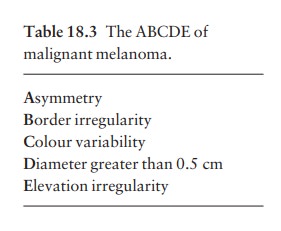
Chapter: Clinical Dermatology: Skin tumours
Benign
Benign
Viral warts
These
are discussed earily, but are mentioned here for two reasons: first, solitary
warts are some-times misdiagnosed on the face or hands of the elderly; and,
secondly, a wart is one of the few tumours in humans that is, without doubt,
caused by a virus. Seventy per cent of transplant patients who have been
immunosuppressed for over 5 years have multiple viral warts and there is
growing evidence that immunosup-pression, viral warts and ultraviolet radiation
interact in this setting to cause squamous cell carcinoma.
Squamous cell papilloma
This common tumour, arising from keratinocytes, may resemble a viral wart clinically. Sometimes an excessive hyperkeratosis produces a horn-shaped excrescence (a ÔÇścutaneous hornÔÇÖ). Excision, or curettage with cautery to the base, is the treatment of choice. The histology should be checked.
Seborrhoeic keratosis (basal cell papilloma, seborrhoeic wart)
This
is a common benign epidermal tumour, unrelated to sebaceous glands. The term
ÔÇśsenile wartÔÇÖ should be avoided as it offends many patients.
Cause
Usually
unexplained but:
ÔÇó
multiple lesions may be inherited
(autosomal dominant);
ÔÇó
occasionally follow an inflammatory
dermatosis; or
ÔÇó
very rarely, the sudden eruption of
hundreds of itchy lesions is associated with an internal neoplasm (LeserÔÇôTr├ęlat
sign).
Presentation
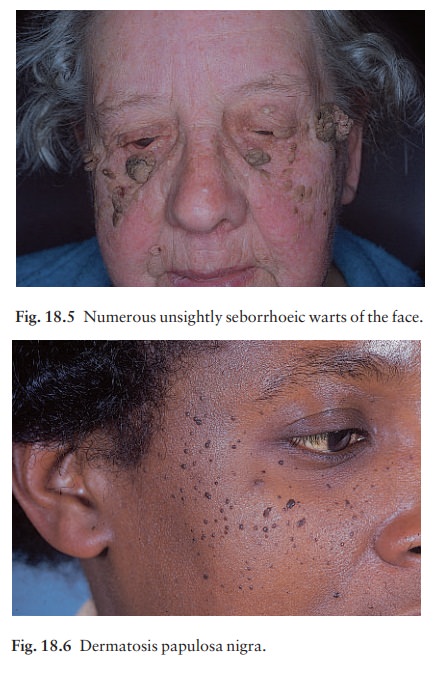
Seborrhoeic
keratoses usually arise after the age of 50 years, but flat inconspicuous
lesions are often visible earlier. They are often multiple (Figs 18.4 and 18.5)
but may be single. Lesions are most common on the face and trunk. The sexes are
equally affected.
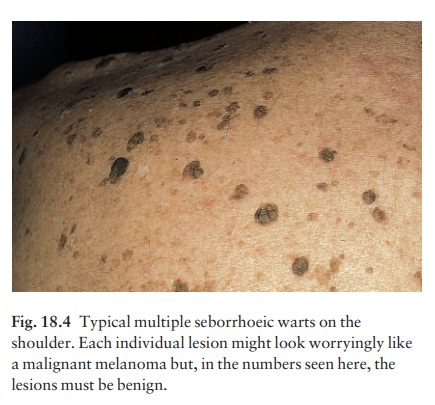
Physical
signs:
ÔÇó
a distinctive ÔÇśstuck-onÔÇÖ appearance;
may be flat, raised or pedunculated;
ÔÇó
colour varies from yellow to dark
brown; and
ÔÇó
surface may have greasy scaling and
scattered keratin plugs (ÔÇścurrant bunÔÇÖ appearance).
Clinical course
Lesions
may multiply with age but remain benign.
Differential diagnosis
Seborrhoeic keratoses are easily recognized. Occa-sionally they can be confused with a pigmented cel-lular naevus, a pigmented basal cell carcinoma and, most importantly, with a malignant melanoma. Some Afro-Caribbeans have many dark warty papules on their faces (dermatosis papulosa nigra; Fig. 18.6). Histologically these are like seborrhoeic warts.
