Chapter: Essential Anesthesia From Science to Practice : Applied physiology and pharmacology : Anesthesia and the lung
Mechanical ventilation
Mechanical ventilation
Many
patients require mechanical ventilation in the operating room or inten-sive
care unit. While an intubated patient can breathe spontaneously through an
endotracheal tube (which imposes significant resistance), many operative
proce-dures require muscle relaxation, making mechanical ventilation mandatory.
Most anesthesia machines are equipped with ventilators capable of providing
volume-or pressure-controlled ventilation. For volume-controlled ventilation,
the oper-ator sets a tidal volume, respiratory rate, and inspiratory to
expiratory time ratio (I : E ratio), and the ventilator does its
best to comply. If compliance deteriorates, the machine will generate
additional pressure (up to a set limit) in an attempt to deliver the desired
tidal volume. In pressure-controlled mode, as the name sug-gests, the selected
pressure will be maintained for a set time, which might mean variable tidal volumes,
depending on the patient’s pulmonary compliance and resistance.
In
general, ventilators used in the ICU offer more options than anesthesia machine
ventilators. For example, they might offer SIMV (synchronized inter-mittent
mandatory ventilation) in which the mechanical breath is synchronized with the
patient’s inspiratory effort, and the patient can breathe spontaneously between
mechanical breaths. SIMV is often combined with pressure support ven-tilation
(PSV), in which spontaneous respiratory efforts are met with a set level of
positive pressure, assisting with inhalation and designed to overcome the
resis-tance imposed by the endotracheal tube and ventilator.
Another
ventilator mode that requires explanation is continuous positive air-way
pressure (CPAP) and positive end-expiratory pressure (PEEP). Ordinarily, when
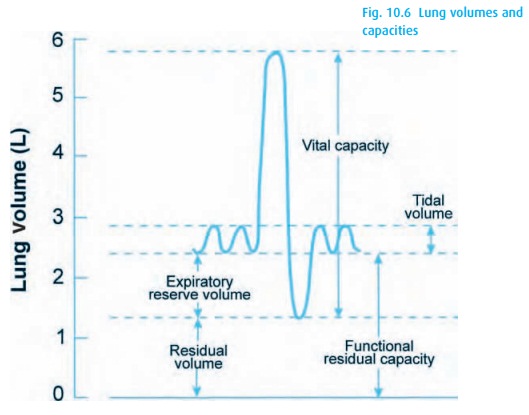
we exhale, some gas remains in the lungs (the FRC – see Fig. 10.6). Supine positioning and anesthesia reduce
the FRC, potentially resulting in hypoxemia. Normal FRC can be restored with the
addition of end-expiratory pressure, PEEP. It becomes particularly useful if
increased intra-abdominal pressure or extravas-cular fluid (pulmonary edema,
atelectasis, aspiration of gastric contents or res-piratory distress syndrome
(ARDS)) decreased FRC or caused collapse of alveoli. Two major factors limit
the amount of PEEP that we can apply: (i) the increase in intrathoracic
pressure will impede venous return; and (ii) the inspired tidal vol-ume is
administered on top of this baseline positive pressure, causing increased peak
inflation pressure and possibly barotrauma.
Related Topics