Chapter: Medical Surgical Nursing: Management of Patients With Neurologic Trauma
Spinal Cord Injury
Spinal
Cord Injury
Spinal cord injury (SCI) is a major health problem. Nearly200,000 people in
the United States live each day with a dis-ability from SCI, with an estimated
11,000 new injuries occur-ring each year. SCI occurs almost four times more
often in males than females. Young people aged 16 to 30 suffer more than half
of the new SCIs each year. African Americans are at a higher risk than
Caucasians, with the incidence rising in recent years. The most common cause of
SCI is motor vehicle crashes, which ac-count for 35% of the injuries.
Violence-related injures account for nearly as many SCIs (30%), with falls
causing 19% and sports-related injuries causing 8% (CDC, 2001). There is a high
frequency of associated injuries and medical complications.
The predominant risk
factors for SCI include age, gender, and alcohol and drug use. The frequency
with which these risk fac-tors are associated with SCI serves to emphasize the
importance of primary prevention. The same interventions suggested earlier for
head injury prevention will serve to decrease the incidence of SCI as well (see
Chart 63-1) (CDC, 2001; Elovic & Kirschblum, 1999).
The vertebrae most
frequently involved in SCI are the 5th, 6th, and 7th cervical (neck), the 12th
thoracic, and the 1st lum-bar vertebrae. These vertebrae are the most
susceptible because there is a greater range of mobility in the vertebral
column in these areas (Dibsie, 1998).
Pathophysiology
Damage to the spinal cord ranges from transient
concussion (from which the patient fully recovers) to contusion, laceration,
and compression of the cord substance (either alone or in com-bination), to
complete transection of the cord
(which renders the patient paralyzed below the level of the injury).
SCIs can be separated
into two categories: primary injuries and secondary injuries (Porth, 2002).
Primary injuries are the re-sult of the initial insult or trauma and are
usually permanent. Sec-ondary injuries are usually the result of a contusion or
tear injury, in which the nerve fibers begin to swell and disintegrate. A
sec-ondary chain of events produces ischemia, hypoxia, edema, and hemorrhagic
lesions, which in turn result in destruction of myelin and axons (Hickey,
2003). These secondary reactions, believed to be the principal causes of spinal
cord degeneration at the level of injury, are now thought to be reversible 4 to
6 hours after injury. Therefore, if the cord has not suffered irreparable
damage, some method of early treatment is needed to prevent partial damage from
developing into total and permanent damage.
Clinical Manifestations
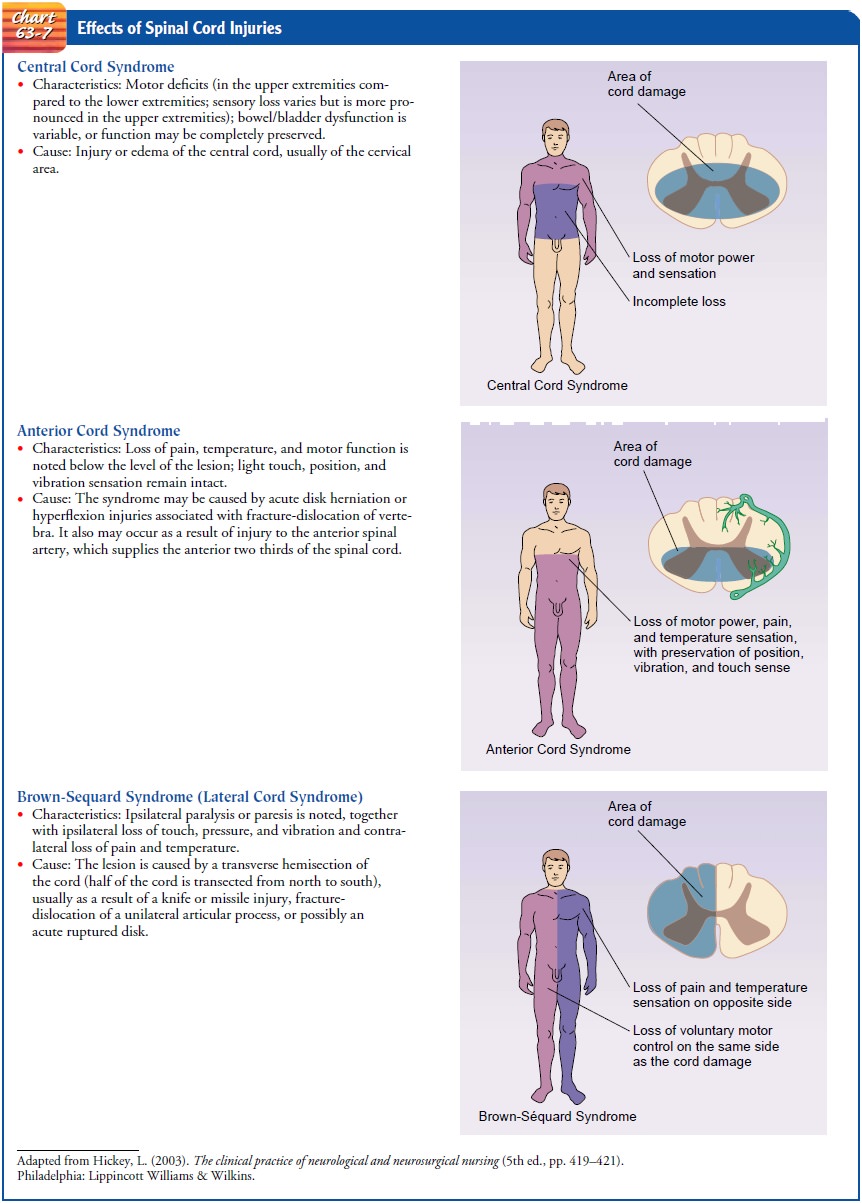
Manifestations depend on
the type and level of injury (Chart 63-7). The type of injury refers to the
