Chapter: Psychiatric Mental Health Nursing : Child and Adolescent Disorders
Delirium
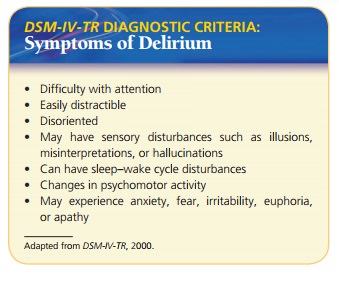
Delirium is a syndrome that involves a
disturbance of consciousness accompanied by a change in cognition. Delirium
usually develops over a short period, sometimes a matter of hours, and
fluctuates, or changes, throughout the course of the day. Clients with delirium
have difficulty paying atten-tion, are easily distracted and disoriented, and
may have sensory disturbances such as illusions, misinterpretations, or
hallucinations. An electrical cord on the floor may appear to them to be a
snake (illusion). They may mistake the banging of a laundry cart in the hallway
for a gunshot (misinterpretation). They may see “angels” hovering above when
nothing is there (hallucination). At times, they also experience disturbances
in the sleep–wake cycle, changes in psychomotor activity, and emotional
problems such as anxiety, fear, irritability, euphoria, or apathy (American
Psychiatric Association [APA], 2000).
An estimated 10% to 15% of people in the hospital for general
medical conditions are delirious at any given time. Delirium is common in older
acutely ill clients. An esti-mated 30% to 50% of acutely ill older adult
clients become delirious at some time during their hospital stay. Risk fac-tors
for delirium include increased severity of physical ill-ness, older age, and
baseline cognitive impairment such as that seen in dementia (Samuels &
Neugroschl, 2005). Children may be more susceptible to delirium, especially that
related to a febrile illness or certain medications such as anticholinergics
(APA, 2000).
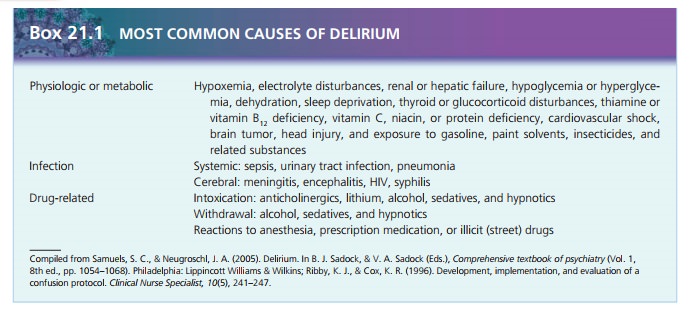
Etiology
Delirium almost always results from an identifiable physiologic,
metabolic, or cerebral disturbance or disease or from drug intoxication or
withdrawal. Often, delir-ium results from multiple causes and requires a
careful and thorough physical examination and laboratory tests for
identification.
Cultural Considerations
People from different cultural backgrounds may not be familiar with
the information requested to assess memory, such as the name of former U.S.
presidents. Other cultures may consider orientation to placement and location
differ-ently. Also, some cultures and religions, such as Jehovah’s Witnesses,
do not celebrate birthdays, so clients may have difficulty stating their date
of birth. The nurse should not mistake failure to know such information for
disorienta-tion (APA, 2000).
Treatment and Prognosis
The primary treatment for delirium is to identify and treat any
causal or contributing medical conditions. Delirium is almost always a
transient condition that clears with suc-cessful treatment of the underlying
cause. Nevertheless, some causes such as head injury or encephalitis may leave
clients with cognitive, behavioral, or emotional impair-ments even after the
underlying cause resolves.
Psychopharmacology
Clients with quiet, hypoactive delirium need no specific
pharmacologic treatment aside from that indicated for the causative condition.
Many clients with delirium, however, show persistent or intermittent
psychomotor agitation that can interfere with effective treatment or pose a
risk to safety. Sedation to prevent inadvertent self-injury may be indicated.
An antipsychotic medication, such as haloperi-dol (Haldol), may be used in
doses of 0.5 to 1 mg to decrease agitation. Sedatives and benzodiazepines are
avoided because they may worsen delirium (Samuels & Neugroschl, 2005).
Clients with impaired liver or kidney function could have difficulty
metabolizing or excreting sedatives. The exception is delirium induced by
alcohol withdrawal, which usually is treated with benzodiazepines .
Other Medical Treatment
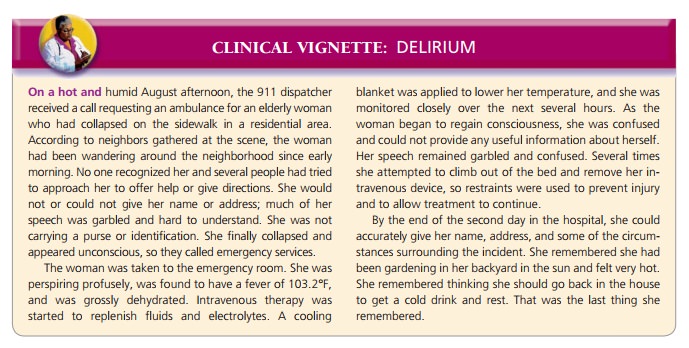
While the underlying causes of delirium are being treated, clients
also may need other supportive physical measures. Adequate nutritious food and
fluid intake speed recovery. Intravenous fluids or even total parenteral
nutrition may be necessary if a client’s physical condition has deterio-rated
and he or she cannot eat and drink.
If a client becomes agitated and threatens to dislodge intravenous
tubing or catheters, physical restraints may be necessary so that needed
medical treatments can continue. Restraints are used only when necessary and
stay in place no longer than warranted because they may increase the client’s
agitation.
Related Topics