients.
XDR-TB: Exensively drug resistance tuberculosis refer
M.tuberculosis strains which are resistant to any fluoroquinolone and at lecest
one of 3 injectable second line drugs (Kanamycin, Capreomycin and Amikarin), in
addition to Isoniazid and rifampicin
24 a March is celebrated as World Tuberculosis day
Related Topics