Chapter: Medical Surgical Nursing: Management of Patients With Neurologic Trauma
Nursing Process: The Patient With a Brain Injury

NURSING PROCESS: THE PATIENT WITH A BRAIN INJURY
Assessment
Depending on the
patient’s neurologic status, the nurse may elicit information from the patient,
family, or witnesses or from emer-gency rescue personnel (Munro, 2000).
Although it may not be possible to obtain all usual baseline data initially, the
immediate health history should include the following questions:
·
When did the injury occur?
·
What caused the injury? A
high-velocity missile? An object striking the head? A fall?
·
What was the direction and
force of the blow?
Since a history of unconsciousness or amnesia after a
head in-jury indicates a significant degree of brain damage, and since changes
that occur minutes to hours after the initial injury can re-flect recovery or
indicate the development of secondary brain damage, the nurse should try to
determine if there was a loss of consciousness, what the duration of the
unconscious period was, and if the patient could be aroused.
In addition to questions that establish the nature of the
injury and the patient’s condition immediately after the injury, the nurse
should examine the patient thoroughly. This assessment should include
determining the patient’s LOC, ability to respond to verbal commands (if
conscious), response to tactile stimuli (if unconscious), pupillary response to
light, status of corneal and gag reflexes, motor function, and Glasgow Coma
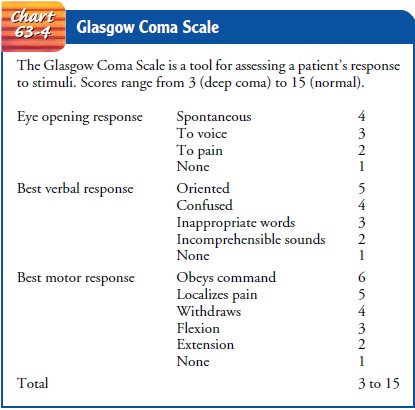
Scale score (Chart 63-4).
Additional detailed neurologic and systems assessments are made initially and at frequent intervals throughout the acute phase of care (Dibsie, 1998). The baseline and ongoing assess-ments are critical nursing interventions for the brain-injured patient, whose condition can worsen dramatically and irrevocably if subtle signs are overlooked. More information on assessment is provided below and in Figure 63-5 and Table 63-1.


Diagnosis
NURSING DIAGNOSES
Based on the assessment data, the patient’s major nursing
diag-noses may include the following:
·
Ineffective airway clearance
and impaired gas exchange re-lated to brain injury
·
Ineffective cerebral tissue
perfusion related to increased ICP and decreased CPP
·
Deficient fluid volume related
to decreased LOC and hor-monal dysfunction
·
Imbalanced nutrition, less
than body requirements, related to metabolic changes, fluid restriction, and
inadequate intake
·
Risk for injury (self-directed
and directed at others) related to seizures, disorientation, restlessness, or
brain damage
·
Risk for imbalanced
(increased) body temperature related to damaged temperature-regulating
mechanism
·
Potential for impaired skin
integrity related to bed rest, hemiparesis, hemiplegia, and immobility
·
Disturbed thought processes
(deficits in intellectual function, communication, memory, information
processing) related to brain injury
·
Potential for disturbed sleep
pattern related to brain injury and frequent neurologic checks
·
Potential for compromised
family coping related to un-responsiveness of patient, unpredictability of
outcome, pro-longed recovery period, and the patient’s residual physical and
emotional deficit
·
Deficient knowledge about
recovery and the rehabilitation process
The nursing diagnoses for the unconscious patient and the patient with increased ICP also apply.
COLLABORATIVE PROBLEMS/POTENTIAL COMPLICATIONS
Based on all the assessment data, the major complications
include the following:
·
Decreased cerebral perfusion
·
Cerebral edema and herniation
·
Impaired oxygenation and
ventilation
·
Impaired fluid, electrolyte,
and nutritional balance
·
Risk of post-traumatic
seizures
Planning and Goals
The goals for the patient may include maintenance of a
patent airway, adequate CPP, fluid and electrolyte balance, adequate
nutritional status, prevention of secondary injury, maintenance of normal body
temperature, maintenance of skin integrity, im-provement of cognitive function,
prevention of sleep deprivation, effective family coping, increased knowledge
about the rehabili-tation process, and absence of complications.
