Chapter: Psychiatric Mental Health Nursing : Child and Adolescent Disorders
Mental Health Promotion - Conduct Disorder
MENTAL HEALTH PROMOTION
Parental behavior profoundly influences children’s behavior.
Parents who engage in risky behaviors such as smoking, drinking, and ignoring
their health are more likely to have children who also engage in risky
behaviors, including early unprotected sex. Group-based parenting classes are
effective to deal with problem behaviors in children and to prevent later
development of conduct disorders (Turner & Sanders, 2006).
Eisen, Raleigh, and Neuhoff (2008) reported that an early
intervention program for children at risk for anxiety disorders improved
behavior. The program consisted of parent sessions, child anxiety management,
parent–child sessions that emphasized coping skills, and graduated exposure to
anxiety-provoking situations.
The SNAP-IV teacher and parent rating scale (Swanson, 2000) is an
assessment tool that can be used for initial evaluation in many areas of
concern such as ADHD, oppo-sitional defiant disorder (ODD), conduct disorder,
and depression. Such tools can identify problems or potential problems that
signal a need for further evalua-tion and follow-up. Early detection and
successful inter-vention are often the key to mental health promotion.

Oppositional Defiant Disorder
ODD consists of an enduring pattern of uncooperative, defiant, and
hostile behavior toward authority figures without major antisocial violations.
A certain level of oppositional behavior is common in children and
adoles-cents; indeed, it is almost expected at some phases such as 2 to 3 years
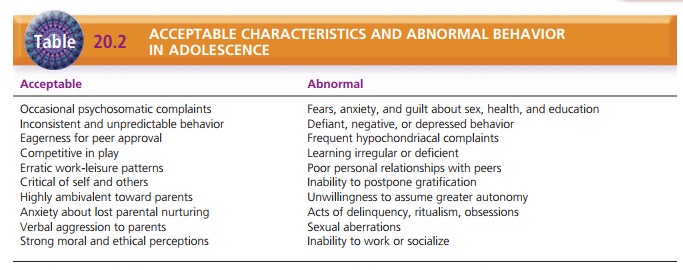
of age and in early adolescence. Table 20.2 contrasts acceptable characteristics
with abnormal behav-ior in adolescents. ODD is diagnosed only when behaviors
are more frequent and intense than in unaffected peers and cause dysfunction in
social, academic, or work situations. This disorder is diagnosed in about 5% of
the population and occurs equally among male and female adolescents. Most
authorities believe that genes, temperament, and adverse social conditions
interact to create ODD. Twenty-five percent of people with this disorder
develop conduct disorder; 10% are diagnosed with antisocial personality
disorder as adults (Thomas, 2005). ODD is often comor-bid with other
psychiatric disorders such as ADHD, anxi-ety, and affective disorders that need
to be treated as well. Treatment approaches for ODD are similar to those used
for conduct disorder.
Feeding and Eating Disorders of Infancy and Early Childhood
The disorders of feeding and eating included in this cate-gory are
persistent in nature and are not explained by underlying medical conditions.
They include pica, rumi-nation disorder, and feeding disorder.
Pica
Pica is persistent ingestion of
nonnutritive substances such as
paint, hair, cloth, leaves, sand, clay, or soil. Pica is com-monly seen in
children with mental retardation; it occasion-ally occurs in pregnant women. It
comes to the clinician’s attention only if a medical complication develops such
as a bowel obstruction or an infection or if a toxic condition develops such as
lead poisoning. In most instances, the behavior lasts for several months and
then remits.
Rumination Disorder
Rumination disorder is the repeated regurgitation
and rechew-ing of food. The child brings partially digested food up into the
mouth and usually rechews and reswallows the food. The regurgitation does not
involve nausea, vomiting, or any medical condition (APA, 2000). This disorder
is relatively uncommon and occurs more often in boys than in girls; it results
in malnutrition, weight loss, and even death in about 25% of affected infants.
