Chapter: Clinical Dermatology: Skin tumours
Lymphomas and leukaemias
Lymphomas
and leukaemias
Skin
involvement falls into two broad categories:
1 Disorders
which arise in the skin or preferentially involve it. These include:
ÔÇó
T-cell lymphoma (mycosis fungoides);
ÔÇó
S├ęzary syndrome; and
ÔÇó
lymphoma associated with HIV
infection.
2 Those
arising extracutaneously, but which some-times involve the skin. These include:
ÔÇó
HodgkinÔÇÖs disease;
ÔÇó
B-cell lymphoma; and
ÔÇó
leukaemia.
Cutaneous T-cell lymphoma (CTCL; sometimes called mycosis fungoides)
This
lymphoma of skin-associated helper T lympho-cytes usually evolves slowly. There
are three clinical phases: the patch, plaque and tumour stages, with
involvement of lymph nodes and other tissues occur-ring late in the disease.
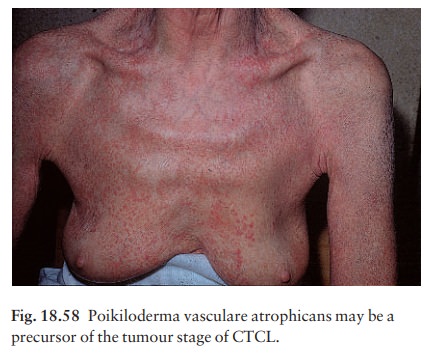
The patch stage (formerly termed ÔÇśpremycoticÔÇÖ to denote an early phase of mycosis fungoides) may last for years (see Fig. 6.9). Most commonly it consists of scattered, barely palpable, erythematous, slightly pig-mented, sharply marginated scaly patches rather like psoriasis or seborrhoeic dermatitis. Often they have a bizarre outline (e.g. arciform, or horseshoe-shaped) and, on close inspection, atrophy with surface wrin-kling is usually evident. Their distribution is usually asymmetrical. Less commonly, the patch stage can be a widespread poikiloderma, with atrophy, pigmenta-tion and telangiectasia (Fig. 18.58). As the lymphoma develops, some patches become indurated and pal-pable: the plaque stage. Some then turn into frank tumours which may become large (occasionally like mushrooms, hence the term ÔÇśmycosis fungoidesÔÇÖ) and ulcerate (Fig. 18.59).

The patch stage of CTCL may be difficult to diagnose clinically,
but the plaque and tumour stages are usually characteristic. The first two
phases of the disease may occupy 20 years or more, but the tumour stage is
often short, with spread and death usually within 3 years.
The
S├ęzary syndrome is also a CTCL caused by a proliferation of helper T
lymphocytes. Generalized skin erythema and oedema is associated with pruritus
and lymphadenopathy. Abnormal T lymphocytes, with large convoluted nuclei, are
found circulating in the blood (ÔÇśS├ęzary cellsÔÇÖ).
Histology
The histological hallmarks of plaque stage CTCL are:
ÔÇó
intraepidermal lymphocytic
microabscesses (Pautrier microabscesses);
ÔÇó
a band of lymphoid cells in the
upper dermis, infiltrating the epidermis; and
ÔÇó
atypical lymphocytes.
The
histology of the patch stage poses more problems
and
may differ little from dermatitis. Immunopheno-typing and T-cell receptor gene
rearrangement studies are not always
helpful in reaching a definitive diagnosis. Many biopsies, over several years,
may be needed to prove that a suspicious rash is indeed an early stage of CTCL.
Differential diagnosis
The
patch and plaque stages may be mistaken for pso-riasis or parapsoriasis ,
seborrhoeic der-matitis or tinea
corporis. However, they respond poorly to treatment for these disorders; the
bizarre shapes of the patches and their asymmet-rical distribution often raise
suspicion. In the early stages skin scrapings may be needed to exclude tinea.
Treatment
Moderately
potent or potent local steroids, and UVB treatment, may provide prolonged
palliation in the patch stage. In the plaque stage, PUVA, oral retinoids and ╬▒-interferon are helpful. If lesions become more indurated,
electron beam therapy may be used. Top-ical nitrogen mustard paint has also
been used with success in both patch and plaque stages. Individual tumours
respond well to low-dose radiotherapy. Systemic chemotherapy is disappointing.
Extracutaneous lymphomas
HodgkinÔÇÖs disease
This is of interest to dermatologists because it may present with severe generalized pruritus .
Patients
with unexplained pruritus must be examined for lymphadenopathy and
hepatosplenomegaly. Only rarely does HodgkinÔÇÖs disease affect the skin
directly, as small nodules and ulcers.
Leukaemia
Rarely,
the first sign of leukaemia is a leukaemic infiltrate in the skin. Clinically,
this shows as plum-coloured plaques or nodules or, less often, a thicken-ing
and rugosity of the scalp (cutis verticis gyratum). More often, the rashes
associated with leukaemia are non-specific red papules (ÔÇśleukaemidsÔÇÖ). Other
non-specific manifestations include pruritus, herpes zoster, acquired
ichthyosis and purpura.
B-cell lymphomas
B-lymphocytic lymphomas presenting with skin lesions are rare. They appear as scattered plum-coloured nodules (Fig. 18.60). Histologically, a B-cell lymphoma infiltrates the lower dermis in a nodular or diffuse manner. Immunophenotyping shows a monoclonal expansion of B lymphocytes. Treatment is with radio-therapy and systemic chemotherapy.

Related Topics