Chapter: Medical Surgical Nursing: Management of Patients With Neurologic Trauma
Brain Injury
Brain
Injury
The most important consideration in any head injury is
whether or not the brain is injured. Even seemingly minor injury can cause
significant brain damage secondary to obstructed blood flow and decreased
tissue perfusion. The brain cannot store oxygen and glucose to any significant
degree. Because the cerebral cells need an uninterrupted blood supply to obtain
these nutrients, irre-versible brain damage and cell death occur when the blood
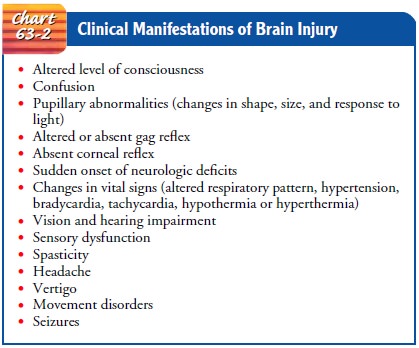
sup-ply is interrupted for even a few minutes. Clinical manifestations of brain injury are listed in Chart 63-2. Closed (blunt) braininjury occurs when
the head accelerates and then rapidly decel-erates or collides with another
object (eg, a wall or dashboard of a car) and brain tissue is damaged, but
there is no opening through the skull and dura. Open brain injury occurs when an object penetrates the skull,
enters the brain, and damages the soft brain tissue in its path (penetrating
injury), or when blunt trauma to the head is so severe that it opens the scalp,
skull, and dura to expose the brain.
Concussion
A cerebral concussion after head injury is a temporary loss of neurologic function with no apparent structural damage. A con-cussion generally involves a period of unconsciousness lasting from a few seconds to a few minutes.
The jarring of the
brain may be so slight as to cause only dizziness and spots before the eyes
(“seeing stars”), or it may be severe enough to cause complete loss of
consciousness for a time. If the brain tissue in the frontal lobe is affected,
the patient may exhibit bizarre irrational behavior, whereas involvement of the
temporal lobe can produce temporary amnesia or disorientation.
The patient may be
hospitalized overnight for observation or discharged from the hospital in a
relatively short time after a con-cussion. Treatment involves observing the
patient for headache, dizziness, lethargy, irritability, and anxiety. The
occurrence of these symptoms after injury is referred to as postconcussion
syndrome. Giving the patient information, explanations, and encouragement may
reduce some of the problems of postconcussion syndrome. The patient is advised
to resume normal activities slowly, and the family is instructed to observe for
the following signs and symp-toms and to notify the physician or clinic (or
bring the patient to the emergency department) if they occur:
·
Difficulty in awakening
·
Difficulty in speaking
·
Confusion
·
Severe headache
·
Vomiting
·
Weakness of one side of the
body
A concussion was once thought of as a minor head injury
without significant sequelae. However, studies have demonstrated that there are
often disturbing and sometimes residual effects, in-cluding headache, lethargy,
personality and behavior changes, attention deficits, difficulty with memory,
and disruption in work habits (Ponsford et al., 1999).
Gerontologic Considerations
Elderly patients must be
assessed very carefully. Even given similar mechanisms of injury, an elderly
person will often suffer more severe injury than a young person and will often
recover more slowly and with more complications (Perdue et al., 1998). The
elderly patient with confusion or behavioral disturbances should be assessed
for head injury, because unrecognized “minor” head trauma may account for
behavioral and confusional episodes in some elderly people (Walshaw, 2000). A
misdiagnosed or un-treated episode of confusion in an elderly patient may
result in long-term disability that might have been avoided if the injury had
been detected and treated promptly.
Contusion
Cerebral contusion is a more severe injury in
which the brain is bruised, with possible surface hemorrhage. The patient is
un-conscious for more than a few seconds or minutes. Clinical signs and
symptoms depend on the size of the contusion and the amount of associated
cerebral edema. The patient may lie motionless, with a faint pulse, shallow
respirations, and cool, pale skin. Often there is involuntary evacuation of the
bowels and the bladder. The patient may be aroused with effort but soon slips
back into unconsciousness. The blood pressure and the temperature are
subnormal, and the picture is somewhat similar to that of shock.
