Chapter: Medical Surgical Nursing: Management of Patients With Neurologic Trauma
Nursing Process: The Patient With Quadriplegia or Paraplegia
NURSING PROCESS: THE PATIENT WITH
QUADRIPLEGIA OR PARAPLEGIA
Assessment
Assessment focuses on
the patient’s general condition, complica-tions, and how the patient is
managing at that particular point in time. A head-to-toe assessment and review
of systems should be part of the database, with emphasis on the areas prone to
prob-lems in this population. A thorough inspection of all areas of the skin
for redness or breakdown is critical. It is also important to review with the
patient the established bowel and bladder pro-gram, because the program must
continue uninterrupted. Patients with quadriplegia or paraplegia have varying
degrees of loss of motor power, deep and superficial sensation, vasomotor control,
bladder and bowel control, and sexual function. They are faced with potential
complications related to immobility, skin break-down and pressure ulcers,
recurring UTI, contractures, and psychosocial disruptions. Knowledge about
these particular issues can further guide the assessment in any setting. Nurses
in all settings, including home care, must be aware of these potential
complications in the lifetime management of these patients.
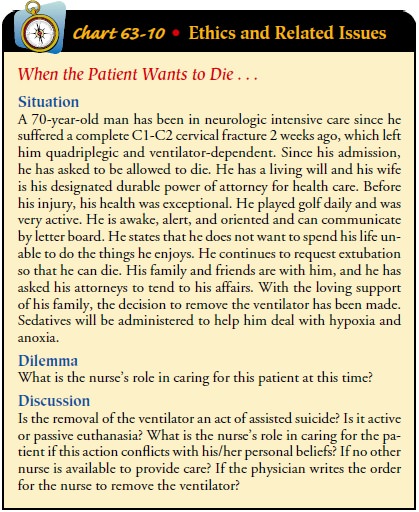
An understanding of the
emotional and psychological responses to quadriplegia or paraplegia is achieved
by observing the responses and behaviors of the patient and family and by
listening to their concerns (see Chart 63-10 for a discussion of ethical
issues). Documenting these assessments and reviewing the plan with the entire
team on a regular basis provide insight into how both the pa-tient and the
family are coping with the changes in lifestyle and body functioning.
Additional information frequently can be gath-ered from the social worker or
psychiatric/mental health worker.
It takes time for the patient and family to comprehend
the magnitude of the disability. They may go through stages of grief, including
shock, disbelief, denial, anger, depression, and accep-tance. During the acute
phase of the injury, denial can be a pro-tective mechanism to shield patients
from the overwhelming reality of what has happened. As they realize the
permanent na-ture of paraplegia or quadriplegia, the grieving process may be
prolonged and all-encompassing because of the recognition that long-held plans
and expectations may be interrupted or perma-nently altered. A period of
depression often follows as the patient experiences a loss of self-esteem in
areas of self-identity, sexual functioning, and social and emotional roles.
Exploration and as-sessment of these issues can assist in developing a
meaningful plan of care.
Diagnosis
NURSING DIAGNOSES
Based on the assessment data, the major nursing diagnoses
of the patient with quadriplegia or paraplegia may include the following:
·
Impaired physical mobility
related to loss of motor function
·
Risk for disuse syndrome
·
Risk for impaired skin
integrity related to permanent sen-sory loss and immobility
·
Urinary retention related to
level of injury
·
Constipation related to effects
of spinal cord disruption
·
Sexual dysfunction related to
neurologic dysfunction
·
Ineffective coping related to
impact of dysfunction on daily living
·
Deficient knowledge about
requirements for long-term management
COLLABORATIVE PROBLEMS/POTENTIAL COMPLICATIONS
Based on all the assessment data, potential complications
of quad-riplegia or paraplegia that may develop include:
·
Spasticity
·
Infection and sepsis
Planning and Goals
The goals for the patient may include attainment of some
form of mobility, maintenance of healthy, intact skin, achievement of bladder
management without infection, achievement of bowel control, achievement of
sexual expression, strengthening of coping mechanisms, and absence of
complications.
