Chapter: Medical Surgical Nursing: Assessment of Cardiovascular Function
Angiography - Diagnostic Evaluation of Cardiovascular Function
ANGIOGRAPHY
Cardiac
catheterization is usually performed with angiography, a technique of injecting
a contrast agent into the vascular system to outline the heart and blood
vessels. When a particular heart chamber or blood vessel is singled out for
study, the procedure is known as selective angiography. Angiography makes use
of cine-angiograms, a series of rapidly changing films on an intensified
fluoroscopic screen that record the passage of the contrast agent through the
vascular site or sites. The recorded information al-lows for comparison of data
over time. Common sites for selec-tive angiography are the aorta, the coronary
arteries, and the right and left sides of the heart.
Aortography
An
aortogram is a form of angiography that outlines the lumen of the aorta and the
major arteries arising from it. In thoracic aor-tography, a contrast agent is
used to study the aortic arch and its major branches. The catheter may be
introduced into the aorta using the translumbar or retrograde brachial or
femoral artery approach.
Coronary Arteriography
In
coronary arteriography, the catheter is introduced into the right or left
brachial or femoral artery, then passed into the ascending aorta and
manipulated into the appropriate coronary artery. Coronary arteriography is
used to evaluate the degree of athero-sclerosis and to guide the selection of
treatment. It is also used to study suspected congenital anomalies of the
coronary arteries.
Right Heart Catheterization
Right
heart catheterization usually precedes left heart catheteri-zation. It involves
the passage of a catheter from an antecubital or femoral vein into the right
atrium, right ventricle, pulmonary artery, and pulmonary arterioles. Pressures
and oxygen satura-tions from each of these areas are obtained and recorded.
Although
right heart catheterization is considered a relatively safe procedure,
potential complications include cardiac dysrhyth-mias, venous spasm, infection
of the insertion site, cardiac perfo-ration, and, rarely, cardiac arrest.
Left Heart Catheterization
Left
heart catheterization is performed to evaluate the patency of the coronary
arteries and the function of the left ventricle and the mitral and aortic
valves. Potential complications include dys-rhythmias, MI, perforation of the
heart or great vessels, and sys-temic embolization. Left heart catheterization
is performed by retrograde catheterization of the left ventricle. In this
approach, the physician usually inserts the catheter into the right brachial
artery or a femoral artery and advances it into the aorta and left ventricle.
After
the procedure, the catheter is carefully withdrawn and arterial hemostasis is
achieved using manual pressure or other techniques previously described. If the
physician performed an arterial or venous cutdown, the site is sutured and a
sterile dress-ing is applied.
NURSING INTERVENTIONS
Nursing
responsibilities before cardiac catheterization include the following:
·
Instruct the patient to fast,
usually for 8 to 12 hours, before the procedure. If catheterization is to be
performed as an outpatient procedure, explain that a friend, family member, or
other responsible person must transport the patient home.
·
Prepare the patient for the expected
duration of the proce-dure; indicate that it will involve lying on a hard table
for less than 2 hours.
·
Reassure the patient that mild
sedatives or moderate seda-tion will be given intravenously.
·
Prepare the patient to experience
certain sensations during the catheterization. Knowing what to expect can help
the patient cope with the experience. Explain that an occasional pounding
sensation (palpitation) may be felt in the chest because of extrasystoles that
almost always occur, particu-larly when the catheter tip touches the myocardium.
The patient may be asked to cough and to breathe deeply, espe-cially after the
injection of contrast agent. Coughing may help to disrupt a dysrhythmia and to
clear the contrast agent from the arteries. Breathing deeply and holding the
breath helps to lower the diaphragm for better visualization of heart
structures. The injection of a contrast agent into either side of the heart may produce a flushed feeling throughout the
body and a sensation similar to the need to void, which sub-sides in 1 minute
or less.
·
Encourage the patient to express
fears and anxieties. Provide teaching and reassurance to reduce apprehension.
Nursing
responsibilities after cardiac catheterization may in-clude the following:
·
Observe the catheter access site for
bleeding or hematoma formation, and assess the peripheral pulses in the
affected extremity (dorsalis pedis and posterior tibial pulses in the lower
extremity, radial pulse in the upper extremity) every 15 minutes for 1 hour,
and then every 1 to 2 hours until the pulses are stable.
·
Evaluate temperature and color of
the affected extremity and any patient complaints of pain, numbness, or
tingling sensations to determine signs of arterial insufficiency. Re-port
changes promptly.
·
Monitor for dysrhythmias by
observing the cardiac moni-tor or by assessing the apical and peripheral pulses
for changes in rate and rhythm. A vasovagal reaction, consist-ing of
bradycardia, hypotension, and nausea, can be pre-cipitated by a distended
bladder or by discomfort during removal of the arterial catheter, especially if
a femoral site has been used. Prompt intervention is critical; this in-cludes
raising the feet and legs above the head, adminis-tering intravenous fluids,
and administering intravenous atropine.
·
Inform the patient that if the procedure
is performed per-cutaneously through the femoral artery (and without the use of
devices such as VasoSeal, Perclose, or Angio-Seal), the patient will remain on
bed rest for 2 to 6 hours with the affected leg straight and the head elevated
to 30 degrees (Logemann et al., 1999). For comfort, the patient may be turned
from side to side with the affected extremity straight. If the cardiologist
uses deployed devices, check local nurs-ing care standards, but anticipate that
the patient will have less restrictions on elevation of the head of the bed and
will be allowed to ambulate in 2 hours or less (Baim et al., 2000). Analgesic
medication is administered as prescribed for discomfort.
·
Instruct the patient to report chest
pain and bleeding or sudden discomfort from the catheter insertion sites
immediately.
·
Encourage fluids to increase urinary
output and flush out the dye.
·
Ensure safety by instructing the
patient to ask for help when getting out of bed the first time after the
procedure, because orthostatic hypotension may occur and the patient may feel
dizzy and lightheaded.
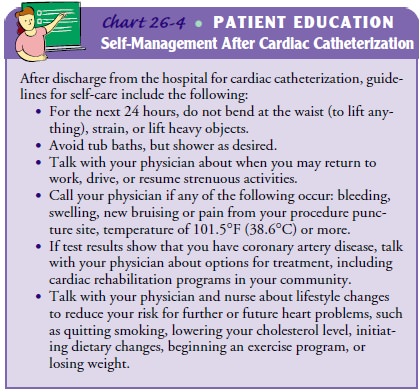
For
patients being discharged from the hospital on the same day as the procedure,
additional instructions are provided. They appear in Chart 26-4.
Related Topics