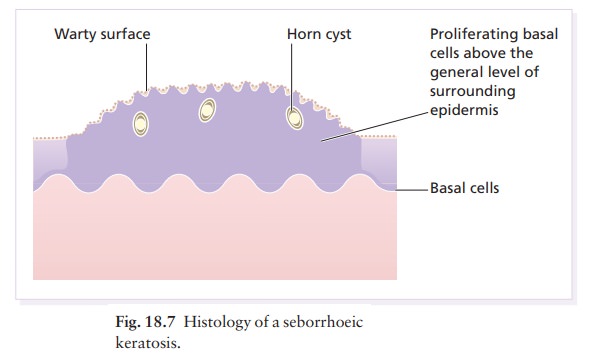
Investigations
Biopsy
is needed only in rare dubious cases. The his-tology is diagnostic (Fig. 18.7):
the lesion lies above the general level of the surrounding epidermis and
consists of proliferating basal cells and horn cysts.
Treatment
Seborrhoeic
keratoses can safely be left alone, but ugly or easily traumatized ones can be
removed with a curette under local anaesthetic (this has the advantage of
providing histology), or by cryotherapy.
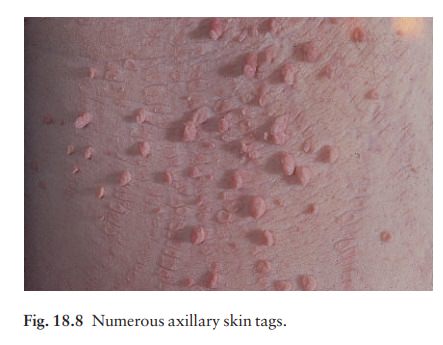
Skin tags (acrochordon)
These
common benign outgrowths of skin affect mainly the middle-aged and elderly.
Cause
This
is unknown but the trait is sometimes familial. Skin tags are most common in
obese women, and rarely are associated with tuberous sclerosis, acan-thosis
nigricans or acromegaly, and diabetes.
Presentation and clinical course
Skin
tags occur around the neck and within the major flexures. They look unsightly
and may catch on clothing and jewellery. They are soft skin-coloured or
pigmented pedunculated papules (Fig. 18.8).
Differential diagnosis
The
appearance is unmistakable. Tags are rarely confused with small melanocytic
naevi.
Treatment
Small lesions can be snipped off with fine scissors, frozen with liquid nitrogen, or destroyed with a hyfre-cator without local anaesthesia. There is no way of preventing new ones from developing.
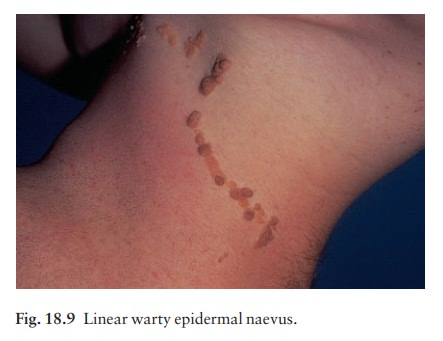
Linear epidermal naevus
These
lesions are an example of cutaneous mosaicism
and so tend to follow BlaschkoÔÇÖs lines (Fig. 18.9).
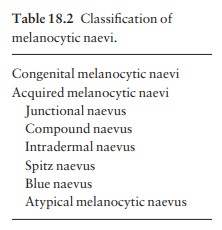
Melanocytic naevi
The
term ÔÇśnaevusÔÇÖ refers to a lesion, often present at birth, which has a local
excess of one or more normal constituents of the skin. Melanocytic naevi
(moles) are localized benign proliferations of melanocytes. Their
classification (Table 18.2) is based on the site of the aggregations of naevus
cells (Fig. 18.10).
Cause and evolution
The cause is unknown. A genetic factor is likely in many families, working together with excessive sun exposure during childhood.
With
the exception of congenital melanocytic naevi , most appear in early childhood,
often with a sharp increase in numbers during adolescence. Further crops may
appear during pregnancy, oestro-gen therapy or, rarely, after cytotoxic
chemotherapy and immunosuppression, but new lesions come up less often after
the age of 20 years.
