Chapter: Modern Medical Toxicology: Substance Abuse: Substances of Dependence and Abuse
Hallucinogens (Psychedelics, Psychotomimetics) - Substances of Dependence and Abuse
Hallucinogens (Psychedelics, Psychotomimetics)
Hallucinogens are substances that
induce changes in thought, perception, and mood, without causing major
disturbances in the autonomic nervous system. Perceptual alterations can take
the form of illusions, synaesthesias, or hallucinations. An illusion is the result of
misinterpretation of an actual experi-ence, while synaesthesias are sensory misperceptions (e.g. hearing colour or
seeing sounds). Both require external stimuli for their institution. Hallucinations differ from them in this
important respect, since they are perceptual alterations without any external
stimulation whatsoever. Hallucinations may be visual, auditory, olfactory,
gustatory, or tactile in nature. Most hallucinogens induce visual or auditory
hallucinations; a few cause tactile or olfactory manifestations. While a number
of therapeutic drugs can cause hallucinations in overdose, they are not
classified as hallucinogens. A true hallucinogen is a drug that induces
hallucinations in small doses (sometimes, as in the case of LSD, in microgram
doses). Most genuine hallucinogens cause vivid visual hallucinations, while the
other types of hallucinations are relatively uncommon. Table 34.15 lists common hallucinogens, some of which will be
discussed in detail in this section, while the others have been discussed in
appropriate sections elsewhere.
1. Lysergic Acid Diethylamide
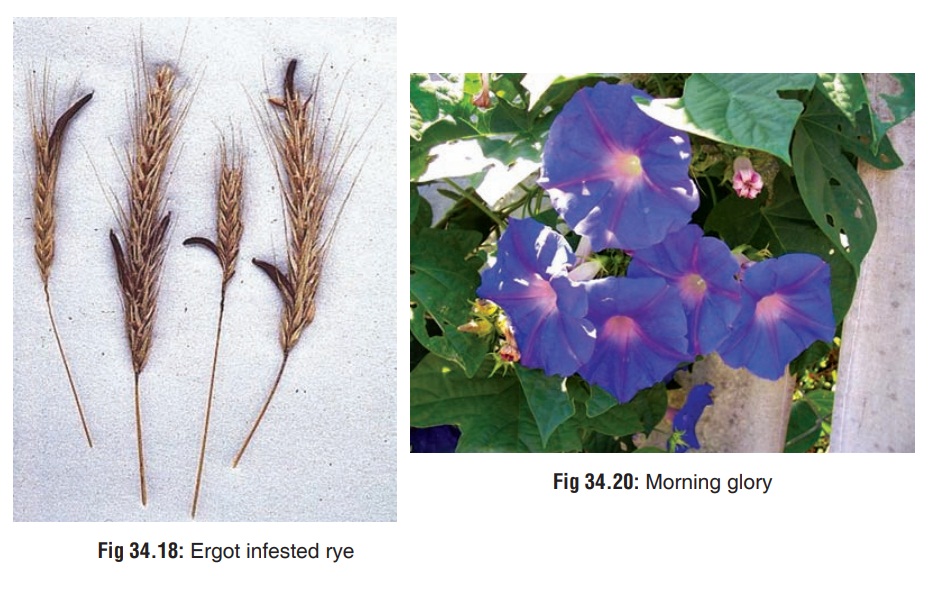
· Lysergic acid diethylamide (LSD) is the synthetic diethylamide derivative of ergot alkaloids, and was originally synthesised exclusively from these alkaloids produced by the fungus Claviceps purpurea , which is a contaminant of rye and certainother grains ( Fig 34.18).

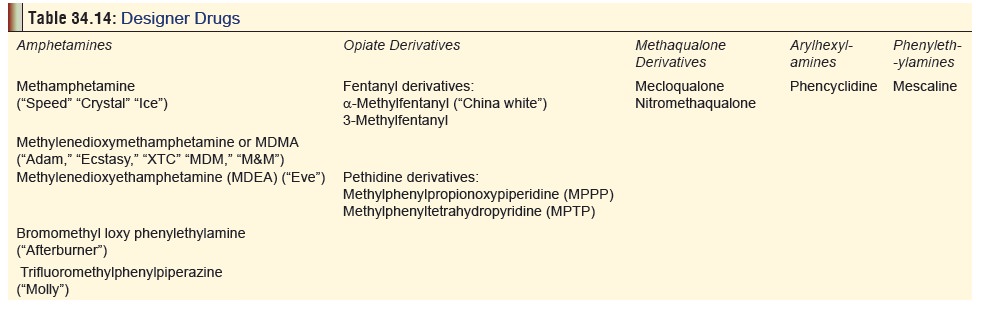
Today, most LSD is synthesised entirely in the laboratory, and typically sold to addicts as liquid-impregnated blotting paper (Fig 34.19) or sugar cubes, tiny tablets (“microdots”), gelatin squares (“window panes”), liquid, or powder. LSD is said to be the most powerful of all hallucinogens, and is active in doses of 50 to 100 mg. It occurs as a water-soluble, colourless, tasteless and odourless powder.