Nursing Interventions
The nursing interventions for the patient with a head
injury are extensive and diverse; they include making nursing assessments,
setting priorities for nursing interventions, anticipating needs and
complications, and initiating rehabilitation.
MONITORING FOR DECLINING NEUROLOGIC FUNCTION
The importance of ongoing assessment and monitoring of
the brain-injured patient cannot be overstated. The following para-meters are
assessed initially and as frequently as the patient’s condition requires. As
soon as the initial assessment is made, the use of a neurologic flow chart is
started and maintained.
Level of Consciousness
The LOC is regularly assessed because changes in it precede all other changes in vital and neurologic signs. The Glasgow Coma Scale, which is used to assess LOC, is based on the three criteria of eye opening, verbal responses, and motor responses to verbal commands or painful stimuli. It is particularly useful for monitoring changes during the acute phase, the first few days after a head injury. It does not take the place of an in-depth neurologic assessment; rather, it is used to monitor the patient’s motor, verbal, and eye-opening responses. The pa-tient’s best responses to predetermined stimuli are recorded (see Chart 63-4). Each response is scored (the greater the num-ber the better the functioning), and the sum of these scores gives an indication of the severity of coma and a prediction of possible outcome. The lowest score is 3 (least responsive); the highest is 15 (most responsive). A score of 8 or less is generally accepted as indicating a severe head injury (Teasdale & Jennett, 1974).
Vital Signs
Although a change in LOC is the most sensitive neurologic
indi-cation of deterioration of the patient’s condition, vital signs are
monitored at frequent intervals also to assess the intracranial sta-tus. Table
63-1 depicts the general assessment parameters for the patient with a head
injury.
Signs of increasing ICP
include slowing of the heart rate (bradycardia), increasing systolic blood
pressure, and widening pulse pressure. As brain compression increases,
respirations be-come rapid, the blood pressure may decrease, and the pulse
slows further. This is an ominous development, as is a rapid fluctuation of
vital signs (March, 2000). A rapid rise in body temperature is regarded as
unfavorable because hyperthermia increases the meta-bolic demands of the brain
and may indicate brain stem damage, a poor prognostic sign. The temperature is
maintained at less than 38°C (100.4°F). Tachycardia and arterial hypotension may indicate
that bleeding is occurring elsewhere in the body.
Motor Function
Motor function is
assessed frequently by observing spontaneous movements, asking the patient to
raise and lower the extremities, and comparing the strength and equality of the
hand grasp and pedal push at periodic intervals. To assess the hand grasp, the
nurse instructs the patient to squeeze the examiner’s fingers tightly. The
nurse assesses lower extremity motor strength (pedal push) by placing the hands
on the soles of the patient’s feet and asking the patient to push down against
the examiner’s hands. The presence or absence of spontaneous movement of each
extremity is also noted, and speech and eye signs are assessed.
If the patient does not
demonstrate spontaneous movement, responses to painful stimuli are assessed.
Motor response to pain is assessed by applying a central stimulus, such as
pinching the pectoralis major muscle, to determine the patient’s best response.
Peripheral stimulation may provide inaccurate assessment data because it may
result in a reflex movement rather than a voluntary motor response. Abnormal
responses (lack of motor response; extension responses) are associated with a
poorer prognosis.
Other Neurologic Signs
In addition to the patient’s spontaneous eye opening
evaluated with the Glasgow Coma Scale, the size and equality of the pupils and
their reaction to light are assessed. A unilaterally dilated and poorly
responding pupil may indicate a developing hematoma, with subsequent pressure
on the third cranial nerve due to shift-ing of the brain. If both pupils become
fixed and dilated, this in-dicates overwhelming injury and intrinsic damage to
the upper brain stem and is a poor prognostic sign.