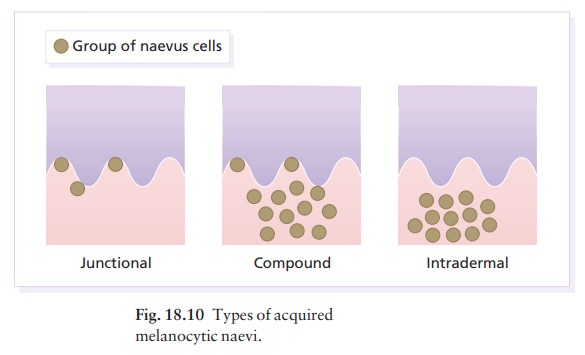
Melanocytic
naevi in childhood are usually of the ÔÇśjunctionalÔÇÖ type, with proliferating
melanocytes in clumps at the dermo-epidermal junction. Later, the melanocytes
round off and ÔÇśdropÔÇÖ into the dermis. A ÔÇścompoundÔÇÖ naevus has both dermal and
junc-tional components. With maturation the junctional component disappears so
that the melanocytes in an ÔÇśintradermalÔÇÖ naevus are all in the dermis (Fig.
18.10).
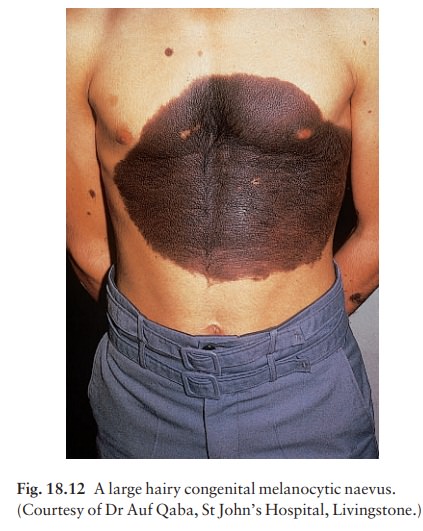
Presentation
Congenital melanocytic naevi (Figs 18.11 and 18.12).These are present at birth or appear in the neonatal period and are seldom less than 1 cm in diame-ter. Their colour varies from brown to black or blue-black. With maturity some become protuberant and hairy, with a cerebriform surface. Such lesions can be disfiguring, e.g. a ÔÇśbathing trunkÔÇÖ naevus, and carry an increased risk of malignant transformation

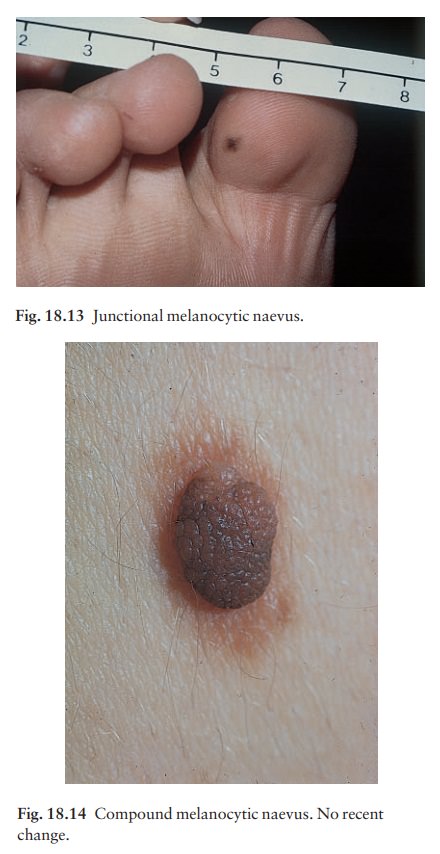
Junctional
melanocytic naevi (Fig. 18.13). These areroughly
circular macules. Their colour ranges from mid to dark brown and may vary even
within a single lesion. Most naevi of the palms, soles and genitals are of this
type.
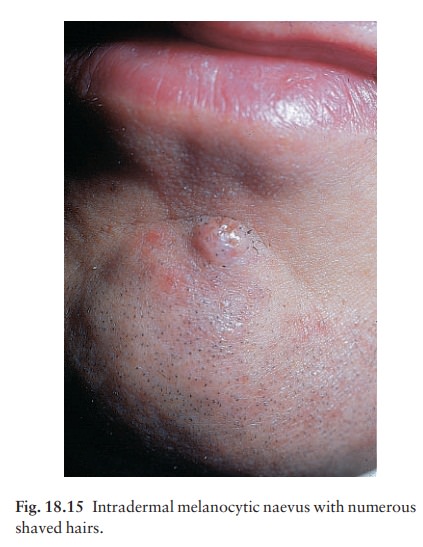
Compound melanocytic naevi (Fig. 18.14). These aredomed pigmented nodules of up to 1 cm in diameter. They may be light or dark brown but their colour is more even than that of junctional naevi. Most are smooth, but larger ones may be cerebriform, or even hyperkeratotic and papillomatous; many bear hairs.
