Chapter: Psychiatric Mental Health Nursing : Child and Adolescent Disorders
Dementia
DEMENTIA
Dementia is a mental disorder that
involves multiple cog-nitive deficits, primarily memory impairment, and at
least one of the following cognitive disturbances (APA, 2000):
·
Aphasia, which is deterioration of
language function Apraxia, which is
impaired ability to execute motor functions
despite intact motor abilities
·
Agnosia, which is inability to
recognize or name ob-jects despite intact sensory abilities
·
Disturbance in executive
functioning, which is the ability to think abstractly and to plan,
initiate, sequence, monitor, and stop complex behavior

These cognitive deficits must be sufficiently severe to impair
social or occupational functioning and must repre-sent a decline from previous
functioning.
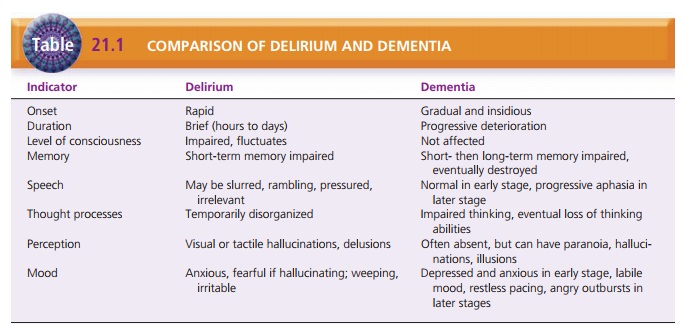
Dementia must be distinguished from delirium; if the two diagnoses
coexist, the symptoms of dementia remain even when the delirium has cleared.
Table 21.1 compares delirium and dementia.
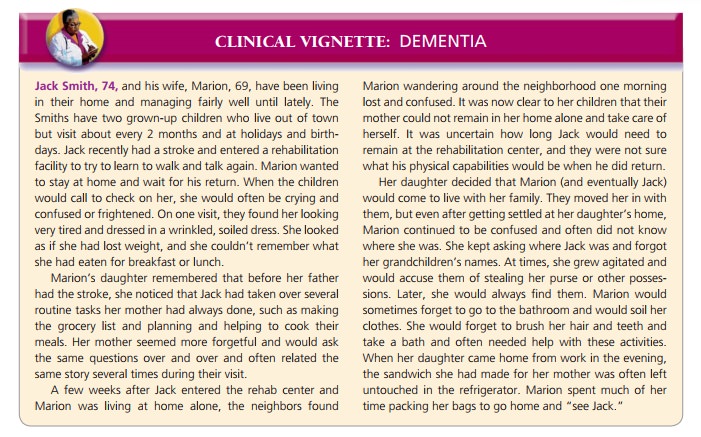
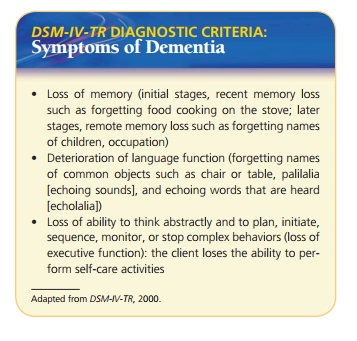
Memory impairment is the prominent early sign of dementia. Clients
have difficulty learning new material and forget previously learned material.
Initially, recent memory is impaired—for example, forgetting where cer-tain
objects were placed or that food is cooking on the stove. In later stages,
dementia affects remote memory; cli-ents forget the names of adult children, their
lifelong occu-pations, and even their names.
Aphasia usually begins with the inability to name familiar objects
or people and then progresses to speech that becomes vague or empty with
excessive use of terms such as it or thing. Clients may exhibit echolalia (echoing what is heard) or palilalia
(repeating words or sounds over and over) (APA, 2000). Apraxia may cause
clients to lose the ability to per-form routine self-care activities such as
dressing or cooking. Agnosia is frustrating for clients: they may look at a
table and chair but are unable to name them. Disturbances in execu-tive
functioning are evident as clients lose the ability to learn new material,
solve problems, or carry out daily activities such as meal planning or
budgeting.
Clients with dementia also may underestimate the risks associated
with activities or overestimate their ability to function in certain
situations. For example, while driving, clients may cut in front of other
drivers, sideswipe parked cars, or fail to slow down when they should.
Onset and Clinical Course
When an underlying, treatable cause is not present, the course of
dementia is usually progressive. Dementia often is described in stages:
·
Mild: Forgetfulness is the hallmark
of beginning, mild de-mentia. It exceeds the normal, occasional forgetfulness
experienced as part of the aging process. The person has difficulty finding
words, frequently loses objects, and be-gins to experience anxiety about these
losses. Occupa-tional and social settings are less enjoyable, and the person
may avoid them. Most people remain in the community during this stage.
