Chapter: Medical Surgical Nursing: Assessment of Cardiovascular Function
Anatomy of the Heart
ANATOMY OF THE HEART
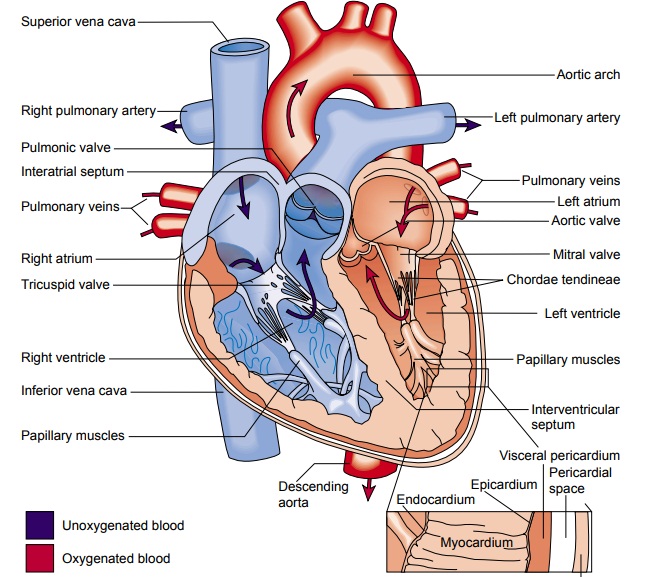
The
heart is composed of three layers (Fig. 26-1). The inner layer, or endocardium,
consists of endothelial tissue and lines the inside of the heart and valves.
The middle layer, or myocardium, is made up of muscle fibers and is responsible
for the pumping action. The exterior layer of the heart is called the epicardium.
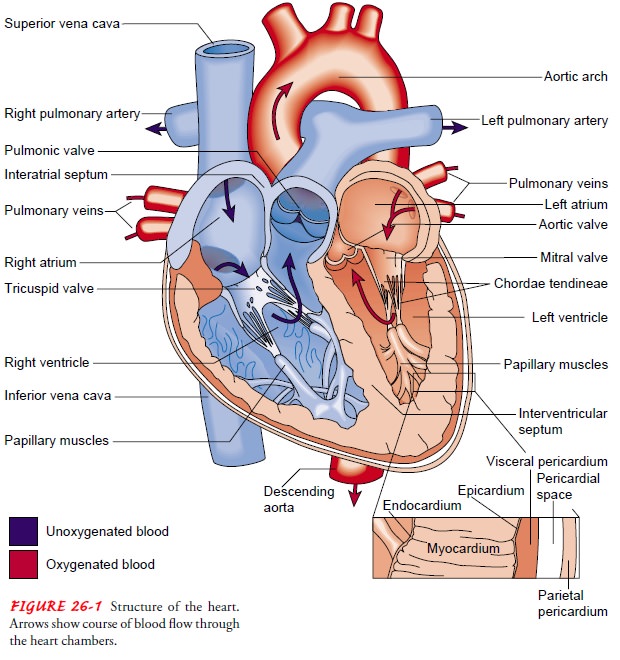
The
heart is encased in a thin, fibrous sac called the pericardium, which is
composed of two layers. Adhering to the epicardium is the visceral pericardium.
Enveloping the visceral pericardium is the parietal pericardium, a tough
fibrous tissue that attaches to the great vessels, diaphragm, sternum, and
vertebral column and sup-ports the heart in the mediastinum. The space between
these two layers (pericardial space) is filled with about 30 mL of fluid, which
lubricates the surface of the heart and reduces friction during systole.
Heart Chambers
The four chambers of the heart constitute the right- and left-sided pumping systems. The right side of the heart, made up of the right atrium and right ventricle, distributes venous blood (deoxygenated blood) to the lungs via the pulmonary artery (pulmonary circulation) for oxygenation. The right atrium re-ceives blood returning from the superior vena cava (head, neck, and upper extremities), inferior vena cava (trunk and lower ex-tremities), and coronary sinus (coronary circulation).