Nursing Interventions
The patient requires extensive rehabilitation, which is
less dif-ficult if appropriate nursing management has been carried out during
the acute phase of the injury or illness. Nursing care is one of the key
factors determining the success of the rehabilitation program. The main
objective is for the patient to live as inde-pendently as possible in the home
and community.
INCREASING MOBILITY
Exercise Programs
The unaffected parts of
the body are built up to optimal strength to promote maximal self-care. The
muscles of the hands, arms,shoulders, chest, spine, abdomen, and neck must be
strengthened in the paraplegic patient because he or she must bear full weight
on these muscles to ambulate. The triceps and the latissimus dorsi are
important muscles used in crutch walking. The muscles of the abdomen and the
back also are necessary for balance and for maintaining the upright position.
To strengthen these
muscles, the patient can do push-ups when in a prone position and sit-ups when
in a sitting position. Extending the arms while holding weights (traction
weights can be used) also develops muscle strength. Squeezing rubber balls or
crumbling newspaper promotes hand strength.
With encouragement from
all members of the rehabilitation team, the paraplegic patient can develop the
increased exercise tolerance needed for gait training and ambulation
activities. The importance of maintaining cardiovascular fitness is stressed to
the patient. Alternative exercises to increase the heart rate to target levels
must be designed within the patient’s abilities.
Mobilization
When the spine is stable
enough to allow the patient to assume an upright posture, mobilization
activities are initiated. A brace or vest may be used, depending on the level
of the lesion. A pa-tient whose paralysis is due to complete transection of the
cord can begin weight-bearing early because no further damage can be incurred.
The sooner muscles are used, the less chance there is of disuse atrophy. The
earlier the patient is brought to a stand-ing position, the less opportunity
for osteoporotic changes to take place in the long bones. Weight-bearing also
reduces the possibility of renal calculi and enhances many other metabolic
processes.
Braces and crutches enable some paraplegic patients to
ambu-late for short distances. Ambulation using crutches requires a high
expenditure of energy. Motorized wheelchairs and specially equipped vans can
provide greater independence and mobility for patients with high-level SCI or
other lesions. Every effort should be made to encourage the patient to be as
mobile and active as possible.
PREVENTING DISUSE SYNDROME
Patients are at high risk for developing contractures as
a result of disuse syndrome due to the musculoskeletal system changes (atrophy)
brought about by the loss of motor and sensory functions below the level of
injury. Range-of-motion exercises must be pro-vided at least four times a day,
and care is taken to stretch the Achilles tendon with exercises (Hickey, 2003).
The patient is repositioned frequently and maintained in proper body align-ment
whether in bed or in a wheelchair (Hickey, 2003).
PROMOTING SKIN INTEGRITY
Because these patients
spend a great portion of their lives in wheel-chairs, pressure ulcers are an
ever-present threat. Contributing factors are permanent sensory loss over
pressure areas; immobil-ity, which makes relief of pressure difficult; trauma
from bumps (against the wheelchair, toilet, furniture, and so forth) that cause
unperceived abrasions and wounds; loss of protective function of the skin from
excoriation and maceration due to excessive per-spiration and possible urinary
and fecal incontinence; and poor general health (anemia, edema, malnutrition),
leading to poor tis-sue perfusion.
The person with
quadriplegia or paraplegia must take respon-sibility for monitoring (or
directing) his or her skin status. This involves relieving pressure and not
remaining in any position for longer than 2 hours, in addition to ensuring that
the skin receives meticulous attention and cleansing. The patient is taught
that ul-cers develop over bony prominences exposed to unrelieved pres-sure in
the lying and sitting positions. The most vulnerable areas are identified. The
paraplegic patient is instructed to use mirrors, if possible, to inspect these
areas morning and night, observing for redness, slight edema, or any abrasions.
While in bed, the patient should turn at 2-hour intervals and then inspect the
skin again for redness that does not fade on pressure. The bottom sheet should
be checked for wetness and for creases. The quadriplegic or paraplegic patient
who cannot perform these activities is en-couraged to direct others to check
these areas and prevent ulcers from developing.