In general, patients with severe brain injury who have
abnor-mal motor function, abnormal eye movements, and elevated ICP have poor
outcomes—that is, brain damage, disability, or death. Conversely, the patient
may recover consciousness but pass into a stage of cerebral irritability. In
this stage, the patient is conscious and easily disturbed by any form of
stimulation such as noises, light, and voices; he or she may become hyperactive
at times. Gradually, the pulse, respirations, temperature, and other body
functions return to normal, but full recovery can be delayed for months.
Residual headache and vertigo are common, and im-paired mental function or
seizures may occur as a result of irreparable cerebral damage.
Diffuse Axonal Injury
Diffuse axonal injury involves widespread damage to axons
in the cerebral hemispheres, corpus callosum, and brain stem. It can be seen in
mild, moderate, or severe head trauma and results in axonal swelling and
disconnection (Porth, 2002). Clinically, with severe injury, the patient has no
lucid intervals and experiences imme-diate coma, decorticate and decerebrate
posturing, and global cerebral edema. Diagnosis is made by clinical signs in
conjunction with a CT scan or MRI. Recovery depends on the severity of the
axonal injury.
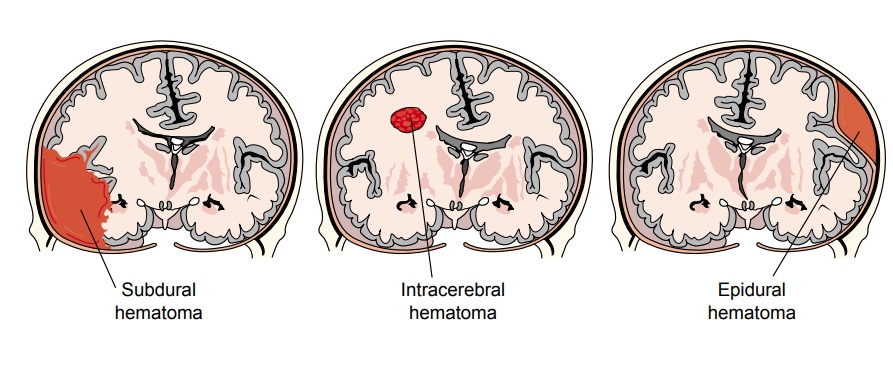
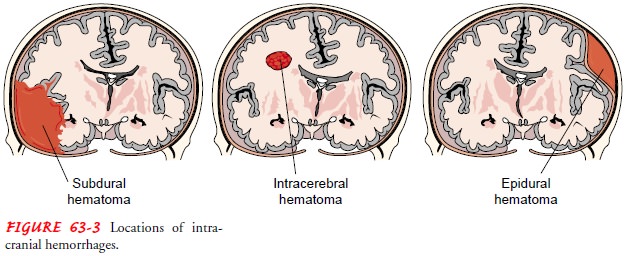
Intracranial Hemorrhage
Hematomas (collections
of blood) that develop within the cra-nial vault are the most serious brain
injuries (Porth, 2002). A hematoma may be epidural (above the dura), subdural
(below the dura), or intracerebral (within the brain) (Fig. 63-3). Major
symptoms are frequently delayed until the hematoma is large enough to cause
distortion of the brain and increased ICP. The signs and symptoms of cerebral
ischemia resulting from the compression by a hematoma are variable and depend
on the speed with which vital areas are affected and the area that is injured.
In general, a rapidly developing hematoma, even if small, may be fatal, whereas
a larger but slowly developing collection of blood may allow compensation for
increases in ICP.
EPIDURAL HEMATOMA (EXTRADURAL HEMATOMA OR HEMORRHAGE)
After a head injury, blood may collect in the epidural
(extradural) space between the skull and the dura. This can result from a skull
fracture that causes a rupture or laceration of the middle meningeal artery,
the artery that runs between the dura and the skull infe-rior to a thin portion
of temporal bone. Hemorrhage from this artery causes rapid pressure on the
brain.