The left side
of the heart, composed of the left atrium and left ventricle, distributes
oxygenated blood to the remainder of the body via the aorta (systemic
circulation). The left atrium receives oxy-genated blood from the pulmonary
circulation via the pulmonary veins. The relationships of the four heart
chambers are shown in Figure 26-1.
The
varying thicknesses of the atrial and ventricular walls re-late to the workload
required by each chamber. The atria are thin-walled because blood returning to
these chambers gener-ates low pressures. In contrast, the ventricular walls are
thicker because they generate greater pressures during systole. The right
ventricle contracts against low pulmonary vascular pres-sure and has thinner
walls than the left ventricle. The left ven-tricle, with walls two-and-a-half
times more muscular than those of the right ventricle, contracts against high
systemic pressure.
Because
the heart lies in a rotated position within the chest cavity, the right
ventricle lies anteriorly (just beneath the ster-num) and the left ventricle is
situated posteriorly. The left ven-tricle is responsible for the apex beat or
the point of maximum impulse (PMI), which is normally palpable in the left
midclavic-ular line of the chest wall at the fifth intercostal space.
Heart Valves
The
four valves in the heart permit blood to flow in only one di-rection. The
valves, which are composed of thin leaflets of fibrous tissue, open and close
in response to the movement of blood and pressure changes within the chambers.
There are two types of valves: atrioventricular and semilunar.
ATRIOVENTRICULAR VALVES
The
valves that separate the atria from the ventricles are termed atrioventricular
valves. The tricuspid valve, so named because it is composed of three cusps or
leaflets, separates the right atrium from the right ventricle. The mitral, or
bicuspid (two cusps) valve, lies between the left atrium and the left ventricle
(see Fig. 26-1).
Normally,
when the ventricles contract, ventricular pressure rises, closing the
atrioventricular valve leaflets. Two additional structures, the papillary
muscles and the chordae tendineae, maintain valve closure. The papillary
muscles, located on the sides of the ventricular walls, are connected to the
valve leaflets by thin fibrous bands called chordae tendineae. During systole,
contrac-tion of the papillary muscles causes the chordae tendineae to be-come
taut, keeping the valve leaflets approximated and closed.
SEMILUNAR VALVES
The
two semilunar valves are composed of three half-moon-like leaflets. The valve
between the right ventricle and the pulmonary artery is called the pulmonic
valve; the valve between the left ven-tricle and the aorta is called the aortic
valve.
Coronary Arteries
The
left and right coronary arteries and their branches (Fig. 26-2) supply arterial
blood to the heart. These arteries originate from the aorta just above the
aortic valve leaflets. The heart has large metabolic requirements, extracting
approximately 70% to 80% of the oxygen delivered (other organs consume, on
average, 25%). Unlike other arteries, the coronary arteries are perfused during
diastole. An increase in heart rate shortens diastole and can de-crease myocardial
perfusion. Patients, particularly those with coronary artery disease (CAD), can
develop myocardial ischemia
(inadequate oxygen supply) when the heart rate accelerates.

The
left coronary artery has three branches. The artery from the point of origin to
the first major branch is called the left main coronary artery. Two
bifurcations arise off the left main coronary artery. These are the left
anterior descending artery, which courses down the anterior wall of the heart,
and the circumflex artery, which circles around to the lateral left wall of the
heart.
The
right side of the heart is supplied by the right coronary artery, which
progresses around to the bottom or inferior wall of the heart. The posterior
wall of the heart receives its blood sup-ply by an additional branch from the
right coronary artery called the posterior descending artery.
Superficial to the coronary arteries are the coronary veins. Venous blood from these veins returns to the heart primarily through the coronary sinus, which is located posteriorly in the right atrium.
Cardiac Muscle
The
myocardium is composed of specialized muscle tissue. Micro-scopically,
myocardial muscle resembles striated (skeletal) mus-cle, which is under
conscious control. Functionally, however, myocardial muscle resembles smooth
muscle because its contrac-tion is involuntary. The myocardial muscle fibers
are arranged in an interconnected manner (called a syncytium) that allows for
co-ordinated myocardial contraction and relaxation. The sequential pattern of
contraction and relaxation of individual muscle fibers ensures the rhythmic
behavior of the myocardium as a whole and enables it to function as an
effective pump.
Related Topics