Chapter: Essential Anesthesia From Science to Practice : Applied physiology and pharmacology : Anesthesia and the lung
Matching of ventilation and perfusion
Matching of ventilation and perfusion
All the tubing leading to the alveoli – trachea, large bronchi, endotracheal tube – serves only as a conduit. These make up the deadspace volume: areas with bi-directional airflow but no gas exchange. There are three types of deadspace:
· physiologic – areas of the normal lung with ventilation but no perfusion – as found in the apices;
· anatomic – trachea and bronchi, which lack alveoli altogether;
· apparatus – the endotracheal tube and other pieces of tubing with bidirectionalgas flow.
An endotracheal tube will decrease the anatomic dead space generated by the pharynx, nose, and mouth. Applying a face mask will increase deadspace, but an anesthesia breathing circuit will add relatively little to the deadspace as long as the valves in the circuit function normally. The deadspace to tidal volume ratio is measured as:
VD/ VT=(PAC O2− PE C O2)/ PAC O2
where VD= deadspace volume, PACO2= alveolar CO2 and PE CO2= mixed expired CO2. A normal VD/VT ratio should not exceed 0.3.
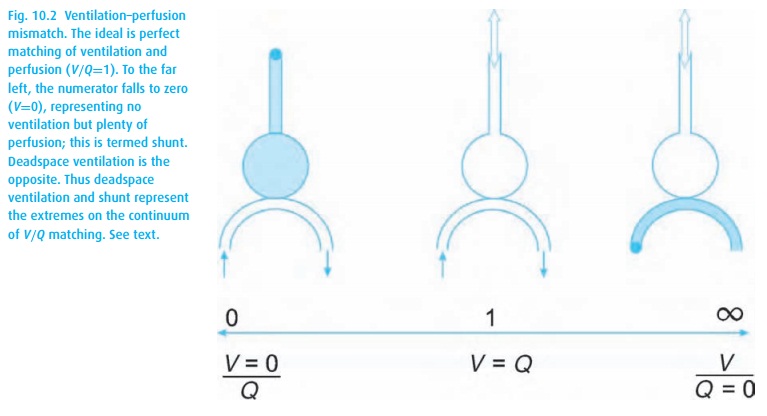
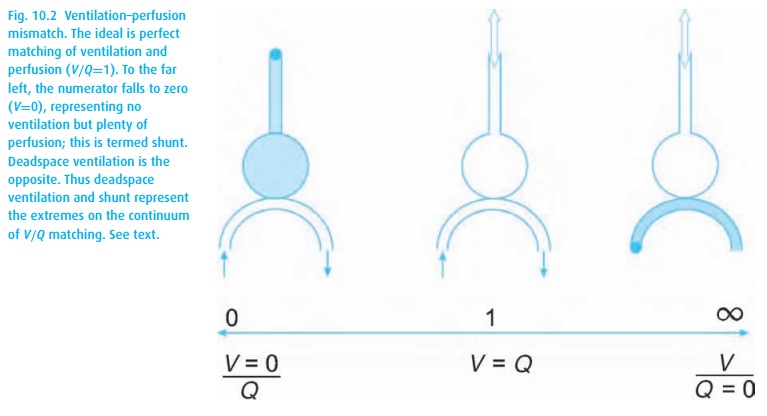
When pulmonary arterial blood manages to pass through the lungs without picking up oxygen or delivering carbon dioxide, we are referring to shunting. A shunt wastes perfusion. Typically, the difference between arterial and end-expired gases increases when ventilation and perfusion are mismatched, either owing to deadspace ventilation (inspired gas returns without having picked up carbon dioxide or delivered oxygen) or to shunting (pulmonary arterial blood bypasses alveoli and then dumps blood high in CO2 and low in O2 into the pulmonary venous blood, see Fig. 10.2). Even normal lungs have some deadspace ventilation and shunting. When either becomes excessive, we refer to a V/Q mismatch evident in abnormal blood gas values.
Related Topics