Chapter: Medical Surgical Nursing: Management of Patients With Neurologic Infections, Autoimmune Disorders, and Neuropathies
Multiple Sclerosis - Autoimmune Processes
Autoimmune
Processes
Autoimmune nervous system disorders include multiple
sclero-sis, myasthenia gravis, and Guillain-Barré syndrome.
MULTIPLE SCLEROSIS
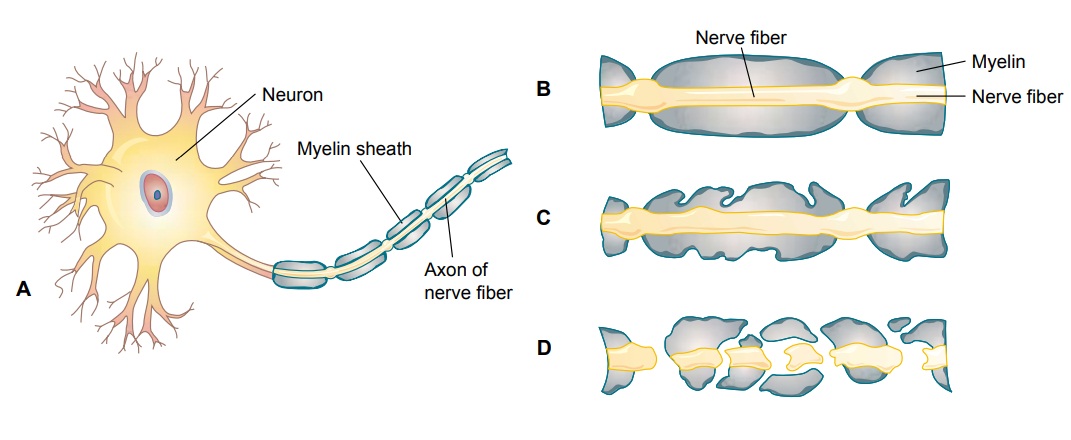
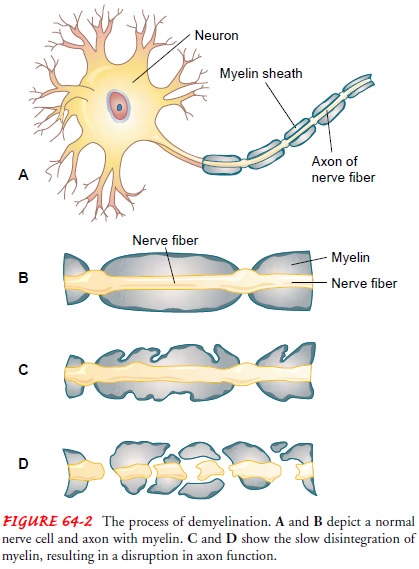
Multiple sclerosis (MS) is an immune-mediated progressive
de-myelinating disease of the CNS. Demyelination refers to the de-struction of
myelin, the fatty and protein material that surrounds certain nerve fibers in
the brain and spinal cord; it results in im-paired transmission of nerve
impulses (Fig. 64-2). MS typically presents in young adults ages 20 to 40, and
it affects women more frequently than men (Boyden, 2000).
The cause of MS is an
area of ongoing research. Autoimmune activity results in demyelination, but the
sensitized antigen has not been identified. Multiple factors play a role in the
initiation of the immune process. Geographic prevalence is highest in northern
Europe, southern Australia, the northern United States, and southern Canada
(Noseworthy, Lucchinetti, Rodriguez et al., 2000). It is believed that an
environmental exposure at a young age may play a role in the development of MS
later in life.
Genetic predisposition is indicated by the presence of a spe-cific cluster (haplotype) of human leukocyte antigens (HLA) on the cell wall. The presence of this haplotype may promote sus-ceptibility to factors, such as viruses, that trigger the autoimmune response activated in MS. A specific virus capable of initiating the autoimmune response has not been identified.
It is believed that DNA on the virus mimics the amino acid
sequence of myelin, resulting in an immune system cross-reaction in the
presence of a defective immune system (Boyden, 2000).