extent of injury to the spinal cord itself. Incomplete spinal cord lesions are classified according to the area
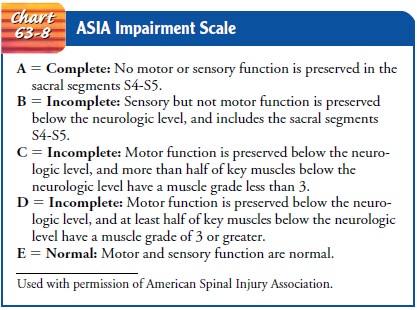
of spinal cord damage: central, lateral, anterior, or periph-eral. The American
Spinal Injury Association (ASIA) provides another standard classification of
SCI according to the degree of sensory and motor function present after injury
(Chart 63-8). “Neurologic level” refers to the lowest level at which sensory
and motor functions are normal. Below the neurologic level, there is total
sensory and motor paralysis, loss of bladder and bowel con-trol (usually with
urinary retention and bladder distention), loss of sweating and vasomotor tone,
and marked reduction of blood pressure from loss of peripheral vascular
resistance. A completespinal cord lesion
can result in paraplegia (paralysis
of the lowerbody) or quadriplegia
(paralysis of all four extremities).
If conscious, the patient usually complains of acute pain
in the back or neck, which may radiate along the involved nerve. Ab-sence of
pain, however, does not rule out spinal injury, and a care-ful assessment of
the spine should be done in the face of any significant mechanism of injury.
Often the patient speaks of fear that the neck or back is broken.
Respiratory dysfunction is related to the level of
injury. The muscles contributing to respiration are the abdominals and
in-tercostals (T1 to T11) and the diaphragm. In high cervical cord injury,
acute respiratory failure is the leading cause of death.
Assessment and Diagnostic Findings
A detailed neurologic examination is performed. Diagnostic x-rays (lateral cervical spine x-rays) and CT scanning are usually per-formed initially. An MRI scan may be ordered as a further work-up if a ligamentous injury is suspected, since significant spinal cord damage may exist even in the absence of bony injury. A search is made for other injuries, because spinal trauma often is accompanied by concomitant injuries, commonly to the head and chest. Continuous electrocardiographic monitoring may be indicated if a cord injury is suspected since bradycardia (slow heart rate) and asystole (cardiac standstill) are common in acute spinal injuries.
Emergency Management
The immediate management of the patient at the scene of
the in-jury is critical, because improper handling can cause further dam-age
and loss of neurologic function. Any patient involved in a motor vehicle or
diving injury, a contact sports injury, a fall, or any direct trauma to the
head and neck must be considered to have SCI until such an injury is ruled out.
Initial care must in-clude a rapid assessment, immobilization, extrication,
stabiliza-tion or control of life-threatening injuries, and transportation to
the most appropriate medical facility.
