Chapter: Medical Surgical Nursing: Assessment of Cardiovascular Function
Hemodynamic Monitoring - Diagnostic Evaluation of Cardiovascular Function
HEMODYNAMIC MONITORING
Critically
ill patients require continuous assessment of their cardio-vascular system to
diagnose and manage their complex medical conditions. This is most commonly
achieved by the use of direct pressure monitoring systems, often referred to as
hemodynamicmonitoring. Central
venous pressure (CVP), pulmonary arterypressure, and intra-arterial BP
monitoring are common forms of hemodynamic monitoring. Patients requiring
hemodynamic monitoring are cared for in specialty critical care units. Some
crit-ical care step-down units also admit stable patients with CVP or
intra-arterial BP monitoring. Noninvasive hemodynamic moni-toring is used in
some facilities.
To
perform invasive monitoring, specialized equipment is necessary and includes
the following:
·
A CVP, pulmonary artery, or arterial
catheter, which is in-troduced into the appropriate blood vessel or heart
chamber
·
A flush system composed of
intravenous solution (which may include heparin), tubing, stopcocks, and a
flush device, which provides for continuous and manual flushing of the system
·
A pressure bag placed around the
flush solution that is main-tained at 300 mm Hg of pressure; the pressurized
flush system delivers 3 to 5 mL of solution per hour through the catheter to
prevent clotting and backflow of blood into the pressure monitoring system
·
A transducer to convert the pressure
coming from the artery or heart chamber into an electrical signal
·
An amplifier or monitor, which
increases the size of the elec-trical signal for display on an oscilloscope
Central Venous Pressure Monitoring
The
CVP, the pressure in the vena cava or right atrium, is used to assess right
ventricular function and venous blood return to the right side of the heart.
The CVP can be continuously measured by connecting either a catheter positioned
in the vena cava or the proximal port of a pulmonary artery catheter to a
pressure mon-itoring system. The pulmonary artery catheter, described in
greater detail later, is used for critically ill patients. Patients in general
medical-surgical units who require CVP monitoring may have a single-lumen or
multilumen catheter placed into the superior vena cava. Intermittent
measurement of the CVP can then be ob-tained with the use of a water manometer.
Because
the pressures in the right atrium and right ventricle are equal at the end of
diastole (0 to 8 mm Hg), the CVP is also an indirect method of determining
right ventricular filling pres-sure (preload). This makes the CVP a useful
hemodynamic pa-rameter to observe when managing an unstable patient’s fluid
volume status. CVP monitoring is most valuable when pressures are monitored
over time and are correlated with the patient’s clin-ical status. A rising
pressure may be caused by hypervolemia or by a condition, such as HF, that
results in a decrease in myocardial contractility. Pulmonary artery monitoring
is preferred for the patient with HF. Decreased CVP indicates reduced right
ven-tricular preload, most often caused by hypovolemia. This diag-nosis can be
substantiated when a rapid intravenous infusion causes the CVP to rise. (CVP
monitoring is not clinically useful in a patient with HF in whom left
ventricular failure precedes right ventricular failure, because in these
patients an elevated CVP is a very late sign of HF.)Before insertion of a CVP
catheter, the site is prepared by shaving if necessary and by cleansing with an
antiseptic solution. A local anesthetic may be used. The physician threads a
single-lumen or multilumen catheter through the external jugular, ante-cubital,
or femoral vein into the vena cava just above or within the right atrium.
NURSING INTERVENTIONS
Once
the CVP catheter is inserted, it is secured and a dry, sterile dressing is
applied. Catheter placement is confirmed by a chest x-ray, and the site is
inspected daily for signs of infection. The dressing and pressure monitoring
system or water manometer are changed according to hospital policy. In general,
the dressing is to be kept dry and air occlusive. Dressing changes are
performed with the use of sterile technique. CVP catheters can be used for
infus-ing intravenous fluids, administering intravenous medications, and
drawing blood specimens in addition to monitoring pressure.
To measure the CVP, the transducer (when a pressure mon-itoring system is used) or the zero mark on the manometer (when a water manometer is used) must be placed at a standard reference point, called the phlebostatic axis (Fig. 26-12).