Pathophysiology
Sensitized T cells
typically cross the blood–brain barrier; their function is to check the CNS for
antigens and then leave. In MS, the sensitized T cells remain in the CNS and
promote the infil-tration of other agents that damage the immune system. The
im-mune system attack leads to inflammation that destroys myelin (which
normally insulates the axon and speeds the conduction of impulses along the
axon) and oligodendroglial cells that produce myelin in the CNS.
Plaques of sclerotic
tissue appear on demyelinated axons, fur-ther interrupting the transmission of
impulses. Demyelination interrupts the flow of nerve impulses and results in a
variety of manifestations, depending on which nerves are affected.
De-myelinated axons are scattered irregularly throughout the CNS (Fig. 64-3).
The areas most frequently affected are the optic nerves, chiasm, and tracts;
the cerebrum; the brain stem and cerebellum; and the spinal cord. Eventually
the axons themselves begin to de-generate, resulting in permanent and
irreversible damage (Bashir & Whitaker, 2002; Halper, 2001).
Clinical Manifestations
The course of MS may assume many different patterns (Fig. 64-4). In some patients, the disease follows a benign course, with a normal life span and symptoms so mild that patients do not seek health care and treatment.
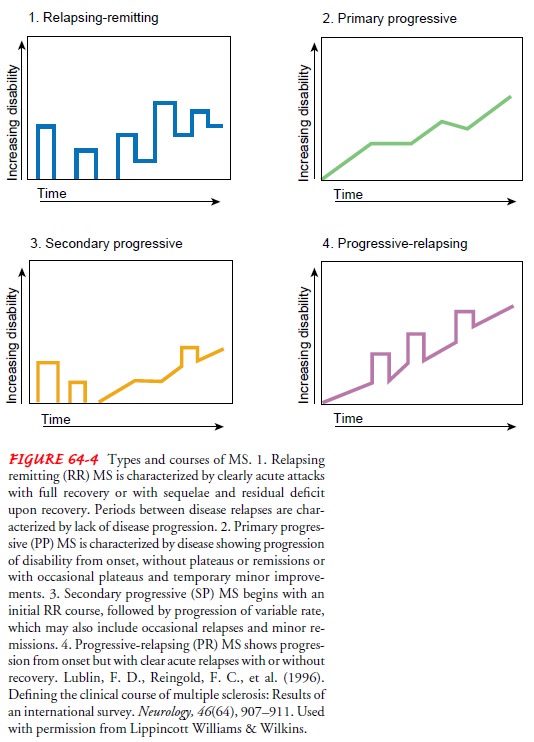
Eighty percent to 85% of cases of MS begin with a relapsing–remitting course,
with complete recovery between clearly defined symptomatic exacerbations
(Noseworthy et al., 2000). This form of the disease does not progress between
relapses, although the majority of cases with this initial type of course
change to a secondary-progressive course after some years (Halper, 2001).
Secondary-progressive MS begins as relapsing– remitting disease but changes to
a course in which there is not full recovery but rather continued progression
between defined re-lapses. Ten percent to 20% percent of patients have a
primary progressive course (Noseworthy et al., 2000; Halper, 2001), in which
symptoms progress throughout the disease, with increasing disability. Primary
progressive MS is characterized by continuous decline, with the potential
development of quadriparesis, cogni-tive dysfunction, visual loss, and brain
stem syndromes.
The signs and symptoms
of MS are varied and multiple, re-flecting the location of the lesion (plaque)
or combination of lesions. The primary symptoms most commonly reported are
fatigue, depression, weakness, numbness, difficulty in coordina-tion, loss of
balance, and pain. Visual disturbances due to lesions in the optic nerves or
their connections may include blurring of vision, diplopia, patchy blindness (scotoma), and total blindness.
Fatigue impairs optimal function throughout the course of the disease. Fatigue is exacerbated when febrile illness, environ-mental temperature, hot showers, and normal circadian rhythms during the afternoon elevate body temperature. Depression may relate to the pathophysiology or may occur as a reaction to the diagnosis. Suicide as the cause of death occurs 7.5 times more fre-quently among persons diagnosed with MS than among the age-matched general population. If suicide occurs, it is likely to occur within the first 5 years of diagnosis (Walther & Hohlfeld, 1999).
Pain occurs in 66% of patients with MS. Pain may be due
to de-myelination of pain fibers, mechanical stress on muscles, bones, and
joints due to disability, or treatment measures (Maloni, 2000).
