Chapter: Medical Surgical Nursing: Management of Patients With Neurologic Infections, Autoimmune Disorders, and Neuropathies
Nursing Process: The Patient With Multiple Sclerosis
NURSING PROCESS:THE PATIENT WITH
MULTIPLE SCLEROSIS
Assessment
Nursing assessment
addresses actual and potential problems as-sociated with the disease, including
neurologic problems, sec-ondary complications, and the impact of the disease on
the patient and family. The patient’s movements and walking are ob-served to
determine if there is danger of falling. Assessment of function is carried out
both when the patient is well rested and when fatigued. The patient is assessed
for weakness, spasticity, vi-sual impairment, incontinence, and disorders of
swallowing and speech. Additional areas of assessment include the following:
How has MS affected the patient’s lifestyle? How well is the pa-tient coping? What
would the patient like to do better?
Diagnosis
NURSING DIAGNOSES
Based on the assessment data, the patient’s major nursing
diag-noses may include the following:
·
Impaired physical mobility
related to weakness, muscle paresis, spasticity
·
Risk for injury related to
sensory and visual impairment
·
Impaired urinary and bowel
elimination (urgency, frequency, incontinence, constipation) related to nervous
system dysfunction
·
Impaired speech and swallowing
related to cranial nerve involvement
·
Disturbed thought processes
(loss of memory, dementia, euphoria) related to cerebral dysfunction
·
Ineffective individual coping
related to uncertainty of course of MS
·
Impaired home maintenance
management related to phys-ical, psychological, and social limits imposed by MS
·
Potential for sexual
dysfunction related to spinal cord in-volvement or psychological reactions to
condition
Planning and Goals
The major goals for the patient may include promotion of
phys-ical mobility, avoidance of injury, achievement of bladder and bowel
continence, promotion of speech and swallowing mecha-nisms, improvement of
cognitive function, development of coping strengths, improved home maintenance
management, and adap-tation to sexual dysfunction.
Nursing Interventions
An individualized program of physical therapy,
rehabilitation, and education is combined with emotional support. The nursing
interventions include face-to-face and telephone interactions that address
patient education to enable the person with MS to deal with the physiologic,
social, and psychological problems that ac-company chronic disease (Madonna
& Keating, 1999).
PROMOTING PHYSICAL MOBILITY
Relaxation and
coordination exercises promote muscle efficiency. Progressive resistive
exercises are used to strengthen weak muscles because diminishing muscle
strength is often significant in MS.
Exercises
Walking improves the gait, particularly when there is
loss of po-sition sense of the legs and feet. If certain muscle groups are
irre-versibly affected, other muscles can be trained to take over their
actions. Instruction in the use of assistive devices may be needed to ensure
their correct and safe use.
Minimizing Spasticity and Contractures
Muscle spasticity is
common and, in its later stages, is character-ized by severe adductor spasm of
the hips with flexor spasm of the hips and knees. If this is not relieved,
fibrous contractures of these joints with resultant pressure ulcers over the
sacrum and hips (due to diminished sensation and the inability to position the
patient properly) occur. Warm packs may be beneficial, but hot baths should be
avoided because of risk for burn injury secondary to sensory loss and
increasing symptoms that may occur with an elevation of the body temperature.
Daily exercises for
muscle stretching are prescribed to mini-mize joint contractures. Special
attention is given to the ham-strings, gastrocnemius muscles, hip adductors,
biceps, and wrist and finger flexors. Muscle spasticity is common and
interferes with normal function. A stretch–hold–relax routine is helpful for
relaxing and treating muscle spasticity. Swimming and stationary bicycling are
useful, and progressive weight-bearing can relieve spasticity in the legs. The
patient should not be hurried in any of these activities because this often increases
spasticity.
Activity And Rest
The patient is
encouraged to work to a point just short of fatigue. Very strenuous physical
exercise is not advisable because it raises the body temperature and may
aggravate symptoms. The patientis advised to take frequent
short rest periods, preferably lying down.Extreme fatigue may contribute to the
exacerbation of symptoms.