·
Moderate: Confusion is apparent, along
with progressive memory loss. The
person no longer can perform com-plex tasks but remains oriented to person and
place. He or she still recognizes familiar people. Toward the end of this
stage, the person loses the ability to live indepen-dently and requires
assistance because of disorientation to time and loss of information such as
address and tele-phone number. The person may remain in the commu-nity if
adequate caregiver support is available, but some people move to supervised
living situations.
·
Severe: Personality and emotional
changes occur. The person may be
delusional, wander at night, forget the names of his or her spouse and
children, and require assistance in activities of daily living (ADLs). Most
peo-ple live in nursing facilities when they reach this stage unless
extraordinary community support is available.
Etiology
Causes vary, although the clinical picture is similar for most
dementias. Often, no definitive diagnosis can be made until completion of a
postmortem examination.
Metabolic activity is decreased in the brains of clients with
dementia; it is not known whether dementia causes decreased metabolic activity
or if decreased metabolic activity results in dementia. A genetic component has
been identified for some dementias such as Huntington’s dis-ease. An abnormal APOE gene is known to be linked with
Alzheimer’s disease. Other causes of dementia are related to infections such as
human immunodeficiency virus (HIV) infection or Creutzfeldt–Jakob disease. The
most common types of dementia and their known or hypothe-sized causes follow
(APA, 2000; Neugroschl et al., 2005):
·
Alzheimer’s disease is a progressive brain disorder
that has a gradual onset but causes
an increasing decline in functioning, including loss of speech, loss of motor
function, and profound personality and behavioral changes such as paranoia,
delusions, hallucinations, in-attention to hygiene, and belligerence. It is
evidenced by atrophy of cerebral neurons, senile plaque deposits, and
enlargement of the third and fourth ventricles of the brain. Risk for
Alzheimer’s disease increases with age, and average duration from onset of
symptoms to death is 8 to 10 years. Dementia of the Alzheimer’s type,
especially with late onset (after 65 years of age), may have a genetic
component. Research has shown link-ages to chromosomes 21, 14, and 19 (APA,
2000).
·
Vascular dementia has symptoms similar to those
of Alzheimer’s disease, but onset is
typically abrupt, fol-lowed by rapid changes in functioning; a plateau, or
leveling-off period; more abrupt changes; another level-ing-off period; and so
on. Computed tomography or magnetic resonance imaging usually shows multiple
vascular lesions of the cerebral cortex and subcortical structures resulting
from the decreased blood supply to the brain.
·
Pick’s disease is a degenerative brain
disease that par-ticularly affects the frontal and temporal lobes and re-sults
in a clinical picture similar to that of Alzheimer’s disease. Early signs
include personality changes, loss of social skills and inhibitions, emotional
blunting, and language abnormalities. Onset is most commonly 50 to 60 years of
age; death occurs in 2 to 5 years.
·
Creutzfeldt–Jakob disease is a central nervous system disorder that typically develops in
adults 40 to 60 years of age. It involves altered vision, loss of coordination
or abnormal movements, and dementia that usually pro-gresses rapidly (a few
months). The cause of the encephalopathy is an infectious particle resistant to
boiling, some disinfectants (e.g., formalin, alcohol), and ultraviolet
radiation. Pressured autoclaving or bleach can inactivate the particle.
·
HIV infection can lead to dementia and other neuro-logic problems;
these may result directly from invasion of nervous tissue by HIV or from other
acquired immu-nodeficiency syndrome–related illnesses such as toxo-plasmosis
and cytomegalovirus. This type of dementia can result in a wide variety of symptoms
ranging from mild sensory impairment to gross memory and cogni-tive deficits to
severe muscle dysfunction.
·
Parkinson’s disease is a slowly progressive
neurologic condition characterized
by tremor, rigidity, bradykine-sia, and postural instability. It results from
loss of neu-rons of the basal ganglia. Dementia has been reported in
approximately 20% to 60% of people with Parkinson’s disease and is
characterized by cognitive and motor slowing, impaired memory, and impaired
executive functioning.
·
Huntington’s disease is an inherited, dominant
gene disease that primarily involves
cerebral atrophy, demy-elination, and enlargement of the brain ventricles.
Ini-tially, there are choreiform movements that are continuous during waking
hours and involve facial contortions, twisting, turning, and tongue movements.
Personality changes are the initial psychosocial mani-festations, followed by
memory loss, decreased intellec-tual functioning, and other signs of dementia.
The disease begins in the late 30s or early 40s and may last 10 to 20 years or
more before death.
·
Dementia can be a direct pathophysiologic consequence of head
trauma. The degree and type of cognitive impairment and behavioral disturbance
depend on the location and extent of the brain injury. When it occurs as a
single injury, the dementia is usually stable rather than progressive. Repeated
head injury (e.g., from box-ing) may lead to progressive dementia.