The patient with a head
injury may develop focal nerve palsies such as anosmia (lack of sense of smell)
or eye movement abnor-malities and focal neurologic deficits such as aphasia,
memory deficits, and post-traumatic seizures or epilepsy. Patients may be left with
residual organic psychological deficits (impulsiveness, emotional lability, or
uninhibited, aggressive behaviors) and, as a consequence of the impairment,
lack insight into their emotional responses (Davis, 2000).
MAINTAINING THE AIRWAY
One of the most
important nursing goals in the management of the patient with a head injury is
to establish and maintain an ad-equate airway. The brain is extremely sensitive
to hypoxia, and a neurologic deficit can worsen if the patient is hypoxic.
Therapy is directed toward maintaining optimal oxygenation to preserve cerebral
function. An obstructed airway causes CO2
retention and hypoventilation, which can produce cerebral vessel dilation and
increased ICP.
Interventions to ensure an adequate exchange of air and
include the following:
·
Keep the unconscious patient
in a position that facilitates drainage of oral secretions, with the head of
the bed elevated about 30 degrees to decrease intracranial venous pressure
(Bader & Palmer, 2000).
·
Establish effective suctioning
procedures (pulmonary secre-tions produce coughing and straining, which
increase ICP).
·
Guard against aspiration and
respiratory insufficiency.
·
Closely monitor arterial blood
gas values to assess the ade-quacy of ventilation. The goal is to keep blood gas
values within the normal range to ensure adequate cerebral blood flow.
·
Monitor the patient who is
receiving mechanical ventilation.
·
Monitor for pulmonary
complications such as acute respi-ratory distress syndrome (ARDS) and pneumonia
(Munro, 2000).
MONITORING FLUID AND ELECTROLYTE BALANCE
Brain damage can produce metabolic and hormonal
dysfunctions. The monitoring of serum electrolyte levels is important,
especially in patients receiving osmotic diuretics, those with inappropriate
antidiuretic hormone secretion, and those with post-traumatic diabetes
insipidus.
Serial studies of blood
and urine electrolytes and osmolality are carried out because head injuries may
be accompanied by dis-orders of sodium regulation. Hyponatremia is common
follow-ing head injury due to shifts in extracellular fluid, electrolytes, and
volume. Hyperglycemia, for example, may cause an increase in extracellular
fluid that lowers sodium (Hickey, 2003). Hyper-natremia may also occur due to
sodium retention that may last several days, followed by sodium diuresis.
Increasing lethargy, confusion, and seizures may be due to electrolyte
imbalance.
Endocrine function is evaluated by monitoring serum
elec-trolytes, blood glucose values, and intake and output. Urine is tested
regularly for acetone. A record of daily weights is main-tained, especially if
the patient has hypothalamic involvement and is at risk for the development of
diabetes insipidus.
PROMOTING ADEQUATE NUTRITION
Head injury results in metabolic changes that increase calorie
consumption and nitrogen excretion (Donaldson et al., 2000). There is an
increased demand for protein. As soon as possible, nu-trition should be
provided. Early initiation of nutritional therapy has been shown to improve
outcomes in head-injured patients (Bader & Palmer, 2000). Parenteral
nutrition via a central line or enteral feedings administered via a nasogastric
or nasojejunal feeding tube may be used. If there is discharge of CSF from the
nose (CSF rhinorrhea), an oral feeding tube should be inserted in place of a
nasal tube.
Laboratory values should
be monitored closely in patients re-ceiving parenteral nutrition. Elevating the
head of the bed and as-pirating the enteral tube for evidence of residual
feeding before administering additional feedings can help prevent distention,
re-gurgitation, and aspiration. A continuous-drip infusion or pump may be used
to regulate the feeding. Enteral or par-enteral feedings are usually continued
until the swallowing reflex returns and the patient can meet caloric
requirements orally.
PREVENTING INJURY
As the patient emerges
from coma, there is often a period of lethargy and stupor followed by a period
of agitation. Each phase is variable and depends on the individual, the
location of the in-jury, the depth and duration of coma, and the patient’s age.
The patient emerging from a coma may become increasingly agitated toward the
end of the day. Restlessness may be due to hypoxia, fever, pain, or a full
bladder. It may indicate injury to the brain but may also be a sign that the
patient is regaining consciousness. (Some restlessness may be beneficial
because the lungs and extremities are exercised.) Agitation may also be due to
discomfort from catheters, intravenous lines, restraints, and repeated
neurologic checks. Alter-natives to restraints must be used whenever possible.