Minimizing Effects of Immobility
Because of the decrease in physical activity that often
occurs with MS, complications associated with immobility, including pres-sure
ulcers, expiratory muscle weakness, and accumulation of bronchial secretions,
need to be considered and steps taken to prevent them. Measures to prevent such
complications include assessment and maintenance of skin integrity and coughing
and deep-breathing exercises.
PREVENTING INJURY
If motor dysfunction
causes problems of incoordination and clumsiness, or if ataxia is apparent, the
patient is at risk for falling. To overcome this disability, the patient is
taught to walk with feet wide apart to widen the base of support and to
increase walking stability. If there is loss of position sense, the patient is
taught to watch the feet while walking. Gait training may require assistive
devices (walker, cane, braces, crutches, parallel bars) and instruc-tion about
their use by a physical therapist. If the gait remains in-efficient, a
wheelchair or motorized scooter may be the solution. The occupational therapist
is a valuable resource person in sug-gesting and securing aids to promote independence.
If incoordi-nation is a problem and tremor of the upper extremities occurs when
voluntary movement is attempted (intention tremor), weighted bracelets or wrist
cuffs are helpful. The patient is trained in transfer and activities of daily
living.
Because sensory loss may
occur in addition to motor loss, pres-sure ulcers are a continuing threat to
skin integrity. Confinement to a wheelchair increases the risk.
ENHANCING BLADDER AND BOWEL CONTROL
Generally, bladder
symptoms fall into the following categories: (1) inability to store urine
(hyperreflexic, uninhibited); (2) inabil-ity to empty the bladder
(hyporeflexic, hypotonic); and (3) a mix-ture of both types. The patient with
urinary frequency, urgency, or incontinence requires special support. The
sensation of the need to void must be heeded immediately, so the bedpan or
uri-nal should be readily available. A voiding time schedule is set up (every
1.5 to 2 hours initially, with gradual lengthening of the interval). The
patient is instructed to drink a measured amount of fluid every 2 hours and
then attempt to void 30 minutes after drinking. Using a timer or wristwatch
with an alarm may be help-ful for the patient who does not have enough
sensation to signal the need to empty the bladder. The nurse encourages the
patient to take the prescribed medications to treat bladder spasticity because
this allows greater independence. Intermittent self-catheterization has been
successful in maintaining bladder control in patients with MS. If the female
patient has permanent urinary in-continence, urinary diversion procedures may
be considered. The male patient may wear a condom appliance for urine
collection.
Bowel problems include
constipation, fecal impaction, and in-continence. Adequate fluids, dietary fiber,
and a bowel-training program are frequently effective in solving these
problems.
MANAGING SPEECH AND SWALLOWING DIFFICULTIES
When the cranial nerves
controlling the mechanisms of speech and swallowing are involved, dysarthrias
(defects of articulation) marked by slurring, low volume of speech, and
difficulties in phonation may occur. Swallowing disturbances (dysphagia) may also occur. A speech
therapist evaluates speech and swallowing and instructs the patient, family,
and health team members about strategies to compensate for speech and
swallowing problems. The nurse reinforces this instruction and encourages the
patient and family to adhere to the plan. Impaired swallowing increases the
patient’s risk for aspiration; therefore, strategies (eg, having suction
apparatus available, careful feeding, proper positioning for eating) are needed
to reduce that risk (Galvan, 2001).
IMPROVING SENSORY AND COGNITIVE FUNCTION
Measures may be taken if
visual defects (the cranial nerves affecting vision may be affected by MS) or
changes in cognitive status occur.
Vision
An eye patch or a covered eyeglass lens may be used to
block vi-sual impulses of one eye when the patient has diplopia (double
vision). Prism glasses may be helpful for the bedridden patient who is having
difficulty reading in the supine position. People unable to read regular-print
materials are eligible for the free talk-ing book services of the Library of
Congress or may obtain large-type books from local libraries.
