Chapter: Clinical Dermatology: Skin tumours
Basal cell carcinoma (rodent ulcer)
Malignant epidermal tumours
Basal cell carcinoma (rodent ulcer)
This
is the most common form of skin cancer. It crops up most commonly on the faces
of the middle-aged or elderly. Lesions invade locally but, for practical
purposes, never metastasize.
Cause
Prolonged
sun exposure is the main factor so these tumours are most common in white
people living near the equator. They may also occur in scars caused by X-rays,
vaccination or trauma. Photosensitizing pitch, tar and oils can act as
cocarcinogens with ultraviolet radiation. Previous treatment with arsenic, once
pre-sent in many ÔÇśtonicsÔÇÖ, predisposes to multiple basal cell carcinomas, often
after a lag of many years.
Multiple
basal cell carcinomas are found in the naevoid basal cell carcinoma syndrome
(GorlinÔÇÖs syndrome) where they may be associated with pal
The
syndrome is inherited as an autosomal dominant trait and recent studies
indicate that the genetic abnormality lies on chromo-some 9q.
Presentation
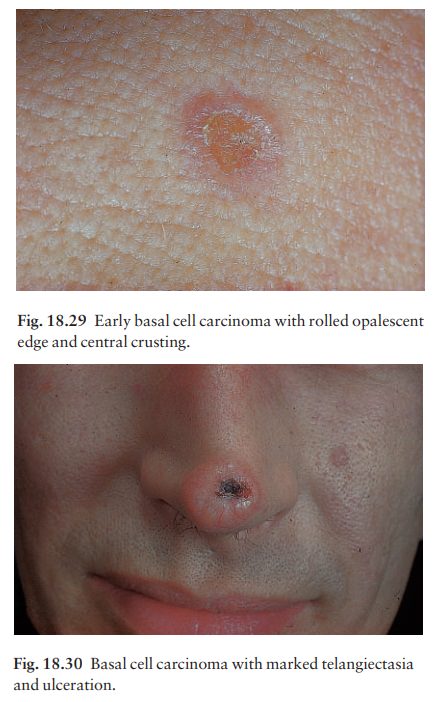
Nodulo-ulcerative.
This is the most common type.An early lesion is a small glistening translucent
skin-coloured papule that slowly enlarges. Central necrosis, although not
invariable, leaves an ulcer with an adherent crust and a rolled pearly edge
(Fig. 18.29). Fine telangiectatic vessels often run across the tumourÔÇÖs surface
(Fig. 18.30). Without treatment such lesions may reach 1ÔÇô2 cm in diameter in
5ÔÇô10 years.
Cystic.
The lesion is at first like the nodular type,but later cystic changes
predominate and the nodule becomes tense and more translucent, with marked
telangiectasia.
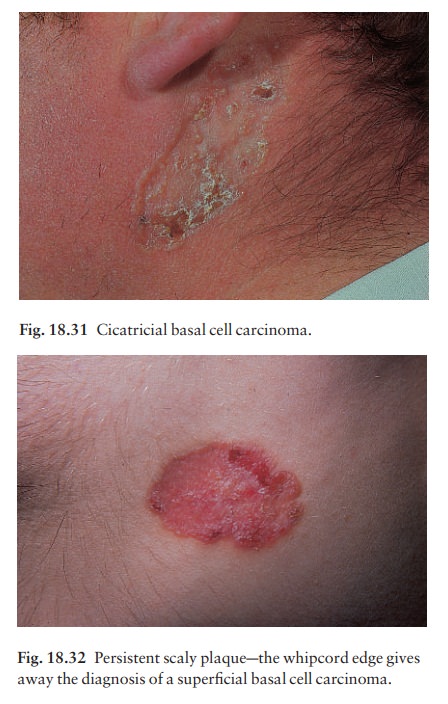
Cicatricial
(morphoeic). These are slowly expandingyellow or white waxy plaques
with an ill-defined edge. Ulceration and crusting, followed by fibrosis, are
common, and the lesion may look like an enlarg-ing scar (Fig. 18.31).