In infants, the disorder frequently remits spontaneously, but it may continue
in severe cases.
Feeding Disorder
Feeding disorder of infancy or early childhood is character-ized by
persistent failure to eat adequately, which results in significant weight loss
or failure to gain weight. Feeding dis-order is equally common in boys and
girls and occurs most often during the first year of life. Estimates are that
5% of all pediatric hospital admissions are for failure to gain weight, and up
to 50% of those admissions reflect a feeding disorder with no predisposing medical condition. In
severe cases, malnutrition and death can result, but most children have
improved growth after some time (APA, 2000).
Tic Disorders
A tic is a sudden,
rapid, recurrent, nonrhythmic, stereo-typed motor movement or vocalization
(APA, 2000). Tics can be suppressed but not indefinitely. Stress exacerbates
tics, which diminish during sleep and when the person is engaged in an
absorbing activity. Common simple motor tics include blinking, jerking the
neck, shrugging the shoulders, grimacing, and coughing. Common simple vocal
tics include clearing the throat, grunting, sniffing, snorting, and barking.
Complex vocal tics include repeat-ing words or phrases out of context,
coprolalia (use of socially unacceptable words, frequently obscene), palilalia
(repeating one’s own sounds or words), and echolalia (repeating the last-heard
sound, word, or phrase; APA, 2000). Complex motor tics include facial gestures,
jump-ing, or touching or smelling an object.
Tic disorders tend to run in families. Abnormal trans-mission of
the neurotransmitter dopamine is thought to play a part in tic disorders
(Scahill & Leckman, 2005). Tic disorders usually are treated with
risperidone (Risperdal) or olanzapine (Zyprexa), which are atypical
antipsychot-ics. It is important for clients with tic disorders to get plenty
of rest and to manage stress because fatigue and stress increase symptoms.
Tourette’s Disorder
Tourette’s disorder involves multiple motor tics
and one or more vocal tics, which
occur many times a day for more than 1 year. The complexity and severity of the
tics change over time, and the person experiences almost all the pos-sible tics
described previously during his or her lifetime. The person has significant
impairment in academic, social, or occupational areas and feels ashamed and
self- conscious. This rare disorder (4 or 5 in 10,000) is more common in boys
and is usually identified by 7 years of age. Some people have lifelong
problems; others have no symptoms after early adulthood (APA, 2000).
Chronic Motor or Tic Disorder
Chronic motor or vocal tic differs from Tourette’s disorder in that
either the motor or the vocal tic is seen, but not both. Transient tic disorder
may involve single or multiple vocal or motor tics, but the occurrences last no
longer than 12 months.
Elimination Disorders
Encopresis is the repeated passage of
feces into inappro-priate places such as clothing or the floor by a child who
is at least 4 years of age either chronologically or develop-mentally. It is
often involuntary, but it can be intentional. Involuntary encopresis usually is
associated with constipation that occurs for psychological, not medical,
reasons. Intentional encopresis often is associated with ODD or conduct
disorder.
Enuresis is the repeated voiding of
urine during the day or at night
into clothing or bed by a child at least 5 years of age either chronologically
or developmentally. Most often enuresis is involuntary; when intentional, it is
asso-ciated with a disruptive behavior disorder. Seventy-five percent of
children with enuresis have a first-degree rela-tive who had the disorder. Most
children with enuresis do not have a coexisting mental disorder.
Both encopresis and enuresis are more common in boys than in girls;
1% of all 5 year olds have encopresis, and 5% of all 5 year olds have enuresis.
Encopresis can persist with intermittent exacerbations for years; it is rarely
chronic. Most children with enuresis are continent by adolescence; only 1% of
all cases persist into adulthood.
Impairment associated with elimination disorders depends on the
limitations on the child’s social activities, effects on self-esteem, degree of
social ostracism by peers, and anger, punishment, and rejection on the part of
par-ents or caregivers (APA, 2000).