At the scene of the
injury, the patient must be immobilized on a spinal (back) board, with head and
neck in a neutral position, to prevent an incomplete injury from becoming
complete. One member of the team must assume control of the patient’s head to
prevent flexion, rotation, or extension; this is done by placing the hands on
both sides of the patient’s head at about the ear to limit movement and
maintain alignment while a spinal board or cer-vical immobilizing device is
applied. If possible, at least four peo-ple should slide the victim carefully
onto a board for transfer to the hospital. Any twisting movement may
irreversibly damage the spinal cord by causing a bony fragment of the vertebra
to cut into, crush, or sever the cord completely.
The patient must be referred to a regional spinal injury
or trauma center because of the multidisciplinary personnel and support
services required to counteract the destructive changes that occur in the first
few hours after injury. During treatment in the emergency and x-ray
departments, the patient is kept on the transfer board. The patient must always
be maintained in an ex-tended position. No part of the body should be twisted
or turned, nor should the patient be allowed to sit up. Once the extent of the
injury has been determined, the patient may be placed on a rotating bed (Fig.
63-7) or in a cervical collar (Fig. 63-8). Later, if SCI and bone instability
have been ruled out, the patient can be moved to a conventional bed or the
collar removed without harm. If a rotating bed is needed but not available, the
patient should be placed in a cervical collar and on a firm mattress with a
bedboard under it.
Management of Spinal Cord Injuries (Acute Phase)
The goals of management
are to prevent further SCI and to ob-serve for symptoms of progressive
neurologic deficits. The patient is resuscitated as necessary, and oxygenation
and cardiovascular stability are maintained. Many changes in the treatment of
SCI have occurred during the past 20 years. Treatments such as hypo-thermia,
corticosteroids, and naloxone were investigated and used during the 1980s; of
these, high-dose corticosteroids have shown the most promise, but their use
remains controversial (Short et al., 2000). Currently, regeneration therapy is
being investigated; this involves transplanting fetal tissue into the injured
spinal cord in hopes of regenerating the damaged tissue (Vacanti et al., 2001).
SCI continues to be a devastating event, and new treatment methods are
continually being investigated.
PHARMACOLOGIC THERAPY
In some studies, the administration of high-dose
corticosteroids, specifically methylprednisolone, has been found to improve
motor and sensory outcomes at 6 weeks, 6 months, and 1 year if given within 8
hours of injury (Hickey, 2003). In other studies, little improvement was found
(Short et al., 2000). Use of high-dose methylprednisolone, a corticosteroid, is
accepted as standard therapy in many countries and remains an established
clinical practice in most institutions in the United States (Bracken, 2000;
Hickey, 2003).
RESPIRATORY THERAPY
Oxygen is administered to maintain a high arterial PO2 because
hypoxemia can create or worsen a neurologic deficit of the spinal cord. If
endotracheal intubation is necessary, extreme care is taken to avoid flexing or
extending the patient’s neck, which can result in an extension of a cervical
injury.
In high cervical spine injuries, spinal cord innervation to the phrenic nerve, which stimulates the diaphragm, is lost. Diaphragmatic pacing (electrical stimulation of the phrenic nerve) attempts to stimulate the diaphragm to help the patient breathe. Diaphragmatic pacing may be considered for the patient with a high cervical lesion but is usually carried out after the acute phase.
SKELETAL FRACTURE REDUCTION AND TRACTION
Management of SCI requires immobilization and
reduction of dislocations (restoration of normal position) and stabilization of
the vertebral column.
Cervical fractures are reduced and the cervical spine is
aligned with some form of skeletal traction, such as skeletal tongs or
calipers, or with use of the halo device. Early surgical stabilization has
reduced the need for cervical traction in many patients with cervical spine
injuries (Gaebler et al., 1999). A variety of skeletal tongs are available, all
of which involve fixation in the skull in some manner (Fig. 63-9). The
Gardner-Wells tongs require no predrilled holes in the skull. Crutchfield and
Vinke tongs are in-serted through holes made in the skull with a special drill
under local anesthesia.
Traction is applied to the tongs by weights, the amount de-pending on the size of the patient and the degree of fracture displacement. The traction
force is exerted along the longitudinal axis of the vertebral bodies, with the
patient’s neck in a neutral position. The traction is then gradually increased
by adding more weights. As the amount of traction is increased, the spaces
be-tween the intervertebral disks widen and the vertebrae may slip back into
position. Reduction usually takes place after correct alignment has been restored.
