Chapter: Psychiatric Mental Health Nursing : Child and Adolescent Disorders
Attention Deficit Hyperactivity Disorder
ATTENTION DEFICIT HYPERACTIVITY
DISORDER
Attention deficit
hyperactivity disorder (ADHD) is characterized by inattentiveness, overactivity,
and impulsiveness. ADHD is a common disorder, especially in boys, and probably
accounts for more child mental health referrals than any other single disorder
(Hechtman, 2005). The essential feature of ADHD is a persistent pattern of
inatten-tion and/or hyperactivity and impulsivity more common than generally
observed in children of the same age.
ADHD affects an estimated 3% to 5% of all school-aged children. The
ratio of boys to girls ranges from 3:1 in non-clinical settings to 9:1 in
clinical settings (Hechtman, 2005). To avoid overdiagnosis of ADHD, a qualified
spe-cialist such as a pediatric neurologist or a child psychia-trist must
conduct the evaluation for ADHD. Children who are very active or hard to handle
in the classroom can be diagnosed and treated mistakenly for ADHD. Some of
these overly active children may suffer from psychosocial stressors at home,
inadequate parenting, or other psychiatric

Onset and Clinical Course
ADHD usually is identified and diagnosed when the child begins
preschool or school, although many parents report problems from a much younger
age. As infants, children with ADHD are often fussy and temperamental and have
poor sleeping patterns. Toddlers may be described as “always on the go” and
“into everything,” at times disman-tling toys and cribs. They dart back and
forth, jump and climb on furniture, run through the house, and cannot tol-erate
sedentary activities such as listening to stories. At this point in a child’s
development, it can be difficult for parents to distinguish normal active
behavior from exces-sive hyperactive behavior.
By the time the child starts school, symptoms of ADHD begin to
interfere significantly with behavior and perfor-mance (Dang, Warrington, Tung,
Baker, & Pan, 2007). The child fidgets constantly, is in and out of
assigned seats, and makes excessive noise by tapping or playing with pen-cils
or other objects. Normal environmental noises, such as someone coughing,
distract the child. He or she cannot listen to directions or complete tasks.
The child interrupts and blurts out answers before questions are completed.
Academic performance suffers because the child makes hurried,
careless mistakes in schoolwork, often loses or forgets homework assignments,
and fails to follow directions.
Socially, peers may ostracize or even ridicule the child for his or
her behavior. Forming positive peer relation-ships is difficult because the
child cannot play coopera-tively or take turns and constantly interrupts others
(APA, 2000). Studies have shown that both teachers and peers perceive children
with ADHD as more aggressive, more bossy, and less likable (Hechtman, 2005).
This perception results from the child’s impulsivity, inability to share or
take turns, tendency to interrupt, and failure to listen to and follow
directions. Thus, peers and teachers may exclude the child from activities and
play, may refuse to socialize with the child, or may respond to the child in a
harsh, punitive, or rejecting manner.
Approximately two thirds of children diagnosed with ADHD continue
to have problems in adolescence. Typical impulsive behaviors include cutting
class, getting speed-ing tickets, failing to maintain interpersonal
relationships, and adopting risk-taking behaviors, such as using drugs or
alcohol, engaging in sexual promiscuity, fighting, and vio-lating curfew. Many
adolescents with ADHD have disci-pline problems serious enough to warrant
suspension or expulsion from high school (Hechtman, 2005). The sec-ondary
complications of ADHD, such as low self-esteem and peer rejection, continue to
pose serious problems.
Previously, it was believed that children outgrew ADHD, but it is
now known that ADHD can persist into adulthood. Estimates are that 30% to 50%
of children with ADHD have symptoms that continue into adulthood. In one study,
adults who had been treated for hyperactivity 25 years ear-lier were three to
four times more likely than their brothers to experience nervousness,
restlessness, depression, lack of friends, and low frustration tolerance.
Approximately 70% to 75% of adults with ADHD have at least one coexisting
psychiatric diagnosis, with social phobia, bipolar disorder, major depression,
and alcohol dependence being the most common (Antai-Otong, 2008).
