Chapter: Modern Medical Toxicology: Substance Abuse: Substances of Dependence and Abuse
Amphetamines - Substances of Dependence and Abuse
Amphetamines
·
Amphetamine belongs to the phenylethylamine family with a
methyl group substitution in the alpha carbon position.
Numerous substitutions of the
phenylethylamine structure are possible, resulting in several amphetamine-like
compounds. These compounds have now collectively come to be known as
“amphetamines”, and include amphetamine phosphate, amphetamine sulfate,
benzphetamine, chlorphentermine, clobenzorex hydrochloride, dextroamphetamine,
diethylpro-pion, mazindol, methamphetamine, 4-methylthioamphetamine,
methylphenidate, pemoline, phendimetrazine, phenmetrazine, and phentermine.
·
In the late 1980s, a pure preparation of methamphetamine
hydrochloride made its appearance for the first time in Hawaii where it was
referred to as “batu”. It quickly made its way across to the United Kingdom,
Australia, Western Europe, and USA, where it became popular by the slang name
“ice” (or “glass”) (Fig 34.15).
While ice is produced by the ephedrine reduction method and is very pure,
occurring as large translucent crystals, a variant produced by an oil-based
method is called “crystal” (or “crank”), and is a white to yellow crystal
product.
·
Methamphetamine abuse began in the 1950s and reached a peak
in the 1970s. It used to be referred to as “speed” or “go”. The newer avatars
“ice” and “crystal” are virtually the same in their pharmacological and toxic
effects. Other slang names include “chalk” and “meth”. Methamphetamine powder
can be inhaled, smoked, ingested, or injected. Ice and crystal are almost
always smoked.
Uses
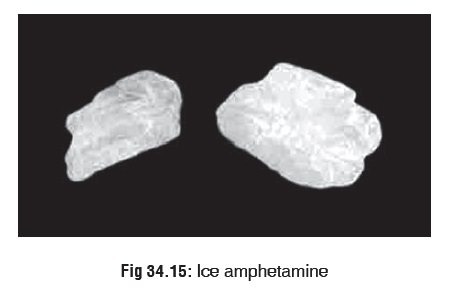
Some amphetamines have therapeutic
uses and are still avail-able as prescription drugs in Western countries (Table 34.13).
They are not available in India.
Mode of Action
The major mechanism of action of
amphetamines involves the release of monoamines from storage sites in axon
terminals, which leads to increased monoamine concentration in the synaptic
cleft. The release of dopamine in the nucleus accum-bens and related structures
is responsible for the reinforcing and mood elevating effects of amphetamines.
Cardiovascular effects result from the stimulation of release of noradrenaline.
The dopamine released into the
cytoplasm of neurons undergoes oxidation, resulting in the production of
several toxic chemicals (oxygen radicals, peroxides and hydroxyquinones).
Methylphenidate has a different
mechanism of action. Like cocaine, it produces CNS action by blocking the
dopa-mine transporters responsible for the reuptake of dopamine from synapses
following its release. The relatively low abuse potential of orally
administered methylphenidate is due to slow occupation of dopamine transporters
in the brain. Also, unlike cocaine, methylphenidate occupies the transporter
sites for a much longer time.
Amphetamines also have weak
monoamine oxidase inhib-iting property, but the significance of this is not
clear.
The most prominent effects of amphetamines are the catecholamine effects as a result of stimulation of peripheral alpha- and beta-adrenergic receptors. Enhanced concentration of noradrenaline at the locus coeruleus is responsible for the anorexic and stimulating effects, as well as to some extent, for the motor-stimulating effects.
The increase in central dopamine (especially in the
neostriatum) provokes stereotypical behaviour and some motor effects. The
activity of dopamine in the neostriatum appears to be linked to glutamate
release and inhibition of GABA-ergic efferent neurons, contributing
significantly to the stereotypical behaviour, locomotor effects, and
neurotoxicity of amphetamines. The effects of serotonin and dopamine at the
mesolimbic system alter perception and induce psychotic manifestations.
Toxicokinetics
In general, peak plasma levels are
seen in about 30 minutes after intravenous or intramuscular injection, and
about 2 to 3 hours after oral amphetamine ingestion. Amphetamines are
extensively metabolised in the liver, but much of what is ingested is excreted
unchanged in the urine. They differ from catecholamines in that they lack the
catechol structure and therefore cannot be metabolised by catechol-o-methyl
transferase (COMT), which permits oral efficacy. In general, amphetamines are
lipophilic, and hence can cross the blood-brain barrier easily.