Cognition and Emotional Responses
Cognitive impairment and
emotional lability may occur early in MS in some patients and may impose
numerous stresses on the patient and family. Some patients with MS are
forgetful and easily distracted and may exhibit emotional lability.
Patients adapt to illness in a variety of ways, which may
in-clude denial, depression, withdrawal, and hostility. Emotional support
assists patients and their families to adapt to the changes and uncertainties
associated with MS and to cope with the dis-ruption in their lives. The patient
is assisted to set meaningful and realistic goals to achieve a sense of
purpose, to remain as active as possible, and to keep up social interests and
activities. Hobbies may help the patient’s morale and provide satisfying
interests if the disease progresses to the stage in which formerly enjoyed
ac-tivities can no longer be pursued.
The family should be
made aware of the nature and degree of cognitive impairment. The environment is
kept structured, and lists and other memory aids are used to help the patient
with cog-nitive changes to maintain a daily routine. The occupational
ther-apist can be helpful in formulating a structured daily routine.
Strengthening Coping Mechanisms
The diagnosis of MS is
always distressing to the patient and fam-ily. They need to know that no two
patients with MS have iden-tical symptoms or courses of illness. Although some
patients do experience significant disability early, others have a near-normal
life span with minimal disability. Some families, however, face overwhelming
frustrations and problems. MS affects people who are often in a productive
stage of life and concerned about career and family responsibilities. Family
conflict, disintegration, sepa-ration, and divorce are not uncommon. Often,
very young family members assume the responsibility of caring for a parent with
MS. Nursing interventions in this area include alleviating stress and making
appropriate referrals for counseling and support to min-imize the adverse
effects of dealing with chronic illness.
The nurse, mindful of these complex problems, initiates
home care and coordinates a network of services, including social ser-vices,
speech therapy, physical therapy, and homemaker services. To strengthen the
patient’s coping skills, as much information as possible is provided. People
who live with chronic illness need an updated list of the assistive devices,
services, and resources that are available.
Coping through problem solving involves helping the
patient define the problem and develop alternatives for its management. Careful
planning and maintaining flexibility and a hopeful atti-tude are useful for
psychological and physical adaptation.
IMPROVING SELF-CARE ABILITIES
MS can affect every
facet of daily living. After certain abilities are lost, they are often
impossible to regain. Physical function may vary from day to day. Modifications
that allow independence in self-care should be implemented (eg, assistive
eating devices, raised toilet seat, bathing aids, telephone modifications, long-handled
comb, tongs, modified clothing). Physical and emotional stresses should be
avoided as much as possible because these may worsen symptoms and impair
performance. Exposure to heat in-creases fatigue and muscle weakness, so air
conditioning in at least one room is recommended. Exposure to extreme cold may
in-crease spasticity.
PROMOTING SEXUAL FUNCTIONING
Patients with MS and their partners face problems that
interfere with sexual activity, arising not only as a direct consequence of
nerve damage but also from psychological reactions to the disease. Easy
fatigability, conflicts arising from dependency and depres-sion, emotional
lability, loss of self-esteem, and feelings of low self-worth compound the
problem. Erectile and ejaculatory dis-orders in men and orgasmic dysfunction
and adductor spasms of the thigh muscles in women can make sexual intercourse
difficult or impossible. Bladder and bowel incontinence and urinary tract
infections add to the difficulties.
An experienced sexual counselor helps bring into focus
the patient’s or partner’s sexual resources and suggests relevant in-formation
and supportive therapy (Sipski & Alexander, 1997). Sharing and
communicating feelings, planning for sexual activ-ity (to minimize the effects
of fatigue), and exploring alternative methods of sexual expression may open up
a wide range of sexual enjoyment and experiences.