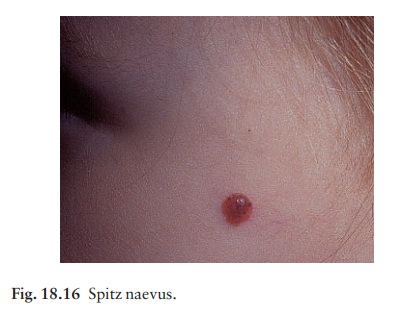
Intradermal
melanocytic naevi (Fig. 18.15). Theselook like
compound naevi but are less pigmented and often skin-coloured.
Spitz
naevi (juvenile melanomas; Fig. 18.16). Theseare usually found in
children. They develop over a month or two as solitary pink or red nodules of
up to 1 cm in diameter and are most common on the face and legs. Although
benign, they are often excised because of their rapid growth.
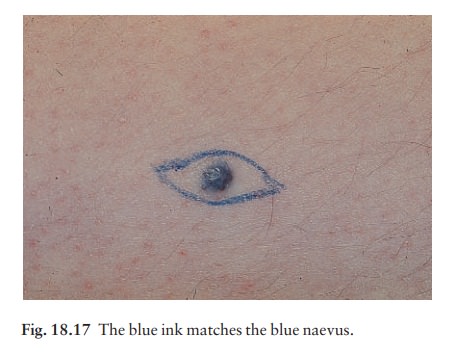
Blue
naevi (Fig. 18.17). So-called because of theirstriking slate
grey-blue colour, blue naevi usually
appear
in childhood and adolescence, on the limbs, buttocks and lower back. They are
usually solitary.
Mongolian
spots. Pigment in dermal melanocytes isresponsible for these
bruise-like greyish areas seen on the lumbosacral area of most DownÔÇÖs syndrome
and many Asian and black babies. They usually fade during childhood.
Atypical mole syndrome (dysplastic naevus syndrome;Fig. 18.18).

Clinically atypical melanocytic naevi can occur
sporadically or run in families as an autosomal dominant trait, with incomplete
penetrance, affecting several generations. Some families with atypical naevi
are melanoma-prone. Genes for susceptibility to melanoma have been mapped to
chromosomes 1p36 and 9p13 in a few of these families. The many large
irregularly pigmented naevi are most obvious on the trunk but some may be
present on the scalp. Their edges are irregular and they vary greatly in
sizeamany being over 1 cm in diameter. Some are pinkish and an inflamed halo
may surround them. Some have a mamillated surface. Patients with multiple
atypical melanocytic or dysplastic naevi with a positive family history of
malignant melanoma should be followed up 6-monthly for life.
Differential diagnosis of melanocytic naevi
ÔÇó
Malignant melanomas. This is
the most importantpart of the differential diagnosis. Melanomas are very rare
before puberty, single and more variably pigmented and irregularly shaped
(other features are listed below under Complications).
ÔÇó
Seborrhoeic keratoses. These
can cause confusionin adults but have a stuck-on appearance and are warty.
Tell-tale keratin plugs and horny cysts may be seen with the help of a lens.
ÔÇó
Lentigines. These may be found on any part of
theskin and mucous membranes. More profuse than junctional naevi, they are
usually grey-brown rather than black, and develop more often after adolescence.
ÔÇó
Ephelides (freckles). These are tan macules
less than
5
mm in diameter. They are confined to sun-exposed areas, being most common in
blond or red-haired people.
ÔÇó
Haemangiomas. Benign proliferations of
bloodvessels, including haemangiomas and pyogenic gran-ulomas, may be confused
with a vascular Spitz naevus or an amelanotic melanoma.
Histology
Most acquired lesions fit into the scheme given in Fig. 18.10: orderly nests of benign naevus cells are seen in the junctional region, in the dermis, or in both. However, some types of melanocytic naevi have their own distinguishing features. In congenital naevi the naevus cells may extend to the subcutaneous fat, and hyperplasia of other skin components (e.g. hair follicles) may be seen.
A Spitz naevus has a histology worry-ingly similar to that of a
melanoma. It shows dermal oedema and dilatated capillaries, and is composed of
large epithelioid and spindle-shaped naevus cells, some of which may be in
mitosis.
In
a blue naevus, naevus cells are seen in the mid and deep dermis.