Protein binding is 16% for
amphetamine, 15% for meth-ylphenidate, and less than 40% for pemoline.
Amphetamines have large volumes of distribution, varying from 3 to 5 L/kg for
amphetamine, to 11 to 33 L/kg for methylphenidate. The half-life ranges from 7
to 30 hours. The half-life is considerably shortened when the urine is acidic.
The excretion of unchanged amphetamine is dependant on pH, and at urine pH less
than 6.6, a range of 67 to 73% of unchanged drug is excreted in the urine. At
urine pH greater than 6.7, the percent excreted unchanged in the urine is
reported to be 17 to 43%.
Clinical Features
Acute Poisoning:
a.
CNS
––
Euphoria
––
Agitation
––
Headache
–– Paranoia
–– Anorexia
–– Hyperthermia: can be severe, and
may result from hypothalamic dysfunction, metabolic and muscle hyperactivity,
or prolonged seizures.
––
Hyperreflexia
––
Choreoathetoid movements
–– Convulsions: Seizures are
associated with a high mortality rate
–– Intracerebral haemorrhage: Abuse
of amphetamine and related drugs can increase the risk for cerebro-vascular
incidents in young adults
–– Coma: If it occurs, is associated
with a high mortality rate.
b. CVS
–– Tachycardia: Tachycardia is
common, however, reflex bradycardia secondary to hypertension can occur.
––
Hypertension: Hypertension is common following amphetamine use and may
result in end organ damage. Pulmonary hypertension has been associ-ated with
methamphetamine use. Hypotension and cardiovascular collapse may result from
severe toxicity, and is associated with a high fatality rate.
–– Arrhythmias.
–– Vasospasm.
–– Myocardial ischaemia: Infarction
can occur (videinfra).
–– Cardiomyopathy: Acute and chronic
cardiomyo-pathy can result from hypertension, necrosis, or ischaemia.
c. Sympathetic Effects:
–– Mydriasis
–– Sweating
–– Tremor
–– Tachypnoea
–– Nausea.
d. Other Effects:
––
Muscle rigidity
––
Pulmonary oedema
–– Ischaemic colitis: More common in
chronic poisoning (vide infra).
–– Rhabdomyolysis: Develops in
patients with severe agitation, muscular hyperactivity, hyperthermia, or
seizures.
-- Metabolic acidosis: This occurs
with severe poisoning, and has even been reported after smoking crystal
methamphetamine.
e. Complications:
–– Psychosis with visual and tactile
hallucinations. –– Cerebral infarction
––
Myocardial infarction
–– Aortic dissection: Several cases
of fatal aortic dissection associated with chronic amphetamine use have been
reported.
––
Ventricular fibrillation
–– Acute renal failure: Renal
failure may develop secondary to dehydration or rhabdomyolysis in patients with
severe amphetamine poisoning.
Death due to amphetamine toxicity
most commonly results from arrhythmias, hyperthermia, or intracerebral
haemorrhage. In cases of survival, symptoms gradually resolve as the drug is
excreted over a period of 24 to 48 hours.
Chronic Poisoning: Amphetamines can be taken orally,by
injection, by absorption through nasal and buccal membranes; or by heating,
inhalation of the vapours, and absorption through the pulmonary alveoli.
Inhaled ampheta-mine is almost immediately absorbed with a rapid onset of
effects. Unlike cocaine, amphetamines can be vapourised without much
destruction of the molecule, thus obviating the need for preparing a free-base
form for smoking. As with opiates, the rapid onset of effects from amphetamine
injection or inhalation produces an intensely pleasurable sensation referred to
as “rush”.
Chronic users of ampheta-mines tend
to fall into one or the other of the following categories:
Intermittent low-dose misuse: Some individuals(students studying
for exams, military personnel on extended exercises, athletes, truck drivers on
night trips, etc.), consume amphetamines periodically to overcome fatigue,
prolong wakefulness, or elevate mood. They usually do not develop dependence.
Sustained oral misuse: Some individuals who havebeen
prescribed amphetamines for legitimate purposes, as well as some others who
have been using these drugs illicitly may continue to ingest them in relatively
large daily doses of 40 to 100 mg or more (as tolerance develops). Attempts to
reduce the dose result in depres-sion and lethargy.
High-dose IV abuse: Individuals who relish theeuphoria
induced by amphetamines quickly progress to IV injections in order to enhance
the “rush” or “flash”.