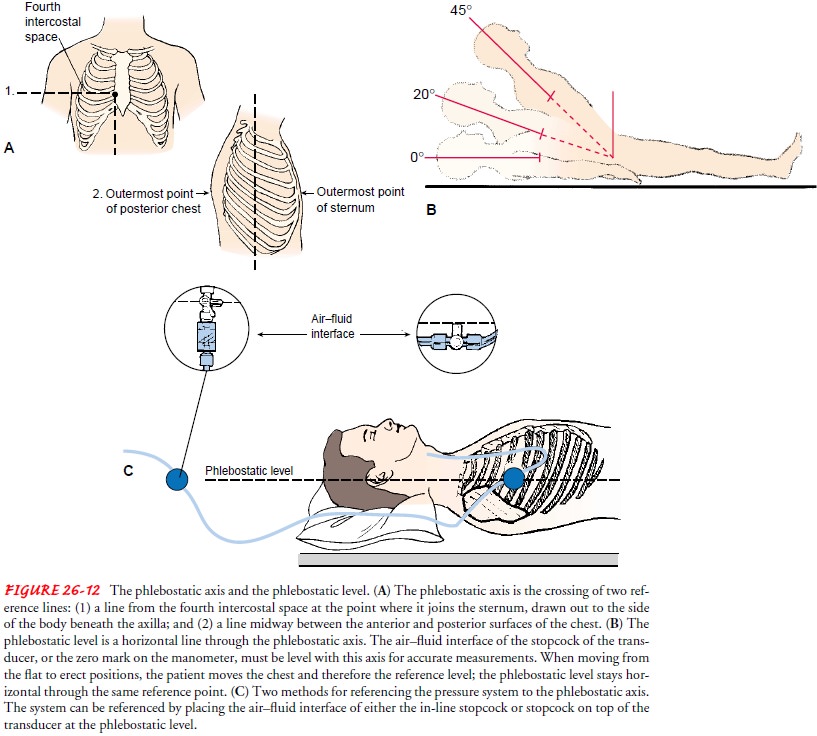
After lo-cating this position, the nurse may make an ink mark on the patient’s
chest to indicate the location. If the phlebostatic axis is used, CVP can be measured
correctly with the patient supine at any backrest position up to 45 degrees.
The range for a normal CVP is 0 to 8 mm Hg with a pressure monitoring system or
3 to 8 cm H2O with a water manometer system. The
most common complications of CVP monitoring are infection and air embolism.
Pulmonary Artery Pressure Monitoring
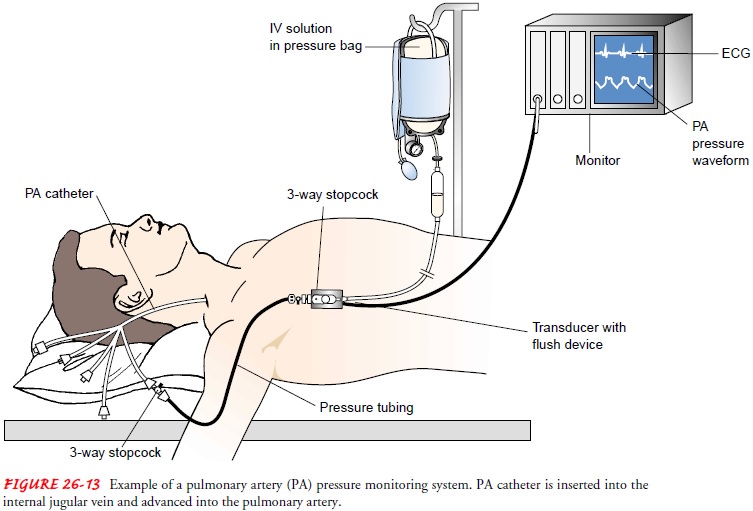
Pulmonary
artery pressure monitoring is an important tool used in critical care for
assessing left ventricular function, diagnosing the etiology of shock, and
evaluating the patient’s response to medical interventions (eg, fluid
administration, vasoactive med-ications). Pulmonary artery pressure monitoring
is achieved by using a pulmonary artery catheter and pressure monitoring
sys-tem. Catheters vary in their number of lumens and their types of
measurement (eg, cardiac output, oxygen saturation) or pacing capabilities. All
types require that a balloon-tipped, flow-directed catheter be inserted into a
large vein (usually the subclavian, jugu-lar, or femoral vein); the catheter is
then passed into the vena cava and right atrium. In the right atrium, the
balloon tip is inflated, and the catheter is carried rapidly by the flow of
blood through the tricuspid valve, into the right ventricle, through the
pulmonic valve, and into a branch of the pulmonary artery. When the cathe-ter
reaches a small pulmonary artery, the balloon is deflated and the catheter is
secured with sutures. Fluoroscopy may be used during insertion to visualize the
progression of the catheter through the heart chambers to the pulmonary artery.
This procedure can be performed in the operating room or cardiac
catheterization laboratory or at the bedside in the critical care unit. During
in-sertion of the pulmonary artery catheter, the bedside monitor is observed
for waveform and ECG changes as the catheter is moved through the heart
chambers on the right side and into the pul-monary artery.
After
the catheter is correctly positioned, the following pres-sures can be measured:
CVP or right atrial pressure, pulmonary artery systolic and diastolic
pressures, mean pulmonary artery pressure, and pulmonary artery wedge pressure
(Fig. 26-13). If a thermodilution catheter is used, the cardiac output can be
mea-sured and systemic vascular resistance and pulmonary vascular re-sistance
can be calculated.