Enuresis can be treated effectively with imipramine (Tof-ranil), an
antidepressant with a side effect of urinary reten-tion. Both elimination
disorders respond to behavioral approaches such as a pad with a warning bell
and to positive reinforcement for continence. For children with a disruptive
behavior disorder, psychological treatment of that disorder may improve the
elimination disorder (Mikkelsen, 2005).
Other Disorders of Infancy, Childhood, or Adolescence
Separation Anxiety Disorder
Separation anxiety disorder is characterized by anxiety exceeding
that expected for developmental level related to separation from the home or
those to whom the child is attached (APA, 2000). When apart from attachment
fig-ures, the child insists on knowing their whereabouts and may need frequent
contact with them, such as phone calls. These children are miserable away from
home and may fear never seeing their homes or loved ones again. They often
follow parents like a shadow, cannot be in a room alone, and have trouble going
to bed at night unless some-one stays with them. Fear of separation may lead to
avoid-ance behaviors such as refusal to attend school or go on errands.
Separation anxiety disorder often is accompanied by nightmares and multiple
physical complaints such as headaches, nausea, vomiting, and dizziness.
Separation anxiety disorders are thought to result from an
interaction between temperament and parenting behav-iors. Inherited temperament
traits such as passivity, avoid-ance, fearfulness, or shyness in novel
situations coupled with parenting behaviors that encourage avoidance as a way
to deal with strange or unknown situations are thought to cause anxiety in the
child (Bernstein & Layne, 2005).
Selective Mutism
Selective mutism is characterized by persistent failure to speak in
social situations where speaking is expected such as school (APA, 2000).
Children may communicate by gestures, nodding or shaking the head, or
occasionally one-syllable vocalizations in a voice different from their natural
voice. These children are often excessively shy, socially withdrawn or
isolated, and clinging; they may have temper tantrums. Selective mutism is rare
and slightly more common in girls than in boys. It usually lasts only a few
months but may persist for years.
Reactive Attachment Disorder
Reactive attachment disorder involves a markedly dis-turbed and developmentally
inappropriate social related-ness in most situations. This disorder usually
begins before 5 years of age and is associated with grossly patho-genic care
such as parental neglect, abuse, or failure to meet the child’s basic physical
or emotional needs. Repeated changes in primary caregivers, such as multiple
foster care placements, also can prevent the formation of stable attachments
(APA, 2000). The disturbed social relatedness may be evidenced by the child’s
failure to ini-tiate or respond to social interaction (inhibited type) or
indiscriminate sociability or lack of selectivity in choice of attachment
figures (disinhibited type). In the first type, the child will not cuddle or
desire to be close to anyone. In the second type, the child’s response is the
same to a stranger or to a parent.
Initially, treatment focuses on the child’s safety, includ-ing
removal of the child from the home if neglect or abuse is found. Individual and
family therapy (either with par-ents or foster caregivers) is most effective.
With early identification and effective intervention, remission or considerable
improvements can be attained. Otherwise, the disorder follows a continuous
course, with relation-ship problems persisting into adulthood.
Stereotypic Movement Disorder
Stereotypic movement disorder is associated with many genetic,
metabolic, and neurologic disorders and often accompanies mental retardation.
The precise cause is unknown. It involves repetitive motor behavior that is
nonfunctional and either interferes with normal activities or results in
self-injury requiring medical treatment (APA, 2000). Stereotypic movements may include waving, rock-ing, twirling
objects, biting fingernails, banging the head, biting or hitting oneself, or
picking at the skin or body orifices. Generally speaking, the more severe the
retarda-tion, the higher the risk for self-injury behaviors. Stereo-typic
movement behaviors are relatively stable over time but may diminish with age
(Shah, 2005).
No specific treatment has been shown effective. Clomipramine
(Anafranil) and desipramine (Norpramin) are effective in treating severe nail
biting; haloperidol (Haldol) and chlorpromazine (Thorazine) have been effective
for stereotypic movement disorder associated with mental retardation and autistic
disorder.
Related Topics