Strategies to prevent
injury include the following:
·
Assess the patient to ensure
that oxygenation is adequate and the bladder is not distended. Check dressings
and casts for constriction.
·
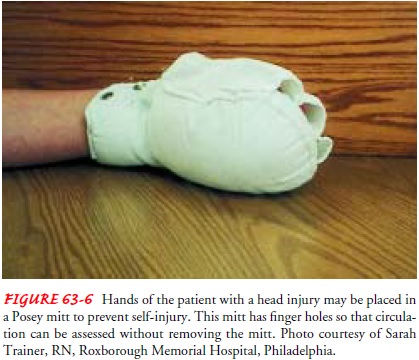
To protect the patient from
self-injury and dislodging of tubes, use padded side rails or wrap the
patient’s hands in mitts (Fig. 63-6). Restraints are avoided because straining
against them can increase ICP or cause other injury. En-closed or floor-level
specialty beds may be indicated.
·
Avoid using opioids as a means
of controlling restlessness because these medications depress respiration,
constrict the pupils, and alter responsiveness.
·
Minimize environmental stimuli
by keeping the room quiet, limiting visitors, speaking calmly, and providing
fre-quent orientation information (eg, explaining where the pa-tient is and
what is being done).
·
Provide adequate lighting to
prevent visual hallucinations.
·
Minimize disruption of the
patient’s sleep/wake cycles.
·
Lubricate the skin with oil or
emollient lotion to prevent irritation due to rubbing against the sheet.
·
If incontinence occurs,
consider use of an external sheath catheter on a male patient. Because
prolonged use of an in-dwelling catheter inevitably produces infection, the
patient may be placed on an intermittent catheterization schedule.
MAINTAINING BODY TEMPERATURE
An increase in body temperature in the head-injured
patient can be the result of damage to the hypothalamus, cerebral irritation
from hemorrhage, or infection. The nurse monitors the patient’s temperature
every 4 hours. If the temperature rises, efforts are undertaken to identify the
cause and to control it using acetamin-ophen and cooling blankets as prescribed
(Bader & Palmer, 2000). Cooling blankets should be used with caution so as
not to induce shivering, which increases ICP. If infection is suspected,
potential sites of infection are cultured and antibiotics are pre-scribed and
administered.
MAINTAINING SKIN INTEGRITY
Patients with traumatic head injury often require
assistance in turning and positioning because of immobility or
unconscious-ness. Prolonged pressure on the tissues will decrease circulation
and lead to tissue necrosis. Potential areas of breakdown need to be identified
early to avoid the development of pressure ulcers. Specific nursing measures
include the following:
·
Assess all body surfaces and
document skin integrity at least every 8 hours.
·
Turn and reposition the
patient every 2 hours.
·
Provide skin care every 4
hours.
·
Assist patient to get out of
bed to a chair three times a day if physically able.
IMPROVING COGNITIVE FUNCTIONING
Although many patients with head injury survive because
of re-suscitative and supportive technology, they frequently have sig-nificant
cognitive sequelae that may not be detected during the acute phase of injury.
Cognitive impairment includes memory deficits, decreased ability to focus and
sustain attention to a task (distractibility), reduced ability to process
information, and slow-ness in thinking, perceiving, communicating, reading, and
writ-ing. Psychiatric or emotional problems develop in as many as 44% of
patients with head injury (van Reekum et al., 2000). Re-sulting psychosocial,
behavioral, emotional, and cognitive im-pairments are devastating to the family
as well as to the patient (Davis, 2000; Perlesz, Kinsella, & Crowe, 1999).
These problems require collaboration among many
disciplines (Bader & Palmer, 2000). A neuropsychologist (specialist in
eval-uating and treating cognitive problems) plans a program and ini-tiates
therapy or counseling to help the patient reach maximal potential. Cognitive
rehabilitation activities help the patient to devise new problem-solving
strategies. The retraining is carried out over an extended period and may
include the use of sensory stimulation and reinforcement, behavior
modification, reality orientation, computer-training programs, and video games.