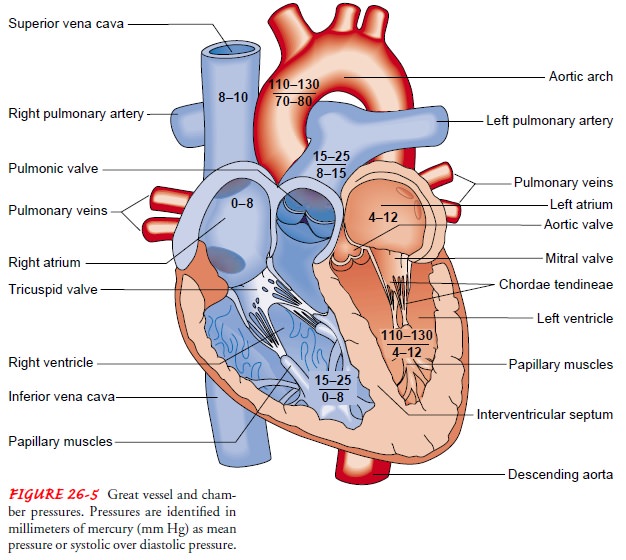
Normal
pulmonary artery pressure is 25/9 mm Hg, with a mean pressure of 15 mm Hg (see
Fig. 26-5 for normal ranges). When the balloon tip is inflated, usually with 1
mL of air, the catheter floats farther out into the pulmonary artery until it
becomes wedged. This is an occlusive maneuver that impedes blood flow through
that segment of the pulmonary artery. A pressure measurement, called pulmonary
artery wedge pressure, is taken within seconds after wedging of the pulmonary
artery catheter; then the balloon is immediately deflated and blood flow is
restored. The nurse who obtains the wedge reading ensures that the catheter has
returned to its normal position in the pulmonary artery by evaluating the
pul-monary artery pressure waveform. The pulmonary artery diastolic reading and
the wedge pressure reflect the pressure in the ventricle at end-diastole and
are particularly important to monitor in criti-cally ill patients, because they
are used to evaluate left ventricular filling pressures (preload). At
end-diastole, when the mitral valve is open, the wedge pressure is the same as
the pressure in the left atrium and the left ventricle, unless the patient has
mitral valve dis-ease or pulmonary hypertension. Pulmonary capillary wedge
pres-sure is a mean pressure and is normally 4.5 to 13 mm Hg. Critically ill
patients usually require higher left ventricular filling pressures to optimize
cardiac output. These patients may need to have their wedge pressure maintained
as high as 18 mm Hg.
NURSING INTERVENTIONS
Catheter
site care is essentially the same as for a CVP catheter. As in measuring CVP,
the transducer must be positioned at the phlebostatic axis to ensure accurate
readings (see Fig. 26-12). Complications of pulmonary artery pressure
monitoring include infection, pulmonary artery rupture, pulmonary
thromboem-bolism, pulmonary infarction, catheter kinking, dysrhythmias, and air
embolism.
Intra-arterial Blood Pressure Monitoring
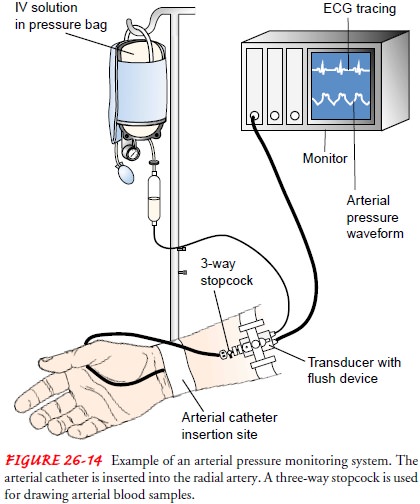
Intra-arterial
BP monitoring is used to obtain direct and contin-uous BP measurements in
critically ill patients who have severe hypertension or hypotension (Fig.
26-14). Arterial catheters are also useful when arterial blood gas measurements
and blood sam-ples need to be obtained frequently.
Once an arterial site is selected (radial, brachial, femoral, or dorsalis pedis), collateral circulation to the area must be con-firmed before the catheter is placed. This is a safety precaution to prevent compromised arterial perfusion to the area distal to the arterial catheter insertion site. If no collateral circulation exists and the cannulated artery became occluded, ischemia and infarc-tion of the area distal to that artery could occur. Collateral circu-lation to the hand can be checked by the Allen test to evaluate the radial and ulnar arteries or by an ultrasonic Doppler test for any of the arteries. With the Allen test, the nurse compresses the ra-dial and ulnar arteries simultaneously and asks the patient to make a fist, causing the hand to blanch. After the patient opens the fist, the nurse releases the pressure on the ulnar artery while maintaining pressure on the radial artery. The patient’s hand will turn pink if the ulnar artery is patent.
NURSING INTERVENTIONS
Site
preparation and care are the same as for CVP catheters. The catheter flush
solution is the same as for pulmonary artery catheters. A transducer is
attached, and pressures are measured in millimeters of mercury (mm Hg).
Complications include local obstruction with distal ischemia, external
hemorrhage, massive ecchymosis, dis-section, air embolism, blood loss, pain,
arteriospasm, and infection.
Related Topics