Etiology
Although much research has taken place, the definitive causes of
ADHD remain unknown. There may be cortical-arousal, information-processing, or
maturational abnor-malities in the brain (Rowe & Hermens, 2006). Combined
factors, such as environmental toxins, prenatal influences, heredity, and
damage to brain structure and functions, are likely responsible (Hechtman,
2005). Prenatal exposure to alcohol, tobacco, and lead and severe malnutrition
in early childhood increase the likelihood of ADHD. Although the relation
between ADHD and dietary sugar and vitamins has been studied, results have been
incon-clusive ( Hechtman, 2005).
Brain images of people with ADHD suggest decreased metabolism in
the frontal lobes, which are essential for attention, impulse control,
organization, and sustained goal-directed activity. Studies also have shown
decreased blood perfusion of the frontal cortex in children with ADHD and
frontal cortical atrophy in young adults with a history of childhood ADHD.
Another study showed decreased glucose use in the frontal lobes of parents of
children with ADHD who had ADHD themselves (Hechtman, 2005). Evidence is not
conclusive, but research in these areas seems promising.
There seems to be a genetic link for ADHD that is most likely
associated with abnormalities in catecholamine and possibly serotonin
metabolism. Having a first-degree rela-tive with ADHD increases the risk of the
disorder by four to five times more than that of the general population
(Hechtman, 2005). Despite the strong evidence support-ing a genetic
contribution, there are also sporadic cases of ADHD with no family history of
ADHD; this furthers the theory of multiple contributing factors.
Risk factors for ADHD include family history of ADHD; male
relatives with antisocial personality disorder or alco-holism; female relatives
with somatization disorder; lower socioeconomic status; male gender; marital or
family dis-cord, including divorce, neglect, abuse, or parental depri-vation;
low birth weight; and various kinds of brain insult (Hechtman, 2005).
Cultural Considerations
ADHD is known to occur in various cultures. It is more prevalent in
Western cultures, but that may be the result of different diagnostic practices
rather than the actual differ-ences in existence (APA, 2000).
The Child Behavior Checklist, Teacher Report Form, and Youth Self
Report (for ages 11 to 18 years) are rating scales frequently used to determine
problem areas and competencies. These scales are often part of a comprehen-sive
assessment of ADHD in children. They have been determined to be culturally
competent and are widely used in various countries (King et al., 2005).
Pierce and Reid (2004) found that an increasing number of children
from culturally diverse groups are diagnosed with ADHD. They believe this
increase may represent overidentification of ADHD in culturally diverse
children and urge practitioners to consider cultural con-text before making the
diagnosis.
Yeh, Hough, McCabe, Lau, and Garland (2004) stud-ied parental
beliefs about the causes of mental illness in their children. They found that
African-American, Asian/ Pacific Islander American, and Latino parents were
less likely to endorse biopsychosocial causes of mental illness than
non-Hispanic white parents and were more likely to believe in sociologic
causes. The authors believe this may affect participation in and compliance
with prescribed treatment.
Treatment
No one treatment has been found to be effective for ADHD; this
gives rise to many different approaches such as sugar-controlled diets and
megavitamin therapy. Parents need to know that any treatment heralded as the
cure for ADHD is probably too good to be true (Hechtman, 2005). ADHD is
chronic; goals of treatment involve managing symptoms, reducing hyperactivity
and impulsivity, and increasing the child’s attention so that he or she can
grow and develop normally. The most effective treatment combines pharma-cotherapy
with behavioral, psychosocial, and educational interventions (Dang et al.,
2007).