As-sistance from many disciplines is necessary during this phase of recovery.
Even if intellectual ability does not improve, social and behavioral abilities
may.
The patient recovering
from a brain injury may experience fluctuations in the level of cognitive
function, with orientation, attention, and memory frequently affected. When
pushed to a level greater than the impaired cortical functioning allows, the
patientmay show symptoms of fatigue, anger, and stress (headache, dizziness).
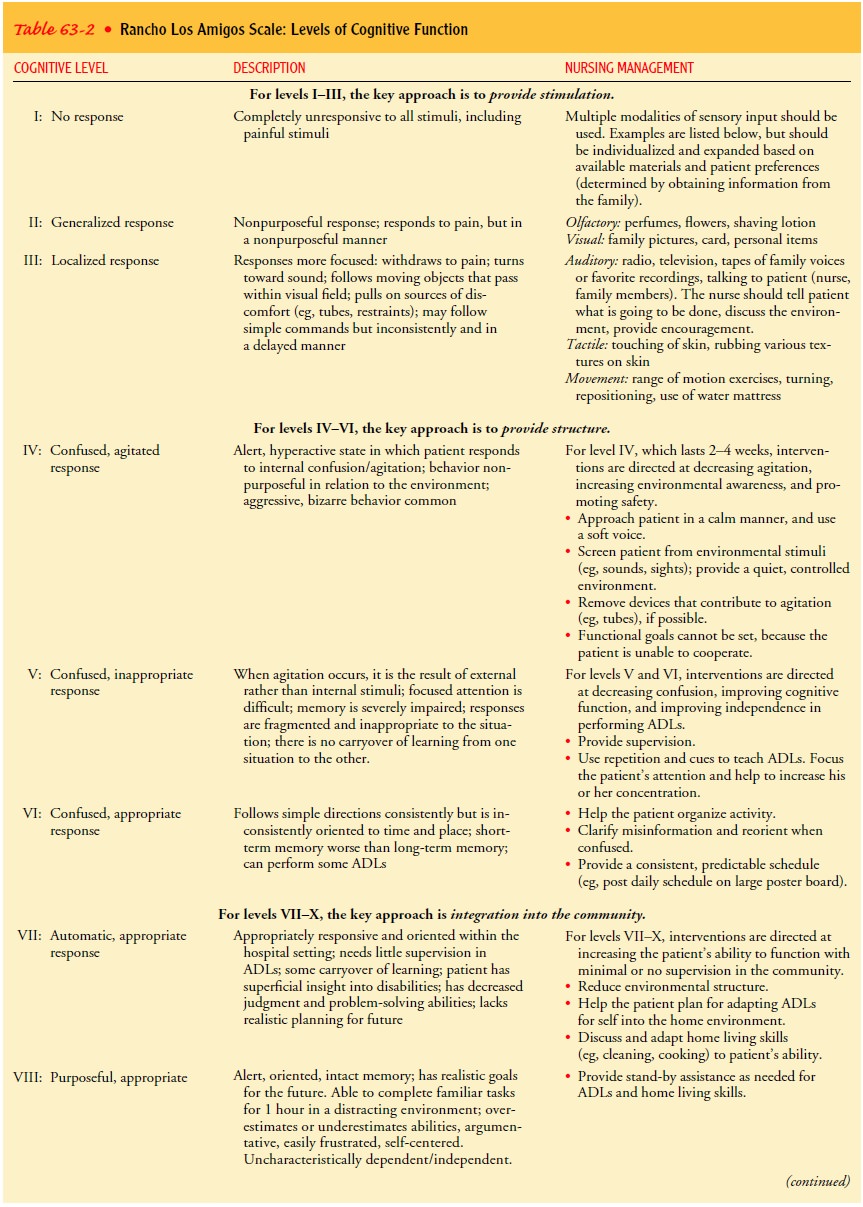
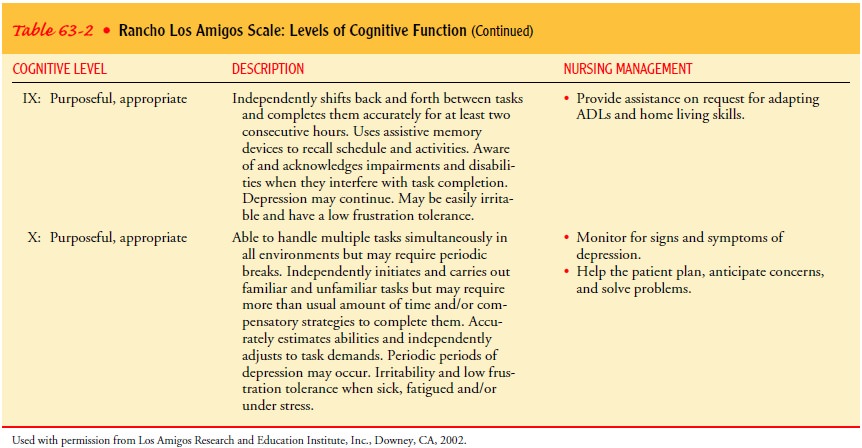
The Rancho Los Amigos Level of Cognitive Function is a scale frequently used to
assess cognitive function and evalu-ate ongoing recovery from head injury.