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care
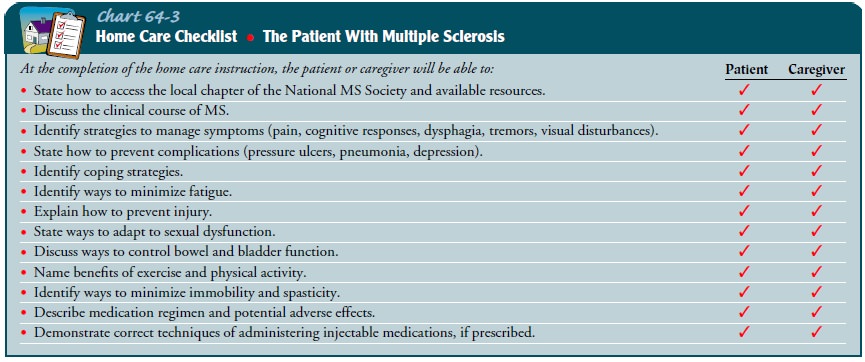
As the disease
progresses, the patient and family need to learn new strategies to maintain
optimal independence. Teaching of new self-care techniques may be initiated in
the hospital or clinic set-ting and reinforced in the home. Teaching about
self-care may address the use of assistive devices, self-catheterization, and
ad-ministration of medications that affect the course of the disease or treat
complications. Although the disease-modifying medica-tions (the “ABC and R
medications”) may slow the progression of disease and disability in many
persons with MS, they are not effective in all patients. Patients who receive
these medications will require teaching and support, while those unable to take
them or for whom the medications have not been effective need continued support
and assistance in coping with this reality. Exercises that enable the patient
to continue some form of activ-ity or that maintain or improve swallowing,
speech, or respiratory function may be taught to the patient and family (Chart
64-3).
Continuing Care
After discharge, the home care nurse often provides teaching and reinforcement of these new techniques in the patient’s home.
Nurses in the home setting assess for changes in the patient’s physical and emotional status, provide physical care to
the patient if required, coordinate outpatient services and resources, and
en-courage health promotion, appropriate health screenings, and adaptation. If
changes in the disease or its course are noted, the home care nurse encourages
the patient to contact the primary care provider because treatment of an acute
exacerbation or new problem may be indicated. Continuing health care and
follow-up are recommended.
The patient with MS is encouraged to contact the local c
hapter of the National Multiple Sclerosis Society for services, publica-tions,
and contact with others with MS. Local c-hapters also pro-vide direct services
to patients. Through group participation, the patient has an opportunity to
meet others with similar problems, to share experiences, and to learn self-help
methods in a social environment.
Evaluation
EXPECTED PATIENT OUTCOMES
Expected patient outcomes may include:
1) Improved
physical mobility
a) Participates
in gait-training and rehabilitation program
b) Establishes
a balanced program of rest and exercise
c) Uses
assistive devices correctly and safely
2) Is
free of injury
a) Uses
visual cues to compensate for decreased sense of touch or position
b) Asks
for assistance when necessary
3) Attains
or maintains control of bladder and bowel patterns
a) Monitors self for urine retention and employs intermit-tent self-catheterization technique, if indicated
b. Identifies the signs and symptoms of urinary
tract infection
Maintains adequate fluid
and fiber intake
4) Participates
in strategies to improve speech and swallowing
a) Practices
exercises recommended by speech therapist
b) Maintains
adequate nutritional intake without aspiration
5) Compensates
for altered thought processes
a) Uses
lists and other aids to compensate for memory losses
b) Discusses
problems with trusted advisor or friend
c) Substitutes
new activities for those that are no longer possible
6) Demonstrates
effective coping strategies
a) Maintains
sense of control
b) Modifies
lifestyle to fit goals and limitations
c) Verbalizes
desire to pursue goals and developmental tasks of adulthood
d) Adheres
to plan for home maintenance management
e) Uses
appropriate self-care techniques to maintain in-dependence
f) Engages
in health promotion activities and health screen-ings as appropriate
7) Adapts
to changes in sexual function
a) Is
able to discuss problem with partner and appropriate health professional
b) Identifies
alternate means of sexual expression
Related Topics