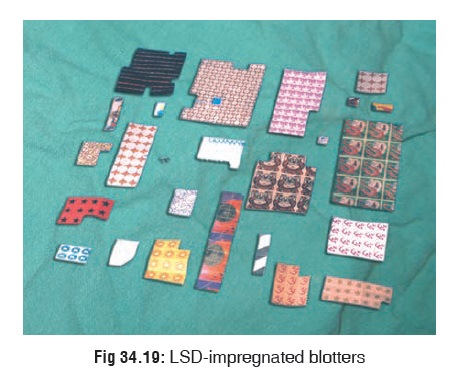
Drugs related to LSD (lysergamides)
also occur naturally in plants such as “Morning glory” (Rivea corymbosa) (Fig 34.20)
and “Hawaiian baby woodrose” (Ipomoea
violacea). Seeds of morning glory contain lysergic acid hydroxyethylamide,
which is 1/10th as powerful as LSD. At least 200 to 300 seeds have to be
pulverised—intact seed coat resists digestion—and ingested, for inducing
hallucinogenic effects.

Mode of Intake
The LSD is almost always ingested.
Other less common routes of intake include intranasal, sublingual, smoking,
conjuctival instillation, and very rarely injection.
Mode of Action
The LSD is structurally related to serotonin (5-hydroxy-tryptamine) and is an agonist at the 5 -HT1 receptor. Serotonin modulates many psychological and physiological processes including mood, personality, affect, appetite, sexual desire, motor function, temperature regulation, pain perception, and sleep induction. LSD inhibits central raphe neurons of brainstem through stimulation of 5-HT1A receptors, which are coupled to adenylcyclase. LSD is also an agonist at 5-HT2A, 2C receptors, which are not located presynaptically on seroton-ergic cell bodies but on certain subpopulations of neurons in postsynaptic regions. The majority of 5 -HT2 receptors in the brain are located in the cerebral cortex. Animal experiments have shown that LSD is anatomically distributed maximally in the visual and auditory cortex, and the limbic cortex (besides the pituitary, pineal, and hypothalamic areas), which parallels the finding of high concentration of 5-HT2 receptors in human cerebral cortex. Recent studies also suggest that ctivation of D1 (dopamine) receptors may contribute to the neurochemical effects of LSD.
Toxicokinetics
The
LSD has a half-life of 2.5 hours, while the duration of effects lasts for up to
8 hours. But psychotropic effects can occur for several days, and urine-screen
is usually positive for 100 to 120 hours. The route of metabolism is hepatic
hydroxylation. The usual dose of abuse is 100 to 300 mcg. Doses over 0.2 mg/kg
are potentially lethal.
Clinical (Toxic) Features
1. Acute Poisoning:
a.Physical
––Mydriasis,
hippus.
––Vertigo.
––Tachycardia,
hypertension.
––Sweating,
piloerection.
––Hyperthermia.
––Tachypnoea.
––Muscle
weakness, ataxia.
––Hyperactivity.
––Coma.
b.Psychological
––Euphoria
or dysphoria.
––Vivid
hallucinations, synaesthesias.
––Bizarre
perceptual changes: People’s faces and body parts appear distorted, objects
undu- late, sounds may be magnified and distorted, colours seem brighter with
halos around objects. Occasionally there is depersonalisation, and the
hallucinating person may feel as if he is observing an event instead of being
involved in it.
Chronic Poisoning:
·
Prolonged psychotic reactions which
are mainly schizo-phrenic in nature.
·
Severe depression.
·
Flashback
phenomena: The person relives the LSDexperience periodically in the
absence of drug intake for months or years.
·
Post-hallucinogen perception
disorder: A
persistentperceptual disorder often described by the person as if he is
residing in a bubble under water in a “purple haze”, with trailing of lights
and images. Associated anxiety, panic, and depression are common. The following
unusual phenomena have also been reported:
–– Pareidolias: images of faces on floor
and walls, floating faces hovering in space.