Nursing management and a description of each level are included in Table 63-2.
PREVENTING SLEEP PATTERN DISTURBANCE
Patients who require
frequent monitoring of neurologic status may experience sleep deprivation. They
are awakened hourly to assess LOC and as a result are deprived of long periods
of sleep and rest. In an effort to allow the patient longer times of
uninter-rupted sleep and rest, the nurse can group nursing care activities so
that the patient is disturbed less frequently. Environmental noise is decreased
and the room lights are dimmed. Back rubs and other activities to increase
comfort can assist in promoting sleep and rest.
SUPPORTING FAMILY COPING
Having a loved one
sustain a serious head injury can produce a great deal of prolonged stress in
the family. This stress can result from the patient’s physical and emotional
deficits, the unpre-dictable outcome, and altered family relationships.
Families report difficulties in coping with changes in the patient’s temperament,
behavior, and personality. Such changes are associated with dis-ruption in
family cohesion, loss of leisure pursuits, and loss of work capacity, as well
as social isolation of the caretaker. The family may experience anger, grief,
guilt, and denial in recurring cycles (Perlesz et al., 1999).
To promote effective
coping, the nurse can ask the family how the patient is different at this time:
What has been lost? What is most difficult about coping with this situation?
Helpful inter-ventions include providing family members with accurate and
honest information and encouraging them to continue to set well-defined,
mutual, short-term goals. Family counseling helps address the family members’
overwhelming feelings of loss and helplessness and gives them guidance for the
management of in-appropriate behaviors. Support groups help the family members
share problems, develop insight, gain information, network, and gain assistance
in maintaining realistic expectations and hope.
The National Head Injury
Foundation serves as a clearing-house for information and resources for
patients with head in-juries and their families, including specific information
on coma, rehabilitation, behavioral consequences of head injury, and fam-ily
issues. This organization can provide names of facilities and professionals who
work with patients with head injuries and can assist families in organizing
local support groups.
Many patients with
severe head injury die of their injuries, and many of those who survive
experience long-term problems that prevent them from resuming their previous
roles and functions. During the most acute phase of injury, family members need
sup-port and facts from the health care team.
Many individuals with
severe head injuries that result in brain death are young and otherwise healthy
and are therefore consid-ered for organ donation. Family members of patients
with such injuries need support during this extremely stressful time and
as-sistance in making decisions to end life support and permit do-nation of
organs. They need to know that the brain-dead patient whose respiratory and
cardiovascular systems are maintained through life support is not going to
survive and that the severe head injury, not the removal of the patient’s
organs or the re-moval of life support, is the cause of patient’s death.
Bereavement counselors and members of the organ procurement team areoften very
helpful to family members in making decisions about organ donation and in
helping them cope with stress.