The patient is taught to
relieve pressure while in the wheelchair by doing push-ups, leaning from side
to side to relieve ischial pres-sure, and tilting forward while leaning on a
table. The caregiver for the quadriplegic patient will need to perform these
activities if the patient cannot do so independently. A wheelchair cushion is
prescribed to meet individual needs, which may change in time with changes in
posture, weight, and skin tolerance. A referral can be made to a rehabilitation
engineer, who can measure pressure levels while the patient is sitting and then
tailor the cushion and other necessary aids and assistive devices to the
patient’s needs.
The diet for the patient
with quadriplegia or paraplegia should be high in protein, vitamins, and
calories to ensure minimal wast-ing of muscle and the maintenance of healthy
skin, and high in fluids to maintain well-functioning kidneys. Excessive weight
gain and obesity should be avoided because they limit mobility.
IMPROVING BLADDER MANAGEMENT
The effect of the spinal cord lesion on the bladder
depends on the level of injury, the degree of cord damage, and the length of
time after injury. A patient with quadriplegia or paraplegia usually has either
a reflex or a nonreflex bladder (see Chaps. 11 and 44). Both bladder types
increase the risk of UTI.
The nurse emphasizes the importance of maintaining an
ade-quate flow of urine by encouraging a fluid intake of about 2.5 L daily. The
patient should empty the bladder frequently so there is minimal residual urine
and should pay attention to personal hygiene, because infection of the bladder
and kidneys almost always occurs by the ascending route. The perineum must be
kept clean and dry and attention given to the perianal skin after defe-cation.
Underwear should be cotton (more absorbent) and changed at least once a day.
If an external catheter (condom catheter) is used, the
sheath is removed nightly; the penis is cleansed to remove urine and is dried
carefully, because warm urine on the periurethral skin pro-motes the growth of
bacteria. Attention also is given to the col-lection bag. The nurse emphasizes
the importance of monitoring for indications of UTI: cloudy, foul-smelling
urine or hematuria (blood in the urine), fever, or chills.
The female patient who cannot achieve reflex bladder
control or self-catheterization may need to wear pads or waterproof
undergarments. Surgical intervention may be indicated in some patients to
create a urinary diversion.
ESTABLISHING BOWEL CONTROL
The objective of a bowel training program is to establish
bowel evacuation through reflex conditioning. If a cord injury occurs above the
sacral seg-ments or nerve roots and there is reflex activity, the anal
sphincter may be massaged (digital stimulation) to stimulate defecation. If the
cord lesion involves the sacral segment or nerve roots, anal massage is not
performed because the anus may be relaxed and lack tone. Massage is also
contraindicated if there is spasticity of the anal sphincter. The anal
sphincter is massaged by inserting a gloved finger (which has been adequately
lubricated) 2.5 to 3.7 cm (1 to 1.5 in) into the rectum and moving it in a
circular motion or from side to side. It soon becomes apparent which area
triggers the defecation response. This procedure should be performed at the
same time (usually every 48 hours), after a meal, and at a time that will be
convenient for the patient at home. The patient also is taught the symptoms of
impaction (frequent loose stools; constipation) and cautioned to watch for
hemorrhoids. A diet with sufficient fluids and fiber is essential to a
successful bowel training program, avoiding constipation, and decreasing the
risk of autonomic dysreflexia.
COUNSELING ON SEXUAL EXPRESSION
Many paraplegic and
quadriplegic patients can have some form of meaningful sexual relationship,
although some modifications will be necessary. The patient and partner benefit
from counsel-ing about the range of sexual expression possible, special
techniques and positions, exploration of body sensations offering sensual
feelings, and urinary and bowel hygiene as related to sexual ac-tivity. For men
with erectile failure, penile prostheses enable them to have and sustain an
erection. Sildenafil (Viagra) is an oral smooth muscle relaxant that causes
blood to flow into the penis, resulting in an erection.
Sexual education and counseling services are included in
the rehabilitation services at spinal centers. Small-group meetings in which
the patients can share their feelings, receive information, and discuss sexual
concerns and practical aspects are helpful in producing effective attitudes and
adjustments (Sipski & Alexander, 1997).
ENHANCING COPING MECHANISMS
The impact of the
disability and loss becomes marked when pa-tients return home. Each time
something new enters their lives (eg, a new relationship, going to work), they
are reminded anew of their limitations. Grief reactions and depression are
common.