–– Aeropsia: visualisation of air in the
form of numerous vibrating pinpoint-sized dots (“mole-cules”).
Diagnosis
â– â– Radioimmunoassay of serum or urine (limit of detection 0.1ng/ml).
â– â– HPTLC (high performance
thin layer chromatography) candetect LSD in urine in concentrations less than 1
mcg/litre.
·
HPLC (high pressure/performance liquid chromatography) of
serum and urine.
·
GC-MS (gas chromatography–mass spectrometry) can confirm
positive LSD urine levels to a lower limit of 5 pg/ml.
Treatment
Avoid
gut decontamination as LSD is ingested in micro-quantities and rapidly
absorbed, rendering decontamina- tion procedures totally redundant.
·
Do not use restraints in agitated
patients; it will only exac- erbate the condition.
·
Because of the short half-life and
few serious medical reactions, elimination enhancement procedures such as
haemodialysis, haemoperfusion, etc. are not warranted.
·
Treat acute panic attacks with quiet
environment, reas- surance, supportive care, and administration of diazepam
(5–10 mg IV) or haloperidol (in severe cases).
·
Treat acute psychotic reactions with
cautious administration of neuroleptics such as haloperidol. Avoid
phenothiazines which can cause hypotension, sedation, extrapyramidal reactions,
lowered seizure threshold, and potentiation of anticholinergic effects.
·
Treat flashbacks with psychotherapy,
anti-anxiety agents, and neuroleptics.
·
Treat post-hallucinogen perception
disorder with long- lasting benzodiazepines such as clonazepam, and to a lesser
extent anticonvulsants such as valproic acid and carbamazepine. This approach
must be combined with behavioural therapy. The patient must be instructed not
to consume alcohol, cannabis, caffeine, and other drugs which can intensify the
disorder.
Phencyclidine
Source
Phencyclidine
(PCP), a phenylcyclohexylamine compound, is easily synthesised from piperazine,
cyclohexanone, and potas-sium cyanide. It is commonly referred to by addicts as
“angel dust” or “PCP”.
Phencyclidine
was developed in the 1950s as a potential general anaesthetic by Parke-Davis
under the brand name Sernyl. It was termed a “dissociative anaesthetic” because
unlike conventional anaesthetics which induced a state of relaxed sleep, PCP
induced a state of catatonia with flat facies, open mouth, fixed staring, rigid
posturing, and waxy flexibility. Patients seemed dissociated from the
environment without classical coma. However, a significant proportion of
patients showed severe adverse reactions during emergence, including agitation
and hallucinations. Some suffered from psychosis for up to 10 days. PCP was
therefore quickly withdrawn. Today, ketamine a less potent PCP derivative is
quite popular as an anaesthetic.
Mode of Intake
Phencyclidine (PCP) is abused by
smoking, insufflation, ingestion, or rarely IV injection. It is commonly sold
on the street as tablets (about 5 mg), capsules, powder, aqueous or alcoholic
solution, or as “rock salt” crystal. It is often mixed with parsley, mint,
oregano,![]() or marijuana. Sometimes “crack” is
dipped in PCP and smoked (“tragic magic”), or cannabis is dipped in PCP (“love
boat”).
or marijuana. Sometimes “crack” is
dipped in PCP and smoked (“tragic magic”), or cannabis is dipped in PCP (“love
boat”).
Mode of Action
Phencyclidine antagonises the action
of glutamate at the NMDA (N-methyl-d-aspartate) receptor. It binds within the
ion channel (PCP binding site) to block Ca++ influx which results from
glutamate binding. Unlike the other types of glutamate receptor channels, NMDA
channels are permeable to both Ca++ and Na+. Following NMDA receptor
activation, NMDA-mediated Ca++ flux may lead to stimulation of
calmodulin-dependant kinases with activation of postsynaptic second-messenger
pathways. Opening the NMDA channel facilitates access of PCP to its receptor,
accelerating the rate at which PCP-induced blockade of NMDA receptor-mediated neurotransmission
takes place.
At doses much higher than at which
it exerts its unique behav-ioural effects by blocking NMDA receptor-mediated
neurotrans-mission, PCP also blocks presynaptic monoamine reuptake, thus
directly increasing synaptic levels of dopamine and noradrenaline. At even
higher doses, PCP blocks neuronal Na+ and K+ channels, as well as muscarinic
cholinergic receptors. This may explain the occurrence of convulsions in PCP
overdose.