MONITORING AND MANAGING POTENTIAL COMPLICATIONS
Decreased Cerebral Perfusion
Maintenance of adequate
CPP is important to prevent serious complications of head injury due to
decreased cerebral perfusion (Bader & Palmer, 2000; March, 2000). Adequate
CPP is greater than 70 mm Hg. Any decrease in this pressure can impair cerebral
perfusion and cause brain hypoxia and ischemia, leading to per-manent damage.
Therapy (eg, elevation of the head of the bed and increased intravenous fluids)
is directed toward decreasing cerebral edema and increasing venous outflow from
the brain. Systemic hypotension, which causes vasoconstriction and a
signif-icant decrease in CPP, is treated with increased intravenous fluids.
Cerebral Edema and Herniation
The patient with a head
injury is at risk for additional complica-tions such as increased ICP and brain
stem herniation. Cerebral edema is the most common cause of increased ICP in
the patient with a head injury, with the swelling peaking approximately 48 to
72 hours after injury. Bleeding also may increase the volume of contents within
the rigid closed compartment of the skull, causing increased ICP and herniation
of the brain stem and re-sulting in irreversible brain anoxia and brain death.
Impaired Oxygenation and Ventilation
Impaired oxygen and
ventilation may necessitate mechanical ven-tilatory support. The patient must
be monitored for a patent air-way, altered breathing patterns, and hypoxemia
and pneumonia. Interventions may include endotracheal intubation, mechanical
ventilation, and positive end-expiratory pressure.
Impaired Fluid, Electrolyte, and Nutritional Balance
Fluid, electrolyte, and
nutritional imbalances are common in the patient with a head injury. Common
imbalances may include hyponatremia, which is often associated with the
syndrome of in-appropriate secretion of antidiuretic hormone (see Chaps. 14 and
42), hypokalemia, and hyperglycemia (Hickey, 2003). Modifica-tions in fluid
intake with tube feedings or intravenous fluids may be necessary to treat these
imbalances. Insulin administra-tion may be prescribed to treat hyperglycemia.
Undernutrition is also a
common problem in response to the increased metabolic needs associated with
severe head injury. If the patient cannot eat, enteral feedings or parenteral
nutrition may be initiated within 24 hours of injury to provide adequate
calories and nutrients.
Post-traumatic Seizures
Patients with head injury are at an increased risk for post-traumatic seizures. Post-traumatic seizures are classified as im-mediate (within 24 hours of injury), early (within 1 to 7 days of injury), or late (more than 7 days following injury) (Kado & Patel, 1999). Seizure prophylaxis refers to the practice of administering antiseizure medications to patients following head injury to pre-vent seizures. It is important to prevent post-traumatic seizures, especially in the immediate and early phase of recovery, as seizures may increase ICP and decrease oxygenation.
Many antiseizure medications impair cognitive performance, prolonging the dura-tion of rehabilitation. Therefore, it is important to weigh the overall benefit of these medications against their side effects. Currently, there is no conclusive evidence that long-term antiseizure prophylaxis improves outcomes in patients with head in-jury. Research evidence supports the use of prophylactic antiseizure agents to prevent immediate and early seizure after head injury, but not for prevention of late seizures (Brain Trauma Foundation, American Association of Neurological Surgeons, Joint Section on Neurotrauma and Critical Care, 2000).
Nurses must assess patients carefully for the development
of post-traumatic seizures. Risk factors that increase the likelihood of
seizures are brain contusion with subdural hematoma, skull fracture, loss of
consciousness or amnesia of 1 day or more, and age over 65 years (Annegers
& Coan, 2000).
Other complications
after traumatic head injury include sys-temic infections (pneumonia, urinary
tract infection [UTI], sep-ticemia), neurosurgical infections (wound infection,
osteomyelitis, meningitis, ventriculitis, brain abscess), and heterotrophic
ossifi-cation (painful bone overgrowth in weight-bearing joints).
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care
Teaching early in the course of head injury often focuses
on re-inforcing information given to the family about the patient’s con-dition
and prognosis. As the patient’s status and expected outcome change over time,
family teaching may focus on interpretation and explanation of changes in the
patient’s physical and psycho-logical responses.
