Chapter: Psychiatric Mental Health Nursing : Child and Adolescent Disorders
Child and Adolescent Disorders
Child and
Adolescent Disorders
PSYCHIATRIC DISORDERS ARE not diagnosed as easily in
children as they are in adults.
Children usually lack the abstract cognitive abilities and verbal skills to
describe what is happening. Because they are constantly changing and
developing, children have limited sense of a stable, normal self to allow them
to discriminate unusual or unwanted symptoms from normal feelings and
sensations. Additionally, behaviors that are normal in a child of one age may
indicate problems in a child of another age. For example, an infant who cries
and wails when separated from his or her mother is normal. If the same child at
5 years of age cries and shows extreme anxiety when separated only briefly from
the mother, however, this behavior would warrant investigation.
Children and adolescents experience some of the same mental health
problems as adults, such as mood and anxiety disorders, and are diagnosed with
these disorders using the same criteria as for adults. Eating disorders,
especially anorexia, usually begin in adolescence and continue into adult-hood.
Mood, anxiety, and eating disorders are discussed in separate chap-ters of this
book.
The childhood psychiatric disorders, most com-mon in mental health
settings and specialized treatment units, include per-vasive developmental
disorders, attention deficit hyperactivity disorder (ADHD), and disruptive
behavior disorders.
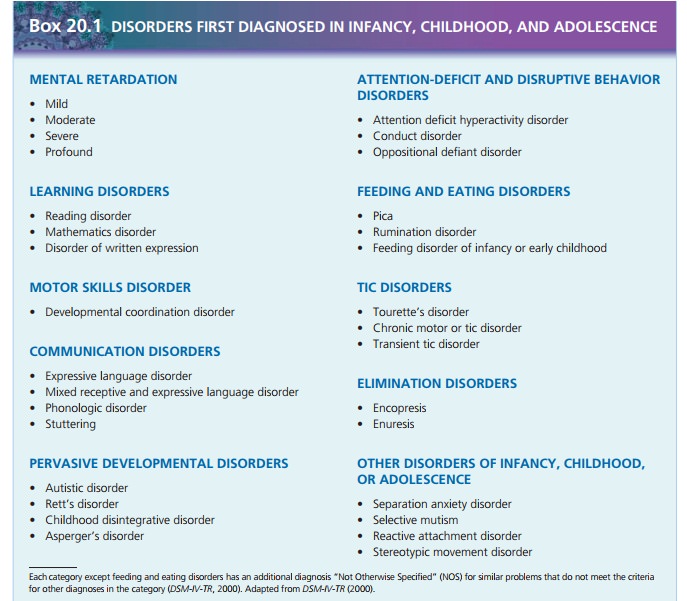
MENTAL RETARDATION
The essential feature of mental retardation is below-average
intellectual functioning (intelligence quotient [IQ] less than 70) accompanied
by significant limitations in areas of adaptive functioning such as
communication skills, self-care, home living, social or interpersonal skills,
use of community resources, self-direction, academic skills, work, leisure, and
health and safety (King, Hodapp, & Dykens, 2005). The degree of retardation
is based on IQ and greatly affects the person’s ability to function:
·
Mild retardation: IQ 50 to 70
·
Moderate retardation: IQ 35 to 50
·
Severe retardation: IQ 20 to 35
·
Profound retardation: IQ less than 20
Causes of mental retardation include hereditary condi-tions such as
Tay–Sachs disease or fragile X chromosome syndrome; early alterations in
embryonic development, such as trisomy 21 or maternal alcohol intake, that
cause fetal alcohol syndrome; pregnancy or perinatal problems such as fetal
malnutrition, hypoxia, infections, and trauma; medical conditions of infancy
such as infection or lead poisoning; and environmental influences such as
depriva-tion of nurturing or stimulation.
Some people with mental retardation are passive and dependent;
others are aggressive and impulsive. Children with mild-to-moderate mental
retardation usually receive treatment in their homes and communities and make
peri-odic visits to physicians. Those with severe or profound mental
retardation may require residential placement or day care services.
LEARNING DISORDERS
A learning disorder is diagnosed when a child’s achieve-ment in
reading, mathematics, or written expression is below that expected for age,
formal education, and intel-ligence. Learning problems interfere with academic
achievement and life activities requiring reading, math, or writing (American
Psychiatric Association [APA], 2000). Reading and written expression disorders
usually are iden-tified in the first grade; math disorder may go undetected
until the child reaches fifth grade. Approximately 5% of children in U.S.
public schools are diagnosed with a learn-ing disorder. The school dropout rate
for students with learning disorders is 1.5 times higher than the average rate
for all students (APA, 2000).
Low self-esteem and poor social skills are common in children with
learning disorders. As adults, some have prob-lems with employment or social
adjustment; others have minimal difficulties. Early identification of the
learning dis-order, effective intervention, and no coexisting problems is
associated with better outcomes. Children with learning disorders are assisted
with academic achievement through special education classes in public schools.
MOTOR SKILLS DISORDER
The essential feature of developmental
coordination disorder is impaired coordination severe enough to interfere
with academic achievement or activities of daily living (APA, 2000). This
diagnosis is not made if the problem with motor coordination is part of a
general medical condition such as cerebral palsy or muscular dystrophy. This
disor-der becomes evident as a child attempts to crawl or walk or as an older child
tries to dress independently or manip-ulate toys such as building blocks.
Developmental coordi-nation disorder often coexists with a communication
disorder. Its course is variable; sometimes lack of coordi-nation persists into
adulthood (APA, 2000). Schools pro-vide adaptive physical education and sensory
integration programs to treat motor skills disorder. Adaptive physical
education programs emphasize inclusion of movement games such as kicking a
football or soccer ball. Sensory integration programs are specific physical
therapies pre-scribed to target improvement in areas where the child has
difficulties. For example, a child with tactile defensiveness (discomfort at
being touched by another person) might be involved in touching and rubbing skin
surfaces (Pataki & Spence, 2005).
COMMUNICATION DISORDERS
A communication disorder is diagnosed when a communi-cation deficit
is severe enough to hinder development, academic achievement, or activities of
daily living, includ-ing socialization. Expressive
language disorder involves an impaired ability to communicate through
verbal and sign languages. The child has difficulty learning new words and
speaking in complete and correct sentences; his or her speech is limited. Mixed receptive-expressive language disor-der
includes the problems of expressive language disorder along with difficulty understanding (receiving) and deter-mining
the meaning of words and sentences. Both disor-ders can be present at birth
(developmental) or may be acquired as a result of neurologic injury or insult
to the brain. Phonologic disorder
involves problems with articula-tion (forming sounds that are part of speech). Stuttering is a disturbance of the
normal fluency and time patterning of speech. Phonologic disorder and
stuttering run in families and occur more frequently in boys than in girls.
Communication disorders may be mild to severe. Dif-ficulties that
persist into adulthood are related most closely to the severity of the
disorder. Speech and language thera-pists work with children who have
communication disor-ders to improve their communication skills and to teach
parents to continue speech therapy activities at home ( Johnson &
Beitchman, 2005).
PERVASIVE DEVELOPMENTAL DISORDERS
Pervasive developmental
disorders are characterized by pervasive
and usually severe impairment of reciprocal social interaction skills,
communication deviance, and restricted stereotypical behavioral patterns
(Volkmar, Klin,
· Schultz, 2005). This category of disorders is also called autism spectrum disorders and includes autistic disorder (classic autism), Rett’s disorder, childhood disintegrative disorder, and Asperger’s disorder. Approximately 75% of children with pervasive developmental disorders have mental retardation (APA, 2000).
Related Topics