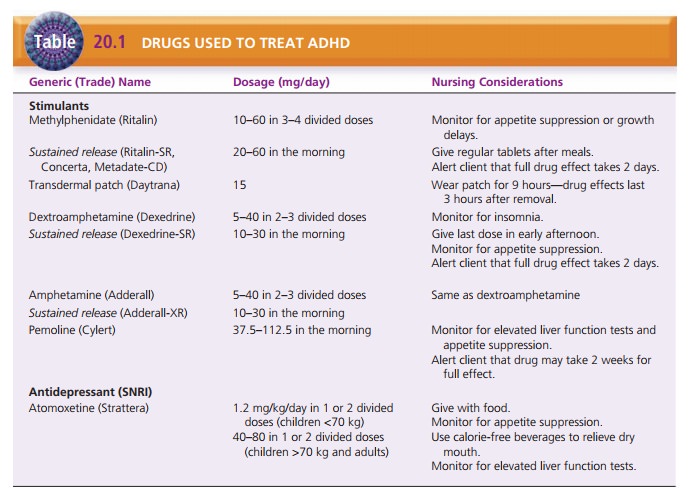
Psychopharmacology
Medications often are effective in decreasing hyperactivity and
impulsiveness and improving attention; this enables the child to participate in
school and family life. The most common medications are methylphenidate
(Ritalin) and an amphetamine compound (Adderall) (Hechtman, 2005; Lehne, 2006).
Methylphenidate is effective in 70% to 80% of children with ADHD; it reduces
hyperactivity, impulsiv-ity, and mood lability and helps the child to pay
attention more appropriately. Dextroamphetamine (Dexedrine) and pemoline
(Cylert) are other stimulants used to treat ADHD. The most common side effects
of these drugs are insomnia, loss of appetite, and weight loss or failure to
gain weight. Methylphenidate, dextroamphetamine, and amphetamine compounds are
also available in a sustained-release form taken once daily; this eliminates
the need for additional doses when the child is at school. Methylphenidate is
also available in a daily transdermal patch, marketed
Giving stimulants during daytime hours usually effec-tively combats
insomnia. Eating a good breakfast with the morning dose and substantial
nutritious snacks late in the day and at bedtime helps the child to maintain an
adequate dietary intake. When stimulant medications are not effective or their
side effects are intolerable, anti-depressants are the second choice for
treatment . Atomoxetine (Strattera) is the only nonstim-ulant drug specifically
developed and tested by the U.S. Food and Drug Administration for treatment of
ADHD. It is an antidepressant, specifically a selective norepi-nephrine
reuptake inhibitor. The most common side effects in children during clinical
trials were decreased appetite, nausea, vomiting, tiredness, and upset
stom-ach. In adults, side effects were similar to those of other
antidepressants, including insomnia, dry mouth, urinary retention, decreased
appetite, nausea, vomiting, dizzi-ness, and sexual side effects. In addition,
atomoxetine can cause liver damage, so individuals taking the drug need to have
liver function tests periodically (Cheng, Chen, Ko, & Ng, 2007). Table 20.1
lists drugs, dosages, and nursing considerations for clients with ADHD.
Strategies for Home and School
Medications do not automatically improve the child’s aca-demic
performance or ensure that he or she makes friends. Behavioral strategies are
necessary to help the child to master appropriate behaviors. Environmental
strategies at school and home can help the child to succeed in those settings.
Educating parents and helping them with parent-ing strategies are crucial
components of effective treatment of ADHD. Effective approaches include
providing consis-tent rewards and consequences for behavior, offering
con-sistent praise, using time-out, and giving verbal reprimands. Additional
strategies are issuing daily report cards for behavior and using point systems
for positive and negative behavior (Hechtman, 2005).
In therapeutic play,
play techniques are used to under-stand the child’s thoughts and feelings and
to promote communication. This should not be confused with play therapy, a
psychoanalytic technique used by psychiatrists. Dramatic play is acting out an
anxiety-producing situation such as allowing the child to be a doctor or use a
stetho-scope or other equipment to take care of a patient (a doll). Play
techniques to release energy could include pounding pegs, running, or working
with modeling clay. Creative play techniques can help children to express
themselves, for example, by drawing pictures of themselves, their family, and
peers. These techniques are especially useful when children are unable or
unwilling to express themselves verbally.
Related Topics