Toxicokinetics
The
volume of distribution of phencyclidine is 6.2 L/kg. Plasma protein binding is
about 65%. Since it is highly lipid soluble, it accumulates in brain and
adipose tissue. Metabolism of the latter causes release of PCP which
contributes to the recurrence of symptoms. PCP can be detected in urine up to
20 to 30 days (usually 2 weeks).
Clinical (Toxic) Features
CNS:
·
Level of consciouness ranges from
fully alert to coma-tose. The coma is usually preceded as well as followed
(upon recovery) by agitation and psychosis.
·
Confusion, disorientation, amnesia.
·
Catatonia with unusual posturing,
mutism, and staring.
·
Myoclonic and dystonic movements,
choreoathetoid, opisthotonus, torticollis.
·
Acute toxic psychosis with bizarre
behaviour, agitation, and violence.
·
Cholinergic (sweating, miosis,
salivation, bronchos-pasm), or anticholingeric (mydriasis, tachycardia, urinary
retention) signs may be present.
·
Hallucinations (auditory and
visual).
·
Convulsions.
·
Hyperthermia.
Eye:
·
Blank stare
·
Dysconjugate gaze
·
Nystagmus (horizontal, vertical, or
rotatory)
·
Blurred vision
·
Miosis (occasionally mydriasis).
CVS:
·
Sinus tachycardia
·
Hypertension.
GIT:
·
Vomiting.
RS:
·
Tachypnoea.
Renal:
·
Myoglobinuria
·
Acute renal failure.
Usual Fatal Dose
â– â– Approximately 100 mg
or more.
â– â– Lethal
blood level: 0.1 mg/100 ml.
Diagnosis
Serum
PCP levels usually do not correlate well with clinical picture. Therefore, a
qualitative test is adequate in most cases.
Laboratory
findings:
·
Leukocytosis
·
Hypoglycaemia
·
Hyperkalaemia
·
Elevated muscle enzymes
·
EEG: Diffuse slowing with theta and
delta waves.
Treatment
The
need for syrup of ipecac or gastric lavage should be assessed carefully. Often
such measures may exacerbate agitation and violence.
·
Activated charcoal is highly
beneficial and can be admin-istered at a dose of 1 gm/kg every 4 hours for
several doses.
·
A single dose of a suitable
cathartic such as sorbitol can be given (unless there are specific
contraindications).
·
Some authors recommend urinary
acidification to enhance excretion of PCP (which is a weak base). But only 10%
of the drug is excreted in the urine, while the remaining 90% is metabolised in
the liver. Hence the practical utility of urinary acidification is negligible.
·
Haemodialysis and haemoperfusion are
not beneficial.
·
As of now there is no antidote for
PCP, though efforts are on to develop PCP-specific antigen binding fragmens
(Fab) which can prove to be very useful.
·
Agitated patients should be
restrained, at first physi-cally and later pharmaceutically. Hypoglycaemia, if
present, must be treated with 50% dextrose in water.
·
Subsequently if agitation persists,
administer titrated doses of diazepam 5 to 10 mg IV, every 10 minutes, until
the patient is calmed. Phenothiazines should be avoided since they can worsen
dystonic reactions, hypotension, hyperthermia, and lower the seizure threshold.
·
Specific antihypertensive therapy
should be instituted in patients with very high blood pressure.
·
Myoglobinuria should be treated with
IV infusion of 1 litre of 5% dextrose in water (containing 25 gm of mannitol
and 100 mEq of sodium bicarbonate), at a rate of 250 ml/hour. Monitor the
patient for hypokalaemia. If renal failure has occurred, haemodialysis should
be undertaken.
Forensic Issues (Hallucinogens)
Hallucinogen abuse has been
traditionally a Western phenom-enon, and drugs of abuse such as LSD and
phencyclidine have always been popular only in countries such as the USA, UK,
Australia, and parts of Europe. The popularity of such drugs has been fuelled
by their, glamourous representation in films and rock music. The 1960s saw an
explosion of hallucinogen use almost in the form of an epidemic, and though it
declined steeply in the 1970s and 1980s, there has been an alarming resurgence
over the last decade.
The
dangers of hallucinogen use do not have as much to do with acute toxicity, as
with long-term psychological damage. The inevitable fallout is violent crime
manifesting as assaulta-tive behaviour, homicides, and suicides. Several
horrific crimes have been committed by drug-crazed individuals acting out their
bizarre fantasies.
Related Topics