The
main features of clinically atypical (ÔÇśdysplasticÔÇÖ) naevi are lengthening and
bridging of rete ridges, and the presence of junctional nests showing
melanocytic dysplasia (nuclear pleomorphism and hyperchroma-tism). Fibrosis of
the papillary dermis and a lympho-cytic inflammatory response are also seen.
Complications
ÔÇó
Inflammation. Pain and swelling are common
butare not features of malignant transformation. They are caused by trauma,
bacterial folliculitis or a foreign body reaction to hair after shaving or
plucking.
ÔÇó
Depigmented halo (Fig.
18.19). So-called ÔÇśhalo naeviÔÇÖare uncommon but benign. There may be vitiligo
elsewhere. The naevus in the centre often involutes spontaneously before the
halo repigments.


Malignant change. This is extremely rare exceptin congenital melanocytic naevi, where the risk has been estimated at between 3 and 6% depending on their size (Fig. 18.20), and in the atypical naevi of melanoma-prone families. It should be considered if the following changes occur in a melanocytic naevus
ÔÇó
itch;
ÔÇó
enlargement;
ÔÇó
increased or decreased pigmentation;
ÔÇó
altered shape;
ÔÇó
altered contour;
ÔÇó
inflammation;
ÔÇó
ulceration; or
ÔÇó
bleeding.
If
changing lesions are examined carefully, remember-ing the ÔÇśABCDEÔÇÖ features of
malignant melanoma (Table 18.3), few malignant melanomas should be missed.
Treatment
Excision
is needed when:
1 a
naevus is unsightly;
2 malignancy
is suspected or is a known risk, e.g. in a large congenital melanocytic naevus;
or
3 a naevus is repeatedly inflamed or traumatized.
Epidermoid and pilar cysts
Often
incorrectly called ÔÇśsebaceous cystsÔÇÖ, these are common and can occur on the
scalp, face, behind the ears and on the trunk. They often have a central
punctum; when they rupture, or are squeezed, foul-smelling cheesy material
comes out. Histologically, the lining of a cyst resembles normal epidermis (an
epidermoid cyst) or the outer root sheath of the hair follicle (a pilar cyst).
Occasionally an adjacent foreign body reaction is noted. Treatment is by
excision, or by incision followed by expression of the contents and removal of
the cyst wall.
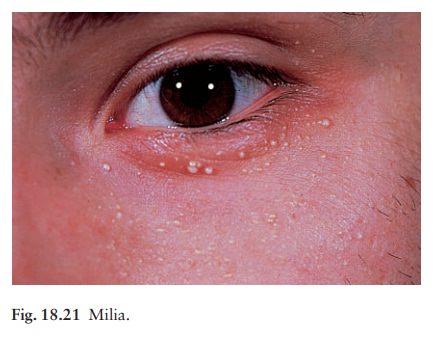
Milia
Milia
are small subepidermal keratin cysts (Fig. 18.21). They are common on the face
in all age groups and appear as tiny white millet seed-like papules of from 0.5
to 2 mm in diameter. They are occasionally seen at the site of a previous
subepidermal blister (e.g. in epidermolysis bullosa and porphyria cutanea
tarda). The contents of milia can be picked out with a sterile needle without
local anaesthesia.
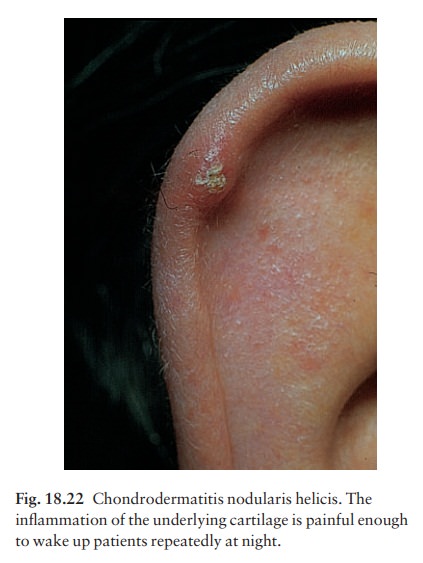
Chondrodermatitis nodularis helicis
(painful nodule of the ear, ear corn; Fig. 18.22)
This
terminological mouthful is, strictly, not a neo-plasm, but a chronic
inflammation. A painful nodule develops on the helix or antehelix of the ear,
most often in men. It looks like a small corn, is tender and prevents sleep if
that side of the head touches the pillow. Histologically, a thickened epidermis
overlies inflamed cartilage. Wedge resection under local anaesthetic is
effective if cryotherapy or intralesional triamcinolone injection fails.
Related Topics