Chapter: Psychiatric Mental Health Nursing : Child and Adolescent Disorders
Conduct Disorder
CONDUCT DISORDER
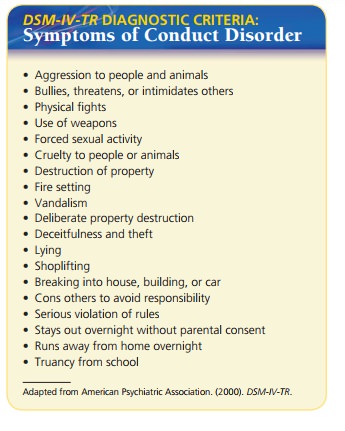
Conduct disorder is characterized by
persistent antisocial behavior in
children and adolescents that significantly impairs their ability to function
in social, academic, or occupational areas. Symptoms are clustered in four
areas:
Onset and Clinical Course
Two subtypes of conduct disorder are based on age at onset. The
childhood-onset type involves symptoms before 10 years of age, including
physical aggression toward oth-ers and disturbed peer relationships. These
children are more likely to have persistent conduct disorder and to develop
antisocial personality disorder as adults. Adoles-cent-onset type is defined by
no behaviors of conduct dis-order until after 10 years of age. These
adolescents are less likely to be aggressive, and they have more normal peer
relationships. They are less likely to have persistent con-duct disorder or
antisocial personality disorder as adults (APA, 2000).
Conduct disorders can be classified as mild, moderate, or severe
(APA, 2000):
·
Mild: The person has some conduct
problems that cause relatively minor
harm to others. Examples in-clude lying, truancy, and staying out late without
permission.
·
Moderate: The number of conduct
problems increases as does the amount
of harm to others. Examples include vandalism and theft.
·
Severe: The person has many conduct
problems that cause considerable harm
to others. Examples include forced sex, cruelty to animals, use of a weapon,
bur-glary, and robbery.
The course of conduct disorder is variable. People with the adolescent-onset
type or mild problems can achieve adequate social relationships and academic or
occupational success as adults. Those with the childhood-onset type or more
severe problem behaviors are more likely to develop antisocial personality
disorder as adults. Even those who do not have antisocial personality disorder
may lead trou-bled lives with difficult interpersonal relationships, unhealthy
lifestyles, and an inability to support themselves (Thomas, 2005).
Etiology
Researchers generally accept that genetic vulnerability,
environmental adversity, and factors like poor coping interact to cause the
disorder. Risk factors include poor parenting, low academic achievement, poor
peer relation-ships, and low self-esteem; protective factors include resil-ience,
family support, positive peer relationships, and good health (Thomas, 2005).
There is a genetic risk for conduct disorder, although no specific
gene marker has been identified (Thomas, 2005). The disorder is more common in
children who have a sibling with conduct disorder or a parent with anti-social
personality disorder, substance abuse, mood disor-der, schizophrenia, or ADHD
(APA, 2000).
A lack of reactivity of the autonomic nervous system has been found
in children with conduct disorder; this nonresponsiveness is similar to adults
with antisocial per-sonality disorder. The abnormality may cause more
aggression in social relationships as a result of decreased normal avoidance or
social inhibitions. Research into the role of neurotransmitters is promising
(Thomas, 2005).
Poor family functioning, marital discord, poor parent-ing, and a
family history of substance abuse and psychiat-ric problems are all associated
with the development of conduct disorder. Prenatal exposure to alcohol causes
an increased risk for conduct disorder (Disney, Iacono, McGue, Tully, &
Legrand, 2008). Child abuse is an espe-cially significant risk factor. The
specific parenting pat-terns considered ineffective are inconsistent parental
responses to the child’s demands and giving in to demands as the child’s
behavior escalates. Exposure to violence in the media and community is a
contributing factor for the child at risk in other areas. Socioeconomic
disadvantages, such as inadequate housing, crowded conditions, and pov-erty, also
increase the likelihood of conduct disorder in at-risk children (McGuinness,
2006).
Academic underachievement, learning disabilities, hyper-activity,
and problems with attention span are all associated with conduct disorder.
Children with conduct disorder have difficulty functioning in social
situations. They lack the abil-ities to respond appropriately to others and to
negotiate con-flict, and they lose the ability to restrain themselves when
emotionally stressed. They are often accepted only by peers with similar
problems (Thomas, 2005).
Cultural Considerations
Concerns have been raised that “difficult” children may be
mistakenly labeled as having conduct disorder. Knowing the client’s history and
circumstances is essential for accu-rate diagnosis. In high-crime areas,
aggressive behavior may be protective and not necessarily indicative of
con-duct disorder. In immigrants from war-ravaged countries, aggressive
behavior may have been necessary for survival, so these individuals should not
be diagnosed with conduct disorder (APA, 2000).
Treatment
Many treatments have been used for conduct disorder with only
modest effectiveness. Early intervention is more effec-tive, and prevention is
more effective than treatment. Dra-matic interventions, such as “boot camp” or
incarceration, have not proved effective and may even worsen the situa-tion
(Thomas, 2005). Treatment must be geared toward the client’s developmental age;
no one treatment is suitable for all ages. Preschool programs, such as Head
Start, result in lower rates of delinquent behavior and conduct disor-der
through use of parental education about normal growth and development,
stimulation for the child, and parental support during crises.
For school-aged children with conduct disorder, the child, family,
and school environment are the focus of treatment. Techniques include parenting
education, social
Adolescents rely less on their parents and more on peers, so
treatment for this age group includes individual therapy. Many adolescent clients
have some involvement with the legal system as a result of criminal behavior,
and consequently they may have restrictions on their freedom. Use of alcohol
and other drugs plays a more significant role for this age group; any treatment
plan must address this issue. The most promising treatment approach includes
keeping the client in his or her environment with family and individual
therapies. The plan usually includes conflict reso-lution, anger management,
and teaching social skills.
Medications alone have little effect but may be used in conjunction
with treatment for specific symptoms. For example, the client who presents a
clear danger to others may be prescribed an antipsychotic medication, or a
client with a labile mood may benefit from lithium or another mood stabilizer
such as carbamazepine (Tegretol) or valp-roic acid (Depakote) (Thomas, 2005).
Related Topics