Chapter: Medical Surgical Nursing: Management of Patients With Neurologic Infections, Autoimmune Disorders, and Neuropathies
Trigeminal Neuralgia (Tic Douloureux) - Cranial Nerve Disorders
TRIGEMINAL NEURALGIA (TIC DOULOUREUX)
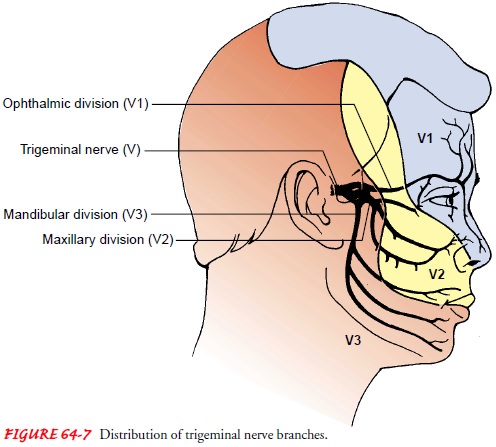
Trigeminal neuralgia is
a condition of the fifth cranial nerve char-acterized by paroxysms of pain in
the area innervated by any of the three branches, but it most commonly occurs
in the second and third branches of the trigeminal nerve (Maloni, 2000) (Fig.
64-7). The pain ends as abruptly as it starts and is described as a uni-lateral
shooting and stabbing sensation. The unilateral nature of the pain is an
important diagnostic characteristic (Preul, 2001). Associated involuntary
contraction of the facial muscles can cause sudden closing of the eye or a
twitch of the mouth, hence the name tic
douloureux (painful twitch). The cause is not certain, but chronic
compression or irritation of the trigeminal nerve or degenerative changes in
the gasserian ganglion are suggested causes. Vascular pressure from structural
abnormalities (loop of an artery) encroaching on the trigeminal nerve,
gasserian ganglion, or root entry zone has also been suggested as a cause.
Trigeminal neuralgia is 400 times more common in patients
with MS than in the general population. The pain is more often cyclic and
affects men with MS at a higher rate than women with MS (Maloni, 2000).
Early attacks, appearing most often in the fifth decade
of life, are usually mild and brief. Pain-free intervals may be measured in
terms of minutes, hours, days, or longer. With advancing years, the painful
episodes tend to become more frequent and agonizing. The patient lives in
constant fear of attacks.
Paroxysms can occur with
any stimulation of the terminals of the affected nerve branches, such as
washing the face, shaving, brushing the teeth, eating, and drinking. A draft of
cold air and direct pressure against the nerve trunk may also cause pain.
Certain areas are called trigger points because the slightest touch immediately
starts a paroxysm or episode. To avoid stimulating these areas, patients with
trigeminal neuralgia try not to touch or wash their faces, shave, chew, or do
anything else that might cause an attack. These behaviors are a clue to
diagnosis.
Medical Management
PHARMACOLOGIC THERAPY
Antiseizure agents, such as carbamazepine (Tegretol), relieve pain in most patients with trigeminal neuralgia by reducing the trans-mission of impulses at certain nerve terminals. Carbamazepine is taken with meals. Serum levels must be monitored to avoid tox-icity in patients who require high doses to control the pain. Side effects include nausea, dizziness, drowsiness, and aplastic anemia. The patient is monitored for bone marrow depression during long-term therapy. Gabapentin (Neurontin) and baclofen (Lioresal) are also used for pain control. If pain control is still not achieved, phenytoin (Dilantin) may be used as adjunctive therapy (Rowland, 2000).
Alcohol or phenol
injection of the gasserian ganglion and pe-ripheral branches of the trigeminal
nerve relieves pain for several months. However, the pain returns with nerve
regeneration.
SURGICAL MANAGEMENT
When these methods fail to relieve pain, a number of
surgical options are available. The choice of procedure depends on the
patient’s preference and health status.
Microvascular Decompression of the Trigeminal Nerve.
An
in-tracranial approach can be used to decompress the trigeminal nerve. The pain
may be caused by vascular compression of the entry zone of the trigeminal root
by an arterial loop and occasionally by a vein. With the aid of an operating
microscope, the artery loop is lifted from the nerve to relieve the pressure,
and a small prosthetic device is inserted to prevent recurrence of im-pingement
on the nerve. This procedure relieves facial pain while preserving normal
sensation, but it is a major procedure, involving a craniotomy. The postoperative
management is the same as for other intracranial surgeries.
Percutaneous Radiofrequency Trigeminal Gangliolysis.
Percu-taneous radiofrequency interruption of the gasserian ganglion, in which the small unmyelinated and thinly myelinated fibers that conduct pain are thermally destroyed, is the surgical procedure of choice for trigeminal neuralgia (Tronnier, Rasche, Hamer et al., 2001). Use of stereotactic MRI for identification of the trigemi-nal nerve followed by gamma knife radiosurgery is being used at some centers with good results (Maesawa et al., 2001).
Under local anesthesia,
the needle is introduced through the cheek on the affected side. Under
fluoroscopic guidance, the needle electrode is guided through the foramen
magnum into the gasserian ganglion. The divisions of the gasserian ganglion
(mandibular, maxillary, and ophthalmic) are encountered se-quentially. The
nerve is stimulated with a small current while the patient is awake. The
patient reports when a tingling sensation is felt. When the electrode needle is
in the desired position, the pa-tient is anesthetized briefly and a
radiofrequency current (heating current to destroy the nerve) is passed in a
controlled manner to injure the trigeminal ganglion and rootlets thermally. The
patient is then awakened from the anesthesia and examined for sensory deficits.
This is repeated until the desired effect is achieved. The procedure takes less
than 1 hour and provides permanent pain re-lief in most patients. Touch and
proprioceptive functions are left intact.
In the patient with trigeminal neuralgia and MS who is
re-fractory to medical pain management, the surgical treatment of choice is
trigeminal rhizotomy (Maloni, 2000).
Nursing Management
PREVENTING PAIN
Preoperative management
of a patient with trigeminal neuralgia occurs mostly on an outpatient basis and
includes recognizing factors that may aggravate excruciating facial pain, such
as food that is too hot or too cold or jarring the patient’s bed or chair. Even
washing the face, combing the hair, or brushing the teeth may produce acute
pain. The nurse can assist the patient in pre-venting or reducing this pain by
providing instructions about pre-ventive strategies. Providing cotton pads and
room-temperature water for washing the face, instructing the patient to rinse
with mouthwash after eating when tooth-brushing causes pain, and performing
personal hygiene during pain-free intervals are all ef-fective strategies. The
patient is instructed to take food and flu-ids at room temperature, to chew on
the unaffected side, and to ingest soft foods. The nurse recognizes that
anxiety, depression, and insomnia often accompany chronic painful conditions
and uses appropriate interventions and referrals.
PROVIDING POSTOPERATIVE CARE
Postoperative neurologic
assessments are conducted to evaluate the patient for facial motor and sensory
deficits in each of the three branches of the trigeminal nerve. If the surgery
results in sensory deficits to the affected side of the face, the patient is
in-structed not to rub the eye, because pain will not be felt if there is
injury. The eye is assessed for irritation or redness. Artificial tears may be
prescribed to prevent dryness in the affected eye. The patient is cautioned not
to chew on the affected side until numb-ness has diminished. The patient is
observed carefully for any dif-ficulty in eating and swallowing foods of
different consistency.
Related Topics