Symptoms are caused by the expanding hematoma. Usually,
there is a momentary loss of consciousness at the time of injury, followed by an
interval of apparent recovery (lucid interval). Although the lucid interval is
considered a classic characteristic of an epidural hematoma, no lucid interval
has been reported in many patients with this lesion (Servadei, 1997), and thus
it should not be considered a critical defining criterion. During the lucid
interval, compensation for the expanding hematoma takes place by rapid
absorption of CSF and decreased intravascular volume, both of which help
maintain a normal ICP. When these mecha-nisms can no longer compensate, even a
small increase in the volume of the blood clot produces a marked elevation in
ICP. Then, often suddenly, signs of compression appear (usually dete-rioration
of consciousness and signs of focal neurologic deficits such as dilation and
fixation of a pupil or paralysis of an extremity), and the patient deteriorates
rapidly.
An epidural hematoma is considered an extreme emergency;
marked neurologic deficit or even respiratory arrest can occur within minutes.
Treatment consists of making openings through the skull (burr holes) to
decrease ICP emergently, remove the clot, and control the bleeding. A
craniotomy may be required to remove the clot and control the bleeding. A drain
is usually in-serted after creation of burr holes or a craniotomy to prevent
reaccumulation of blood.
SUBDURAL HEMATOMA
A subdural hematoma is a collection of blood between the dura and the brain, a space normally occupied by a thin cushion of fluid. The most common cause of subdural hematoma is trauma, but it may also occur from coagulopathies or rupture of an aneurysm. A subdural hemorrhage is more frequently venous in origin and is due to the rupture of small vessels that bridge the subdural space. A subdural hematoma may be acute, subacute, or chronic, depending on the size of the involved vessel and the amount of bleeding present.
Acute and Subacute Subdural Hematoma.
Acute subdural
hema-tomas are associated with major head injury involving contusion or
laceration. Clinical symptoms develop over 24 to 48 hours. Signs and symptoms
include changes in the level of consciousness (LOC), pupillary signs, and
hemiparesis. There may be minor or even no symptoms with small collections of
blood. Coma, in-creasing blood pressure, decreasing heart rate, and slowing
respi-ratory rate are all signs of a rapidly expanding mass requiring immediate
intervention.
Subacute subdural hematomas are the result of less severe
con-tusions and head trauma. Clinical manifestations usually appear between 48
hours and 2 weeks after the injury. Signs and symp-toms are similar to those of
an acute subdural hematoma.
If the patient can be transported rapidly to the
hospital, an immediate craniotomy is performed to open the dura, allowing the
subdural clot to be evacuated. Successful outcome also de-pends on the control
of ICP and careful monitoring of respira-tory function. The mortality rate for
patients with acute and sub-acute subdural hematomas is high because of
associated brain damage.
Chronic Subdural Hematoma.
Chronic subdural
hematomas candevelop from seemingly minor head injuries and are seen most
frequently in the elderly. The elderly are prone to this type of head injury
secondary to brain atrophy, which is an expected con-sequence of the aging process.
Seemingly minor head trauma may produce enough impact to shift the brain
contents abnormally. The time between injury and onset of symptoms may be
lengthy (eg, 3 weeks to months), so the actual insult may be forgotten.
A chronic subdural hematoma resembles other conditions
and may be mistaken for a stroke. The bleeding is less profuse and there is
compression of the intracranial contents. The blood within the brain changes in
character in 2 to 4 days, becoming thicker and darker. In a few weeks, the clot
breaks down and has the color and consistency of motor oil. Eventually,
calcification or ossification of the clot takes place. The brain adapts to this
for-eign body invasion, and the clinical signs and symptoms fluctu-ate. There
may be severe headache, which tends to come and go; alternating focal
neurologic signs; personality changes; mental de-terioration; and focal
seizures. Unfortunately, the patient may be labeled neurotic or psychotic if
the cause of the symptoms is over-looked.
The treatment of a chronic subdural hematoma consists of
surgical evacuation of the clot. The procedure may be carried out through
multiple burr holes, or a craniotomy may be performed for a sizable subdural
mass that cannot be suctioned or drained through burr holes.
INTRACEREBRAL HEMORRHAGE AND HEMATOMA
Intracerebral
hemorrhage is bleeding into the substance of the brain. It is commonly seen in
head injuries when force is exerted to the head over a small area (missile
injuries or bullet wounds; stab injury). These hemorrhages within the brain may
also result from systemic hypertension, which causes degeneration and rup-ture
of a vessel; rupture of a saccular aneurysm; vascular anom-alies; intracranial
tumors; systemic causes, including bleeding disorders such as leukemia,
hemophilia, aplastic anemia, and thrombocytopenia; and complications of
anticoagulant therapy.