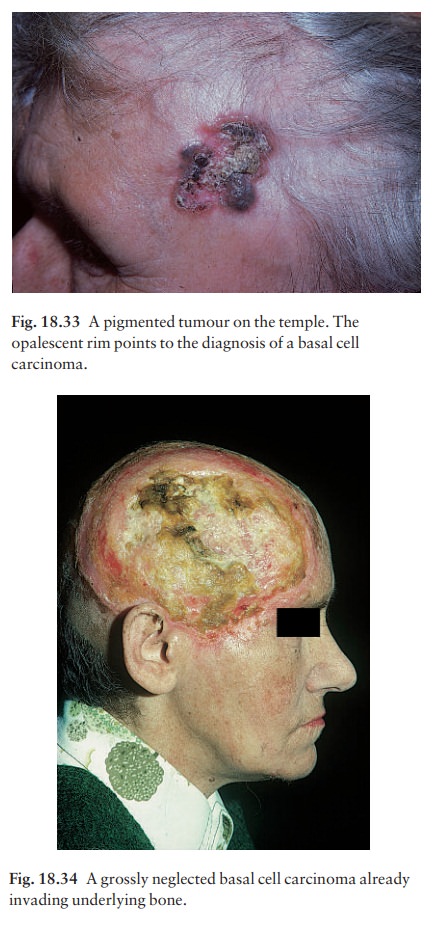
Superficial
(multicentric). These arise most often onthe trunk. Several lesions may be
present, each expanding slowly as a pink or brown scaly plaque with a fine
ÔÇśwhipcordÔÇÖ edge (Fig. 18.32). Such lesions can grow to more than 10 cm in
diameter.
Pigmented. Pigment may be present in all types ofbasal cell carcinoma causing all or part of the tumour to be brown or have specks of brown or black within it (Fig. 18.33).
Clinical course
The slow but relentless growth destroys tissue locally. Untreated, a basal cell carcinoma can invade underly-ing cartilage or bone (Fig. 18.34) or damage import-ant structures such as the tear ducts.
Histology
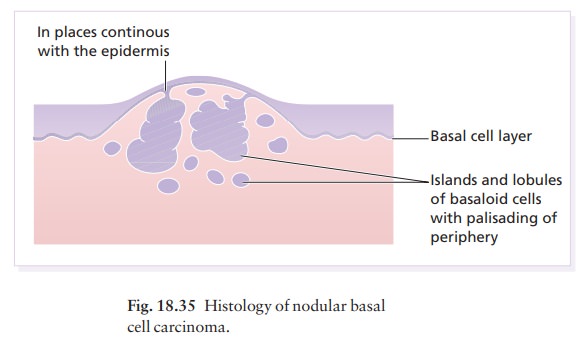
Small,
darkly blue staining basal cells grow in well-defined aggregates which invade
the dermis (Fig. 18.35). The outer layer of cells is arranged in a palisade.
Num-erous mitoses and apoptotic bodies are seen. In the cicatricial type the
islands of tumour are surrounded by fibrous tissue.
Differential diagnosis
A
nodular basal cell carcinoma may be confused with an intradermal melanocytic
naevus, a squamous cell carcinoma, a giant molluscum contagiosum or a
keratoacanthoma. Pigmented basal cell carcino-mas should be distinguished from
seborrhoeic warts and malignant melanomas. A cicatricial basal cell carcinoma
may mimic morphoea or a scar. A
superficial basal cell carcinoma may be confused with an intraepidermal
carcinoma, with psoriasis (Chap-ter 5) or with nummular eczema.
Treatment
There
is no single treatment of choice for all basal cell carcinomas. Treatment
should be tailored to the type of tumour, its site and the age and general
health of the patient. Published guidelines are very useful (see Further
reading).
In
general, excision, with 0.5 cm of surrounding normal skin, is the treatment of
choice for discrete nodular and cystic tumours in patients under 60 years.
Cicatricial tumours, with their ill-defined edges, and lesions near vital
structures, should be excised by specialist surgeons. MohsÔÇÖ micrographic
surgical technique is highly effective; it includes careful histo-logical
checks in all planes of tissue excised during the operation. MohsÔÇÖ surgery is
also becom-ing the treatment of choice for large (> 1 cm)
tumours and for those on cosmetically important sites, such as the nose, and
for tumours in certain anatomical areas, such as the inner canthus and the
nasolabial folds. Radiotherapy is also effective; it is seldom used now for
biopsy-proven lesions in patients under 70 years, but is helpful when surgery
is contraindicated. Cryo-therapy, curettage and cautery and photodynamic
therapy are sometimes useful for superficial lesions. Sometimes palliative
treatment with curettage and cautery may be preferable to aggressive treatment
for elderly patients in poor health; nowadays there is seldom justification for
doing nothing. The 5-year cure rate for all types of basal cell carcinoma is
over 95%, but regular follow-up is necessary to detect local recurrences when
they are small and remediable.
Related Topics