Chapter: Medical Surgical Nursing: Management of Patients With Neurologic Infections, Autoimmune Disorders, and Neuropathies
Meningitis - Infectious Neurologic Disorders
Infectious Neurologic Disorders
The infectious disorders
of the nervous system include meningitis, brain abscesses, various types of
encephalitis, and CreutzfeldtJakob and new-variant Creutzfeldt-Jakob disease.
The clinical manifestations, assessment, and diagnostic findings as well as the
medical and nursing management are related to the specific infectious process.
MENINGITIS
Meningitis is an
inflammation of the meninges, the protective membranes that surround the brain
and spinal cord. Meningitis is classified as aseptic or septic. In aseptic
meningitis, bacteria are not the cause of the inflammation; the cause is viral
or secondary to lymphoma, leukemia, or brain abscess. Septic meningitis refers
to meningitis caused by bacteria, most commonly Neisseria meningitidis, although
Haemophilus influenzae and Streptococcus pneumoniae are also causative agents.
Outbreaks of N.
meningitidis infection are most likely to occur in dense community groups, such
as college campuses and military installations. Though infections occur year
round, the peak incidence is in the winter and early spring. Factors that
increase the risk for developing bacterial meningitis include tobacco use and
viral upper respiratory infection because they increase the amount of droplet
production. Otitis media and mastoiditis increase the risk of bacterial
meningitis because the bacteria can cross the epithelium membrane and enter the
subarachnoid space. Persons with immune system deficiencies are also at greater
risk for developing bacterial meningitis. Between 1992 and 1996 there was a 28%
increase in the number of new cases reported in the 12-to-29-year-old age group
(Rosenstein, Perkins, Stephens et al.,2001). This increase focused attention on
the need to develop a vaccine for high-risk populations.
Pathophysiology
Meningeal infections
generally originate in one of two ways:through the bloodstream as a consequence
of other infections, or by direct extension, such as might occur after a
traumatic injury to the facial bones, or secondary to invasive procedures.
N. meningitidis
concentrates in the nasopharynx and is transmitted by secretion or aerosol
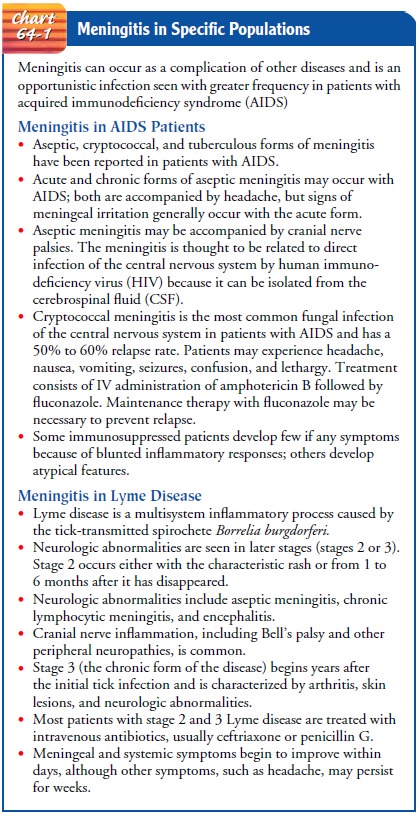
contamination. Bacterial or meningococcal meningitis also occurs as an
opportunistic infection in patients with acquired immunodeficiency syndrome
(AIDS) and as a complication of Lyme disease (Chart 64-1). S. pneumoniae is the
most frequent causative agent of bacterial meningitis associated with AIDS
(Rosenstein, Perkins, Stephens et al., 2001).
Once the causative
organism enters the bloodstream, it crosses the blood–brain barrier and causes
an inflammatory reaction in the meninges. Independent of the causative agent,
inflammation of the subarachnoid space and pia mater occurs. Since there is
little room for expansion within the cranial vault, the inflammation may cause
increased intracranial pressure. Cerebrospinal fluid (CSF) flows in the
subarachnoid space, where inflammatory cellular material from the affected
meningeal tissue enters and accumulates in the subarachnoid space, thereby
increasing the CSF cell count (Coyle, 1999).