An estimated 5 million people in the United States have moderate to
severe dementia from various causes. World-wide, it is estimated there are 4.6
million new cases each year (Smith, 2008). Prevalence rises with age: estimated
prevalence of moderate to severe dementia in people older than 65 years is
about 5%; 20% to 40% of the general pop-ulation older than 85 years have
dementia. Predictions are that by 2050, there will be 18 million Americans with
dementia (Neugroschl et al., 2005) and 114 million people with dementia
worldwide (Smith, 2008). Dementia of the Alzheimer’s type is the most common type
in North America (60% of all dementias), Scandinavia, and Europe; vascular
dementia is more prevalent in Russia and Japan. Dementia of the Alzheimer’s
type is more common in women; vascular dementia is more common in men.
Cultural Considerations
Clients from other cultures may find the questions used on many
assessment tools for dementia difficult or impossible to answer. Examples
include the names of former U.S. presidents. To avoid drawing erroneous
conclusions, the nurse must be aware of differences in the person’s knowl-edge
base.
The nurse also must be aware of different culturally influenced
perspectives and beliefs about elderly family
Treatment and Prognosis
Whenever possible, the underlying cause of dementia is identified
so that treatment can be instituted. For example, the progress of vascular
dementia, the second most com-mon type, may be halted with appropriate
treatment of the underlying vascular condition (e.g., changes in diet,
exer-cise, control of hypertension, or diabetes). Improvement of cerebral blood
flow may arrest the progress of vascular dementia in some people (Neugroschl et
al., 2005).
The prognosis for the progressive types of dementia may vary as
described earlier, but all prognoses involve progres-sive deterioration of
physical and mental abilities until death. Typically, in the later stages,
clients have minimal cognitive and motor function, are totally dependent on
caregivers, and are unaware of their surroundings or people in the environment.
They may be totally uncommunicative or make unintelligible sounds or attempts to
verbalize.
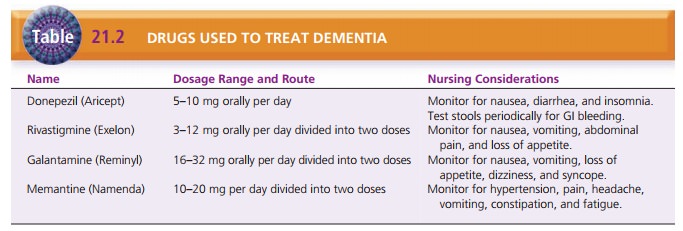
For degenerative dementias, no direct therapies have been found to
reverse or retard the fundamental pathophys-iologic processes. Levels of
numerous neurotransmitters such as acetylcholine, dopamine, norepinephrine, and
serotonin are decreased in dementia. This has led to attempts at replenishment
therapy with acetylcholine precursors, cholinergic agonists, and cholinesterase
inhib-itors. Donepezil (Aricept), rivastigmine (Exelon), and galantamine
(Reminyl) are cholinesterase inhibitors and have shown modest therapeutic
effects and temporarily slow the progress of dementia (Table 21.2). They have
no effect, however, on the overall course of the disease. Tacrine (Cognex) is
also a cholinesterase inhibitor; how-ever, it elevates liver enzymes in about
50% of clients using it. Lab tests to assess liver function are necessary every
1 to 2 weeks; therefore, tacrine is rarely prescribed. Memantine (Namenda) is
an NMDA receptor antagonist that can slow the progression of Alzheimer’s in the
moderate or severe stages (Facts and Comparisons, 2009).
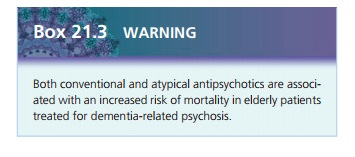
Clients with dementia demonstrate a broad range of behaviors that
can be treated symptomatically. Doses of medications are one half to two thirds
lower than usually prescribed. Antidepressants are effective for significant
depressive symptoms; however, they can cause delirium. SSRI antidepressants are
used since they have fewer side effects. Antipsychotics, such as haloperidol
(Haldol), olan-zapine (Zyprexa), risperidone (Risperdal), and quetiapine
(Seroquel), may be used to manage psychotic symptoms of delusions,
hallucinations, or paranoia, and other behav-iors, such as agitation or
aggression. The potential benefit of antipsychotics must be weighed with the
risks, such as an increased mortality rate, primarily from cardiovascular
complications. Due to this increased risk, the FDA has not approved
antipsychotics for dementia treatment, and there is a black box warning issued.
Lithium carbon-ate, carbamazepine (Tegretol), and valproic acid (Depak-ote)
help to stabilize affective lability and to diminish aggressive outbursts.
Benzodiazepines are used cautiously because they may cause delirium and can
worsen already compromised cognitive abilities (Neugroschl et al., 2005).
Related Topics