To work through this depression, patients must have some
hope for relief in the future. Thus, the nurse can encourage them to feel
confident in their ability to achieve self-care and relative independence. The
role of the nurse ranges from caretaker during the acute phase to teacher,
counselor, and facilitator as patients gain mobility and independence.
The patient’s disability affects not only the patient,
but also the entire family. In many cases, family therapy is helpful to help
work through issues as they arise.
Adjustment to the
disability leads to the development of re-alistic goals for the future, making
the best of the abilities that are left intact and reinvesting in other
activities and relation-ships. Rejection of the disability causes
self-destructive neglect and noncompliance with the therapeutic program, which
leads to more frustration and depression. Crises for which interven-tions may
be sought include social, psychological, marital, sexual, and psychiatric
problems. The family usually requires counsel-ing, social services, and other
support systems to help them cope with the changes in their lifestyle and
socioeconomic status.
A major goal of nursing
management is to help patients over-come their sense of futility and to
encourage them in the emo-tional adjustment that must be made before they are
willing to venture into the outside world. However, an excessively sympa-thetic
attitude on the part of the nurse may cause patients to develop an
overdependence that defeats the purpose of the entire rehabilitation program.
Patients are taught and assisted when necessary, but the nurse should avoid
performing activities that patients can do for themselves with a little effort.
This approach to care more than repays itself in the satisfaction of seeing a
com-pletely demoralized and helpless patient become independent and find
meaning in a newly emerging lifestyle.
MONITORING AND MANAGING POTENTIAL COMPLICATIONS
Spasticity
Muscle spasticity is one of the most problematic
complications of quadriplegia and paraplegia. These incapacitating flexor or
ex-tensor spasms, which occur below the level of the spinal cord le-sion,
interfere with both the rehabilitation process and activities of daily living.
Spasticity results from an imbalance between the facilitatory and inhibitory
effects on neurons that exist normally. The area of the cord distal to the site
of injury or lesion becomes disconnected from the higher inhibitory centers
located in the brain. Facilitatory impulses, which originate from muscles,
skin, and ligaments, thus predominate.
Spasticity is defined as a condition of increased muscle
tone in a muscle that is weak. Initial resistance to stretching is quickly
followed by sudden relaxation. The stimulus that precipitates spasm can be
either obvious, such as movement or a position change, or subtle, such as a
slight jarring of the wheelchair. Most patients with quadriplegia or paraplegia
have some degree of spasticity. With SCI, the onset of spasticity usually
occurs from a few weeks to 6 months after the injury. The same muscles that are
flaccid during the period of spinal shock will develop spas-ticity during
recovery. The intensity of spasticity tends to peak around 2 years after the
injury, after which the spasms tend to regress.
Management of spasticity
is based on the severity of symptoms and the degree of incapacitation.
Antispasmodic medications such as diazepam (Valium), baclofen (Lioresal), and
dantrolene (Dantrium) are frequently effective in controlling spasm but cause
drowsiness, weakness, and vertigo in some patients. Passive range-of-motion
exercises and frequent turning and reposition-ing are helpful because stiffness
tends to increase spasticity. These activities also are essential in the
prevention of contractures, pres-sure ulcers, and bowel and bladder
dysfunction.
Contractures can complicate day-to-day care, increasing
the difficulty with positioning and decreasing mobility. A number of surgical
procedures have been tried with varying degrees of suc-cess. These techniques
are used if more conservative approaches fail. The best treatment is
prevention.
Infection and Sepsis
Patients with
quadriplegia and paraplegia are at increased risk for infection and sepsis from
a variety of sources: urinary tract, res-piratory tract, and pressure ulcers.
Sepsis remains a major cause of death and complications in these patients.
Prevention of in-fection and sepsis is essential through maintenance of skin
in-tegrity, complete emptying of the bladder at regular intervals, and
prevention of urinary and fecal incontinence. The risk of respira-tory
infection can be decreased by avoiding contact with people with symptoms of
respiratory infection, performing coughing and deep-breathing exercises to
prevent pooling of respiratory se-cretions, receiving yearly influenza
vaccines, and giving up smok-ing. A high-protein diet is important in
maintaining an adequate immune system, as is avoiding factors that may reduce
immunesystem function (eg, excessive stress, drug abuse,
excessive alcohol intake).