The onset may be
insidious, beginning with the development of neurologic deficits followed by
headache. Management includes supportive care, control of ICP, and careful
administration of fluids, electrolytes, and antihypertensive medications.
Surgical intervention by craniotomy or craniectomy permits removal of the blood
clot and control of hemorrhage but may not be possi-ble because of the
inaccessible location of the bleeding or the lack of a clearly circumscribed
area of blood that can be removed.
Management of Brain Injuries
Assessment and diagnosis
of the extent of injury are accomplished by the initial physical and neurologic
examinations. CT and MRI are the primary neuroimaging diagnostic tools and are
useful in evaluating soft tissue injuries. Positron emission tomography (PET
scan) is available in some trauma centers; this method of scanning examines
brain function rather than structure. A flow-chart developed by the Brain
Trauma Foundation for the initial management of brain-injured patients is
presented in Figure 63-4 (Brain Trauma Foundation, 2000).
Any individual with a
head injury is presumed to have a cer-vical spine injury until proven
otherwise. From the scene of the injury, the patient is transported on a board
with the head and neck maintained in alignment with the axis of the body. A
cervi-cal collar should be applied and maintained until cervical spine x-rays
have been obtained and the absence of cervical spinal cord injury documented.
All therapy is directed toward preserving brain
homeostasis and preventing secondary brain injury. “Secondary injury” is a term
used to describe injury to the brain subsequent to the orig-inal traumatic
event (Bader & Palmer, 2000). Common causes of secondary injury are
cerebral edema, hypotension, and respi-ratory depression that may lead to
hypoxemia and electrolyte imbalance. Treatments to prevent this include
stabilization of cardiovascular and respiratory function to maintain adequate
cerebral perfusion, control of hemorrhage and hypovolemia, and maintenance of
optimal blood gas values (Wong, 2000).
TREATMENT OF INCREASED INTRACRANIAL PRESSURE
As the damaged brain swells with edema or as blood
collects within the brain, a rise in ICP occurs; this requires aggressive
treatment. If the ICP remains elevated, it can decrease the CPP. Initial
management is based on the principle of preventing secondary injury and
maintaining adequate cere-bral oxygenation (see Fig. 63-4).
Surgery is required for
evacuation of blood clots, débridement and elevation of depressed fractures of
the skull, and suture of se-vere scalp lacerations. ICP is monitored closely;
if increased, it is managed by maintaining adequate oxygenation, elevating the
head of the bed, and maintaining normal blood volume. Devices to monitor ICP or
drain CSF can be inserted during surgery or at the bedside using aseptic
technique. The patient is cared for in the intensive care unit, where expert
nursing care and medical treatment are readily available.
SUPPORTIVE MEASURES
Treatment also includes ventilatory support, seizure
prevention, fluid and electrolyte maintenance, nutritional support, and pain
and anxiety management. Comatose patients are intubated and mechanically
ventilated to ensure adequate oxygenation and pro-tect the airway.
Because seizures are common after head injury and can cause secondary brain damage from hypoxia, antiseizure agents may be administered. If the patient is very agitated, benzodiazepines may be prescribed to calm him or her without decreasing LOC. These medications do not affect ICP or CPP, making them good choices for the head-injured patient.
A nasogastric tube may
be inserted because reduced gastric motility and reverse peristalsis are
associated with head injury, making regurgitation and aspiration common in the
first few hours.
BRAIN DEATH
When a patient has sustained a severe head injury
incompatible with life, the nurse may assist in the clinical examination for
determination of brain death and in the process of organ pro-curement. Since
1981, all 50 states have recognized the Uni-form Determination of Brain Death
Act (Lovasik, 2000). This act states that death will be determined with accepted
medical standards and that death will indicate irreversible loss of all brain
function. The patient has no neurologic activity upon clinical examination;
adjunctive tests such as EEG and cerebral blood flow (CBF) studies are often
used to confirm brain death (Lovasik, 2000). Many of these patients are
potential organ donors, and the nurse may provide information to the family and
assist them with this decision-making process about organ donation.
Related Topics