Chapter: Medical Surgical Nursing: Management of Patients With Neurologic Infections, Autoimmune Disorders, and Neuropathies
BellŌĆÖs Palsy - Cranial Nerve Disorders
BELLŌĆÖS PALSY
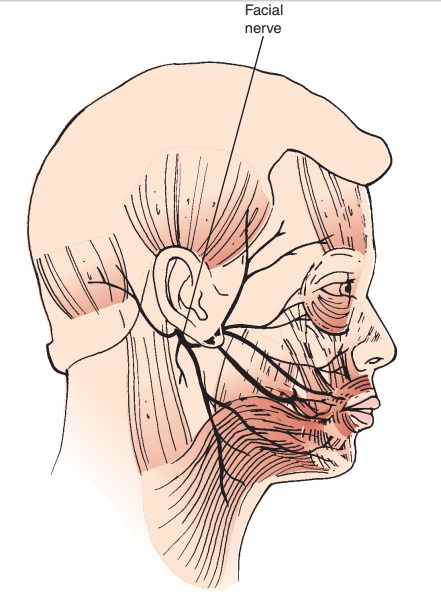
BellŌĆÖs palsy (facial paralysis) is due to unilateral inflammation of the seventh cranial nerve, which results in weakness or paralysis of the facial muscles on the affected side (Fig. 64-8). The cause is unknown, although possible causes may include vascular ischemia, viral disease (herpes simplex, herpes zoster), autoimmune disease, or a combination of all of these factors. The incidence is 13 to 34 cases per 100,000; it increases with age and among pregnant women in the third trimester (Campbell & Brundage, 2002; Shmorgun, Chan & Ray, 2002).
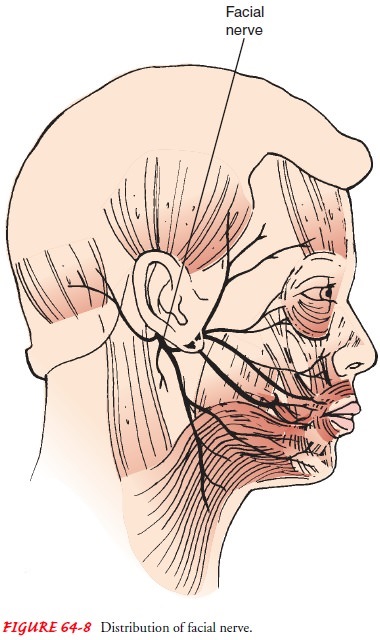
BellŌĆÖs palsy is considered by some to represent a type of
pres-sure paralysis. The inflamed, edematous nerve becomes com-pressed to the
point of damage, or its nutrient vessel is occluded, producing ischemic
necrosis of the nerve. There is distortion of the face from paralysis of the
facial muscles; increased lacrimation (tearing); and painful sensations in the
face, behind the ear, and in the eye. The patient may experience speech
difficulties and may be unable to eat on the affected side because of weakness
or paralysis of the facial muscles.
Management
The objectives of treatment are to maintain the muscle
tone of the face and to prevent or minimize denervation. The patient should be
reassured that no stroke has occurred and that sponta-neous recovery occurs
within 3 to 5 weeks in most patients.
Corticosteroid therapy (prednisone) may be prescribed to
re-duce inflammation and edema; this reduces vascular compression and permits
restoration of blood circulation to the nerve. Early administration of
corticosteroid therapy appears to diminish the severity of the disease, relieve
the pain, and prevent or minimize denervation.
Facial pain is controlled with analgesic agents. Heat may
be applied to the involved side of the face to promote comfort and blood flow
through the muscles.
Electrical stimulation may be applied to the face to
prevent muscle atrophy. Although most patients recover with conserva-tive
treatment, surgical exploration of the facial nerve may be in-dicated in
patients who are suspected of having a tumor or for surgical decompression of
the facial nerve and for surgical treat-ment of a paralyzed face.
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care.
While the paralysis lasts, the in-volved eye must
be protected. Frequently, the eye does not close completely and the blink
reflex is diminished, so the eye is vul-nerable to dust and foreign particles.
Corneal irritation and ul-ceration may occur if the eye is unprotected.
Distortion of the lower lid alters the proper drainage of tears. To prevent
injury, the eye should be covered with a protective shield at night. The eye
patch may abrade the cornea, however, because there is some difficulty in
keeping the partially paralyzed eyelids closed. The application of eye ointment
at bedtime causes the eyelids to ad-here to one another and remain closed
during sleep. The patient can be taught to close the paralyzed eyelid manually
before going to sleep. Wrap-around sunglasses or goggles may be worn to
de-crease normal evaporation from the eye.
Continuing Care.
When the sensitivity of
the nerve to touch de-creases and the patient can tolerate touching the face,
the nurse can suggest massaging the face several times daily, using a gentle
upward motion, to maintain muscle tone. Facial exercises, such as wrinkling the
forehead, blowing out the cheeks, and whistling, may be performed with the aid
of a mirror in an effort to prevent muscle atrophy. Exposure of the face to
cold and drafts is avoided.
Related Topics