The prognosis for
bacterial meningitis depends on the causative organism, the severity of the
infection and illness, and the timeliness of treatment. In acute fulminant
presentations there may be adrenal damage, circulatory collapse, and widespread
hemorrhages (Waterhouse-Friderichsen syndrome). This syndrome is the result of
endothelial damage and vascular necrosis caused by the bacteria. Complications
include visual impairment, deafness, seizures, paralysis, hydrocephalus, and
septic shock.
Clinical Manifestations
Headache and fever are
frequently the initial symptoms. Fever tends to remain high throughout the
course of the illness. The headache is usually severe as a result of meningeal
irritation. Meningeal irritation results in a number of other well-recognized
signs common to all types of meningitis:
·
Nuchal rigidity (stiff neck) is an early sign.
Any attempts at flexion of the head are difficult because of spasms in the
muscles of the neck. Forceful flexion causes severe pain.
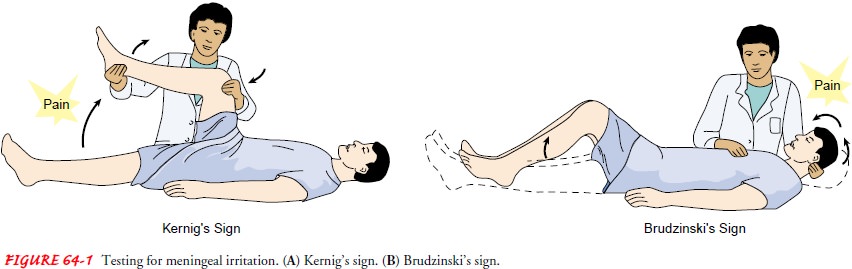
· Positive Kernig’s sign: When the patient is lying with the thigh flexed on the abdomen, the leg cannot be completely extended (Fig. 64-1).
·
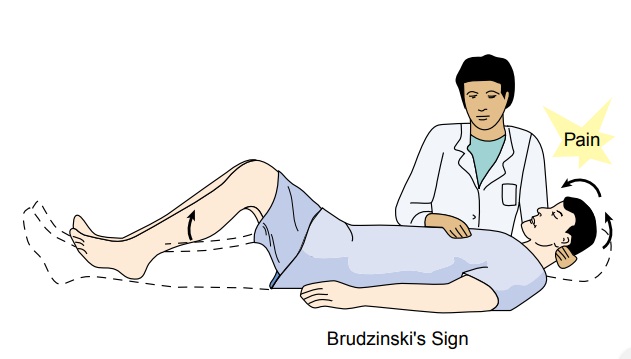
Positive Brudzinski’s sign:
When the patient’s neck is flexed, flexion of the knees and hips is produced;
when passive flex-ion of the lower extremity of one side is made, a similar
movement is seen in the opposite extremity (see Fig. 64-1).
·
Photophobia: extreme
sensitivity to light; this finding is common, although the cause is unclear.
A rash can be a striking feature of N. meningitidis infection, occurring in about half of patients with
this type of meningitis. Skin lesions develop, ranging from a petechial rash
with purpuric lesions to large areas of ecchymosis.
Disorientation and memory impairment are common early in
the course of the illness. The changes depend on the severity of the infection
as well as the individual response to the physiologic processes. Behavioral
manifestations are also common. As the illness progresses, lethargy, unresponsiveness,
and coma may develop.
Seizures and increased intracranial pressure (ICP) are
also as-sociated with meningitis. Seizures occur secondary to focal areas of
cortical irritability. Intracranial pressure increases secondary to
accumulation of purulent exudate. The initial signs of in-creased ICP include
decreased level of consciousness and focal motor deficits. If ICP is not
controlled, the uncus of the temporal lobe may herniate through the tentorium
into the brain stem. Brain stem herniation is a life-threatening event causing
cranial nerve dysfunction and depressing the centers of vital functions, such
as the medulla (Rowland, 2000).
A fulminating infection occurs in about 10% of patients
with meningococcal meningitis, with signs of overwhelming sep-ticemia: an
abrupt onset of high fever, extensive purpuric lesions (over the face and
extremities), shock, and signs of disseminated intravascular coagulopathy
(DIC). Death may occur within a few hours of onset of the infection.
Assessment and Diagnostic Findings
When the clinical presentation points to meningitis, diagnostic testing to identify the causative organism is conducted. Bacterial culture and Gram staining of CSF and blood are key diagnostic tests (Fischbach, 2002). The presence of polysaccharide antigen in CSF further supports the diagnosis of bacterial meningitis (Rosenstein et al., 2001).