If the patient’s physical status allows him or her to be
dis-charged home, the patient and family are instructed about limi-tations that
can be expected and complications that may occur. Monitoring for complications
that merit contacting the neuro-surgeon is explained to the patient and family
verbally and in writing. Depending on the patient’s prognosis and physical and
cognitive status, the patient may be included in teaching about self-care
management strategies.
Because of the risk for post-traumatic seizures,
antiseizure med-ications may be prescribed for 1 to 2 years after injury. The
patient and family require instruction about the side effects of these
med-ications and about the importance of continuing to take them as prescribed.
Continuing Care
Rehabilitation of the
patient with a head injury begins at the time of injury and extends into the
home and community. Depending on the degree of brain damage, the patient may be
referred to a rehabilitation setting that specializes in cognitive
restructuring of the brain-injured patient. The patient is encouraged to continue
the rehabilitation program after discharge because improvement in status may
continue 3 or more years after injury. Changes in the head-injured patient and
the effects of long-term rehabilitation on the family and their coping
abilities need frequent assessment. Teaching and continued support of the
patient and family are es-sential as their needs and the patient’s status
change. Teaching points to address with the family of the head-injured patient
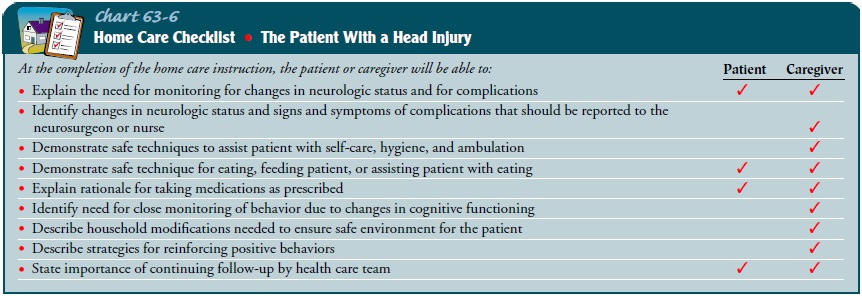
who is about to return home are described in Chart 63-6.
Depending on his or her status, the patient is encouraged
to return to normal activities gradually. Referral to support groups and the
National Head Injury Foundation may be warranted.
During the acute and rehabilitation phase of care, the
focus of teaching is on obvious needs, issues, and deficits. The nurse needs to
remind patients and family members of the need for continuing health promotion
and screening practices following these initial phases. Patients who have not
been involved in these practices in the past are educated about their
importance and are referred to appropriate health care providers.
Evaluation
EXPECTED PATIENT OUTCOMES
Expected patient outcomes may include:
1) Attains
or maintains effective airway clearance, ventilation, and brain oxygenation
a) Achieves
normal blood gas values and has normal breath sounds on auscultation
b) Mobilizes and clears secretions
2) Achieves
satisfactory fluid and electrolyte balance
a) Demonstrates
serum electrolytes within normal range
b) Has
no clinical signs of dehydration or overhydration
3) Attains
adequate nutritional status
a) Has
less than 50 mL of aspirate in stomach before each tube feeding
b) Is
free of gastric distention and vomiting
c) Shows
minimal weight loss
4) Avoids
injury
a) Shows
lessening agitation and restlessness
b) Is
oriented to time, place, and person
5) Does
not have a fever
6) Demonstrates
intact skin integrity
a) Exhibits
no redness or breaks in skin integrity
b) Exhibits
no pressure ulcers
7) Shows
improvement in cognitive function and improved memory
8) Demonstrates
normal sleep/wake cycle
9) Demonstrates
absence of complications
a) Exhibits
normal ICP, normal vital signs and body temperature, and increasing orientation
to time, place, and person
b) Demonstrates
reduced ICP
10) Patient
experiences no post-traumatic seizures
a) Takes
antiseizure medications as prescribed
b) Identifies
side effects/adverse effects of antiseizure medications
11) Demonstrate
adaptive coping mechanisms for family members
a) Join
support group
b) Share
feelings with appropriate health care personnel
c) Make
end-of-life decisions, if needed
12) Participate
in rehabilitation process as indicated for pa-tient and family members
a) Take
active role in identifying rehabilitation goals and participating in
recommended patient care activities
b) Prepare
for discharge of patient
Related Topics