Spasticity (muscle
hypertonicity) of the extremities and lossof the abdominal reflexes are due to
involvement of the main motor pathways (pyramidal tracts) of the spinal cord.
Disruption of the sensory axons may produce sensory dysfunction (paresthesias,
pain). Cognitive and psychosocial problems may reflect frontal or parietal lobe
involvement; some degree of cognitive change (eg, memory loss, decreased
concentration) occurs in about half of pa-tients, but severe cognitive changes
with dementia (progressive organic mental disorder) are rare. Involvement of
the cerebellum or basal ganglia can produce ataxia (impaired coordination of
movements) and tremor. Loss of the control connections between the cortex and
the basal ganglia may occur and cause emotional lability and euphoria. Bladder,
bowel, and sexual dysfunctions are common.
Secondary complications
of MS include urinary tract infections, constipation, pressure ulcers,
contracture deformities, dependent pedal edema, pneumonia, reactive depression,
and decreased bone mass. Emotional, social, marital, economic, and vocational
prob-lems may also be a consequence of the disease.
Exacerbations and
remissions are characteristic of MS. During exacerbations, new symptoms appear
and existing ones worsen; dur-ing remissions, symptoms decrease or disappear.
Relapses may be associated with periods of emotional and physical stress. MRI stud-ies
demonstrate that many plaques do not produce serious symp-toms; however, the
disease may be very active, as demonstrated by MRI. There also is evidence that
remyelination actually occurs in some patients.
Assessment and Diagnostic Findings
MRI is the primary
diagnostic tool for visualizing plaques, docu-menting disease activity, and
evaluating the effect of treatment. Electrophoresis of CSF identifies the
presence of oligoclonal banding (several bands of immunoglobulin G bonded
together,indicating an immune system abnormality). Evoked
potential studies can help define the extent of the disease process and
mon-itor changes. Underlying bladder dysfunction is diagnosed by urodynamic
studies. Neuropsychological testing may be indi-cated to assess cognitive
impairment. A sexual history helps to identify changes in sexual function.
Gerontologic Considerations
Due to improved
treatment and an increase in the average life span for patients with MS, more
individuals are living to become elderly. These patients may have chronic
health problems for which they may be taking additional medications that could
in-teract with medications prescribed for MS. The absorption, dis-tribution,
metabolism, and excretion of medications are altered in the elderly as a result
of age-related changes in renal and liver functions. Therefore, the elderly
must be monitored closely for adverse and toxic effects of MS medications and
for osteoporosis (particularly with frequent corticosteroid use, which may be
re-quired for exacerbations). The cost of medications could lead to poor
adherence to the prescribed regimen in elderly patients on fixed incomes.
Elderly MS patients have specific physical and
psychosocial challenges. Physical challenges include impaired mobility,
spas-ticity, pain and bladder dysfunction, impaired sleep, and an in-creased
need for assistance with self-care (Klewer et al., 2001). Psychosocial issues
include depression and suicidal thoughts (Klewer et al., 2001).
Medical Management
No cure exists for MS.
An individualized, organized, and ratio-nal treatment program is indicated to
relieve the patient’s symp-toms and provide continuing support, particularly
for individuals with cognitive changes (50%), who may need more structure and
support. The goals of treatment are to delay the progression of the disease,
manage chronic symptoms, and treat acute exacer-bations. Many patients with MS
have stable disease and require only intermittent treatment, whereas others
experience steady progression of their disease. Symptoms requiring intervention
include spasticity, fatigue, bladder dysfunction, and ataxia. Management
strategies target the various motor and sensory symptoms and effects of
immobility that can occur.
PHARMACOLOGIC THERAPY
Three medications, referred to as the “ABC (and R)
drugs,” are currently the main pharmacologic therapy for MS. The inter-ferons
beta-1a (Avonex) and beta-1b (Betaseron) reduce the fre-quency of relapse by
30% and decrease the appearance of new lesions on MRI by 80% (Tselis &
Lisak, 1999). Glatiramer ac-etate (Copaxone) also reduces the number of lesions
on MRI and the relapse rate. In March 2002, the FDA approved a fourth agent,
Rebif, for the treatment of relapsing MS (PRISMS Study Group, 2001).
All of these medications have multiple immune activities.