If infection occurs, the patient requires thorough
assessment and prompt treatment. Antibiotic therapy and adequate hydra-tion, in
addition to local measures (depending on the site of infection), are initiated
immediately.
UTIs are minimized or prevented by:
·
Aseptic technique in catheter
management
·
Adequate hydration
·
Bladder training program
·
Prevention of overdistention
of the bladder and stasis
Skin breakdown and infection are prevented by:
·
Maintenance of a turning
schedule
·
Frequent back care
·
Regular assessment of all skin
areas
·
Regular cleansing and
lubrication of the skin
·
Passive range-of-motion
exercise to prevent contractures
·
Pressure relief, particularly
over broken skin areas, bony prominences, and heels
·
Wrinkle-free bed linen
Pulmonary infections are managed and prevented by:
·
Frequent coughing, turning,
and deep-breathing exercises and chest physiotherapy
·
Aggressive respiratory care
and suctioning of the airway if a tracheostomy is present
·
Assisted coughing
·
Adequate hydration
Infections of any kind can be life-threatening.
Therefore, ag-gressive nursing interventions are key to their prevention and
management.
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care
Patients with
quadriplegia or paraplegia are at risk for complica-tions for the rest of their
lives. Thus, a major aspect of nursing care is teaching patients and their
families about these complica-tions and about strategies to minimize this risk.
UTIs, contractures, infected pressure ulcers, and sepsis may necessitate
hospitaliza-tion. Other late complications that may occur include lower
ex-tremity edema, joint contractures, respiratory dysfunction, and pain. To
avoid these and other complications, the patient and a family member are taught
skin care, catheter care, range-of-motion exercises, breathing exercises, and
other care techniques. Teaching is initiated as soon as possible and extends
into the rehabilitation or long-term care facility and home.
Continuing Care
Referral for home care is often appropriate for
assessment of the home setting, patient teaching, and evaluation of the
patient’s physical and emotional status. During visits by the home care nurse,
teaching about strategies to prevent or minimize potential complications is
reinforced. The home environment is assessed for adequacy for care and for
safety. Environmental modifications are made and specialized equipment is
obtained, ideally before the patient goes home.
The home care nurse also
assesses the patient’s and the family’s adherence to recommendations and their
use of coping strategies. The use of inappropriate coping strategies such as
drug and alco-hol use is assessed and referrals to counseling are made for the
patient and family. Appropriate and effective coping strategies are reinforced.
The nurse reviews previous teaching and deter-mines the need for further
physical or psychological assistance. The patient’s self-esteem and body image
may be very poor at this time. Because people with high levels of social
support often re-port feelings of well-being despite major physical disability,
it is beneficial for the nurse to assess and promote further develop-ment of
the support system and effective coping strategies of each patient.
The patient requires continuing, life-long follow-up by
the physician, physical therapist, and other rehabilitation team mem-bers
because the neurologic deficit is usually permanent and new deficits and
complications can develop. These require prompt at-tention before they take
their toll in additional physical impair-ment, time, morale, and financial
costs. The local counselor for the Office of Vocational Rehabilitation works
with the patient with respect to job placement or additional educational or voca-tional
training.
The nurse is in a good position to remind patients and
family members of the need for continuing health promotion and screening
practices. Referral to accessible health care providers and imaging centers is
important in health promotion.
Evaluation
EXPECTED PATIENT OUTCOMES
Expected patient outcomes may include:
a) Attains
some form of mobility
b) Contractures
do not develop
c) Maintains
healthy, intact skin
d) Achieves
bladder control, absence of UTI
e) Achieves
bowel control
f) Reports sexual satisfaction
g)Shows
improved adaptation to environment and others
h) Exhibits
reduction in spasticity
i) Reports
understanding of the precipitating factors
ii) Reports
understanding of measures to reduce spasticity
i) Describes
long-term management required
j) Exhibits
absence of complications
Related Topics