Once reduction is achieved, as ver-ified by cervical spine x-rays and
neurologic examination, the weights are gradually removed until the amount of
weight needed to maintain the alignment is identified. The weights should hang
freely so as not to interfere with the traction. Traction is some-times
supplemented with manual manipulation of the neck by a surgeon to help achieve
realignment of the vertebral bodies.
A halo device may be
used initially with traction or may be ap-plied after removal of the tongs. It
consists of a stainless-steel halo ring that is fixed to the skull by four
pins. The ring is attached to a removable halo
vest, which suspends the weight of the unit cir-cumferentially around the
chest. A metal frame connects the ring to the chest. Halo devices provide
immobilization of the cervical spine while allowing early ambulation (Fig.
63-10).
Thoracic and lumbar injuries are usually treated with
surgical intervention followed by immobilization with a fitted brace. Traction
is not indicated either before or after surgery.
Surgical Management
Surgery is indicated in any of the following instances:
·
Compression of the cord is
evident.
·
The injury results in a
fragmented or unstable vertebral body.
·
The injury involves a wound
that penetrates the cord.
·
There are bony fragments in
the spinal canal.
·
The patient’s neurologic
status is deteriorating.
Surgery is performed to
reduce the spinal fracture or dislocation or to decompress the cord. A
laminectomy (excision of the pos-terior arches and spinous processes of a
vertebra) may be indi-cated in the presence of progressive neurologic deficit,
suspected epidural hematoma, bony fragments, or penetrating injuries that
require surgical débridement, or to permit direct visualization and exploration
of the cord. Vertebral bodies may also be surgi-cally fused to create a stable
spinal column.
Management of Complications of Spinal Cord Injury
SPINAL AND NEUROGENIC SHOCK
The spinal shock associated with SCI represents a sudden depression of reflex activity in the spinal cord (areflexia) below the level of injury. The muscles innervated by the part of the spinal cord segment below the level of the lesion are without sensation,paralyzed, and flaccid, and the reflexes are absent. In particular,the reflexes that initiate bladder and bowel function are affected. Bowel distention and paralytic ileus can be caused by depression of the reflexes and are treated with intestinal decompression by insertion of a nasogastric tube (Hickey, 2003).Neurogenic shock develops due to the loss of autonomic nervous system function below the level of the lesion (Hickey, 2003). The vital organs are affected, causing the blood pressure and heart rate to fall.
This loss of sympathetic innervation causes a variety of other clinical
manifestations, including a decrease in cardiac output, venous pooling in the
extremities, and peripheral vaso-dilation. In addition, the patient does not
perspire on the para-lyzed portions of the body because sympathetic activity is
blocked; therefore, close observation is required for early detection of an
abrupt onset of fever.
With injuries to the
cervical and upper thoracic spinal cord, innervation to the major accessory
muscles of respiration is lost and respiratory problems develop. These include
decreased vital capacity, retention of secretions, increased PaCO2
levels and de-creased oxygen levels, respiratory failure, and pulmonary edema
DEEP VEIN THROMBOSIS
Deep vein thrombosis (DVT) is a potential complication of
immobility and is common in patients with SCI. Patients who develop DVT are at
risk for pulmonary embolism (PE), a life-threatening complication. One estimate
from a meta-analysis of recent studies of the incidence of DVT and PE in SCI
patients put the rate at 6.3% for PE and 17.4% for DVT (Velmahos et al., 2000).
Manifestations of PE include pleuritic chest pain, anxiety, shortness of
breath, and abnormal blood gas values (increased PaCO2
and decreased PaO2).
Thigh and calf mea-surements are made daily. The patient is evaluated for the
presence of DVT if there is a significant increase in the cir-cumference of one
extremity. Low-dose anticoagulation ther-apy usually is initiated to prevent
DVT and PE, along with thigh-high elastic compression stockings or pneumatic com-pression
devices. In some cases, permanent indwelling filters may be placed in the vena
cava to prevent dis-lodged clots (emboli) from migrating to the lungs and
causing pulmonary emboli (Velmahos et al., 2000).
OTHER COMPLICATIONS
In addition to respiratory complications (respiratory
failure, pneu-monia) and autonomic
dysreflexia (characterized by pounding headache, profuse sweating, nasal
congestion, piloerection [“goose bumps”], bradycardia, and hypertension), other
complications that may occur include pressure ulcers and infection (urinary,
respiratory, and local infection at the skeletal traction pin sites) (Sullivan,
1999).
Related Topics