The interferons reduce T-cell proliferation; glatiramer acetate inhibits
antigen-specific T-cell activation (Noseworthy et al., 2000). All of the
disease-modifying medications, the “ABC (and R) drugs,” require injections.
Interferon beta-1b (Betaseron) is administered subcutaneously every other day,
interferon beta-la (Avonex) is given by intramuscular injection once a week,
and glatiramer ac-etate (Copaxone) is administered by subcutaneous injection
every day. Rebif is administered subcutaneously three times a week.
Seventy-five percent of patients taking one of the interferons ex-perience
flu-like symptoms; these symptoms can be controlled with nonsteroidal
anti-inflammatory drugs (NSAIDs) and usu-ally resolve after a few months of
therapy (Walther & Hohlfeld, 1999). Patients receiving these injectable
medications and their families must be instructed in injection technique and
must be-come knowledgeable about site reactions and other possible side effects
(Ross, 2001).
Mitoxantrone (Novantrone),
which received FDA approval in 2000 (Rolak, 2001), is an antineoplastic agent
used primarily to treat leukemia and lymphoma. It received approval to treat
sec-ondary progressive MS due to its immunosuppressive qualities (Rolak, 2001).
Patients need to have laboratory tests (complete blood count) performed, and
the results must be closely monitored due to the potential for leukopenia and
cardiac toxicity. A few pa-tients (2% to 3%) will develop signs and symptoms of
cardio-myopathy and heart failure due to cardiac toxicity (Rolak, 2001).
Corticosteroids modulate
the immune response and are used to limit the severity and duration of
exacerbations. These agents suppress the immune response and decrease
inflammatory change. Nerve conduction is restored with variable degrees of
sympto-matic recovery. Typically the patient receives high-dose IV
methyl-prednisolone followed by an oral prednisone taper. The nurse must
carefully monitor the patient for side effects related to cor-ticosteroids such
as mood changes and fluid and electrolyte alter-ations and teach the patient
and family about side effects.
Researchers continue to
investigate other possible treatments for MS. Many agents that have been
investigated have proven to be too toxic for clinical use. Researchers are
studying strategies that facilitate the proliferation of anti-inflammatory
cytokines. T-cell vaccination and agents that inhibit oxygen radicals and
proteases are under study (Noseworthy et al., 2000).
Medications are also
prescribed for management of specific symptoms. Baclofen (Lioresal), a GABA
agonist, is the medica-tion of choice in treating spasms. It can be
administered orally or by intrathecal injection. Benzodiazepines (Valium),
tizanidine (Zanaflex), and dantrolene (Dantrium) may also be used to treat
spasms. Patients with disabling spasms and contractures may require nerve
blocks or surgical intervention. Fatigue that interferes with activities of
daily living may be treated with amantadine (Symmetrel), pemoline (Cylert), or
fluoxetine (Prozac). Ataxia is a chronic problem most resistant to treatment.
Medications used to treat ataxia include beta-adrenergic blockers (Inderal),
anti-seizure agents (Neurontin), and benzodiazepines (Klonopin).
Various strategies for
pain management can be implemented, based on the type of pain that exists.
Acute pain may be treated with antidepressants, opiates, or antiseizure
medications. Surgi-cal procedures may be required to interrupt the pain
pathway. Subacute pain as well as chronic back pain can be effectively treated
with NSAIDs. Physical therapy may also benefit the patient by improving posture
and strength.
Pain may also be due to
osteoporosis (Maloni, 2000). Peri-menopausal women with MS are more likely to
develop osteo-porosis than those without MS. Immobility, corticosteroid
therapy, and estrogen loss play a role in the development of osteoporosis in
women with MS. Bone mineral density testing is recommended for this high-risk
group (Smeltzer, Zimmerman, Capriotti & Fernandes, 2002).
Management of bladder
and bowel control is often among the patient’s most difficult problems and a
variety of medications (anticholinergics, alpha-adrenergic blockers, or
antispasmodic agents) may be prescribed. Nonpharmacologic strategies also
as-sist in establishing effective bowel and bladder elimination (see Nursing
Process section).
Urinary tract infection is often superimposed on the
under-lying neurologic dysfunction. Ascorbic acid (vitamin C) may be prescribed
to acidify the urine, making bacterial growth less likely. Antibiotics are
prescribed when appropriate.
Related Topics