Prevention
In 1971, the military
began vaccinating all new recruits against meningococcal meningitis, resulting
in a dramatic decrease in the incidence. Researchers suggested vaccination of
college freshman as surveillance studies indicated that freshmen living in
dormito-ries were at highest risk for developing meningococcal meningitis. At
this time vaccination is not required for college freshmen; however, the
American Academy of Pediatrics provides informa-tion to college freshmen and
their parents about the risk of dis-ease and the availability of vaccination
(Bruce et al., 2001; Centers for Disease Control and Prevention [CDC], 2000).
People in close contact
with patients with meningococcal meningitis should be treated with
antimicrobial chemopro-phylaxis using rifampin (Rifadin), ciprofloxacin
hydrochloride (Cipro), or ceftriaxone sodium (Rocephin) (CDC, 2000). Ther-apy should
be started as soon as possible after contact; a delay in the initiation of
therapy will limit the effectiveness of the pro-phylaxis (Rosenstein et al.,
2001). Vaccination should also be considered as an adjunct to antibiotic
chemoprophylaxis for any-one living with a person who develops meningococcal
infection. Vaccination for children and at-risk adults should be encouraged to
avoid meningitis caused by H. influenzae
and S. pneumoniae.
Medical Management
Successful outcomes depend on the early administration of
an anti-biotic that crosses the blood–brain barrier into the subarachnoid space
in sufficient concentration to halt the multiplication of bac-teria. Penicillin
antibiotics (eg, ampicillin, piperacillin) or one of the cephalosporins (eg,
ceftriaxone sodium, cefotaxime sodium) may be used. Vancomycin hydrochloride
alone or in combina-tion with rifampin may be used if resistant strains of
bacteria are identified. High doses of the appropriate antibiotic are
adminis-tered intravenously.
Dexamethasone has been shown to be beneficial as adjunct
therapy in the treatment of acute bacterial meningitis and in pneumococcal
meningitis if given 15 to 20 minutes before the first dose of antibiotic and
every 6 hours for the next 4 days. Studies indicate that dexamethasone improves
the outcome in adults and does not increase the risk of gastrointestinal
bleeding (de Gans & van de Beek, 2002).
Dehydration and shock are treated with fluid volume
ex-panders. Seizures, which may occur in the early course of the dis-ease, are
controlled with phenytoin (Dilantin). Increased ICP is treated as necessary.
Nursing Management
The patient may be
critically ill; therefore, so many of the nurs-ing interventions are
collaborative with those of the physician, respiratory therapist, and other
members of the health care team. The patient’s prognosis may depend on the
supportive care provided.
Neurologic status and
vital signs are continually assessed. Pulse oximetry and arterial blood gas
values are used to quickly identify the need for respiratory support as the
increasing ICP compromises the brain stem. Insertion of a cuffed endotracheal
tube (or tracheotomy) and mechanical ventilation may be neces-sary to maintain
adequate tissue oxygenation.
Arterial blood pressures
are monitored to assess for incipient shock, which precedes cardiac or
respiratory failure. Rapid intra-venous (IV) fluid replacement may be
prescribed, but care is takento prevent fluid overload. Fever also will
increase the workload of the heart and cerebral metabolism. ICP will increase
in response to increased cerebral metabolic demands. Therefore, measures are
taken to reduce body temperature as quickly as possible.
Other important components of nursing care include:
·
Monitoring body weight, serum
electrolytes, and urine vol-ume, specific gravity, and osmolality, especially
if the syn-drome of inappropriate antidiuretic hormone (SIADH) secretion is
suspected
·
Protecting the patient from
injury secondary to seizure ac-tivity or altered level of consciousness
·
Preventing complications
associated with immobility, such as pressure ulcers and pneumonia
·
Instituting droplet
precautions until 24 hours after the ini-tiation of antibiotic therapy (oral
and nasal discharge is con-sidered infectious)
Any sudden, critical illness can be devastating to the
family. Because the patient’s condition is often critical and the progno-sis
guarded, the family needs to be informed about the patient’s condition and
permitted to see the patient at intervals, even though the priority is to
address the patient’s need for immediate and intensive treatment. An important
aspect of the nurse’s role is to support the patient and to assist the family
in identifying others who can be supportive to them during the crisis.
Related Topics