These individuals (“speed freaks”)
classically manifest the symptomatology of chronic amphetamine toxicity. They
are also prone to “speed binges” wherein there are repeated cycles of action
and reaction phases. The former is due to intake of the drug resulting in a
“high”, while the latter is due to stoppage, and is associated with acute
hunger followed by intense depression or “crash”. This provokes him to go on
the action phase again, and the cycle continues until collapse or financial
ruin.![]()
Inhalant abuse: WhenBenzedrineinhalers were avail-able, a significant proportion of
users became addicted.
The 1959 FDA ban on these inhalers
led to the introduc-tion of Benedrex
inhalers (containing propylhexedrine, methanol, and aromatic compounds). By the
1970s, addiction to these inhalers became a major problem. Today, all
amphetamine analogues have been banned from inhalers. However, there are
indications that the apparently innocuous Vicks
Nasal Inhaler (containing l-desoxyephedrine,
which is actually l-methampheta-mine)*
may have high abuse potential.
Manifestations of heavy chronic amphetamine use: –– Hyperactivity, hyperexcitability.
––
Anorexia, loss of weight, emaciation: Weight loss is one of the most
characteristic findings with chronic use of amphetamine or its derivatives, and
is said to be the most striking effect in chronic “ice” smoking.
–– Vomiting and diarhoea are common.
Ischaemic colitis may occur.
–– Stereotyped behaviour (skin
picking, pacing, inter-minable chattering).
––
Dyskinesias: bruxism, tics.
–– Paranoid psychosis, unpredictable
violence: In one study, the most common symptoms in patients with
methamphetamine-induced psychosis were auditory and visual hallucinations,
persecutory delusions, and delusions of reference. They also demonstrated a
high tendency for major depres-sive disorder, alcohol dependence, and
antisocial personality disorder.
–– Heightened sexual activity
initially, followed by impotence and sexual dysfunction.
–– Occasionally, very rapid IV
injection of a large dose produces a condition called “overamped”,
charac-terised by inability to speak or move even though consciousness is fully
retained. Blood pressure and temperature are usually elevated. There may be
respiratory distress.
–– Deterioration of social (family problems), physical (slovenly, unkempt appearance),
and economic (loss of job,
bankruptcy) status.
–– Adverse psychological
reactions—anxiety reactions, amphetamine psychosis, exhaustion syndrome,
depression and hallucinosis.
––
One study revealed that postmortem levels of striatal dopamine in some
methamphetamine users were reduced to levels similar to those seen in patients
with Parkinson’s disease in the caudate, ![]() but not in the putamen subdivision
of the striatum. This reduction of the neurotransmitter in the striatal
subdivision could explain the presence of cognitive problems in methamphetamine
users.
but not in the putamen subdivision
of the striatum. This reduction of the neurotransmitter in the striatal
subdivision could explain the presence of cognitive problems in methamphetamine
users.
––
Medical complications—cardiomyopathy, vascu-litis, pulmonary
hypertension, permanent neurolog-ical deficits, HIV infection, hepatitis,
endocarditis, osteomyelitis, and pulmonary abscesses. Case reports of
hepatotoxicity resulting in hepatocellular injury have been reported in
children receiving pemoline. As of September 1999, pemoline has been withdrawn
from some Western countries. In one case, a young boy unresponsive to other
drugs in the treatment of his attention deficit/hyperactivity disorder (ADHD),
received 75 mg/day of pemoline.
This resulted in liver failure which
required trans-plantation.
–– Obstetric complications (in
pregnant users)— eclampsia, intrauterine growth retardation, prema-turity, etc.
Amphetamine use during pregnancy has also been associated with birth defects,
increased risk of cardiac malformations and cleft palate.
–– Intravenous injection abusers may
display skin lesions, such as “tracks”, abscesses, ulcers, cellu-litis, or
necrotising angitis.
Withdrawal syndrome: Withdrawal after
prolongedamphetamine abuse may precipitate severe depres-sion and suicide
attempts. Anxiety, abdominal cramps, gastroenteritis, headache, diaphoresis,
lethargy, and dyspnoea may result. Increased appetite is common.
Diagnosis
·
Urine is the specimen of choice. Levels above 2 mg/100 ml
indicate acute toxicity. Methods of analysis include TLC, RIA, HPLC, and GC-MS.
The first three methods often give false positive results, and hence
confirmation of a positive test must always be done by GC-MS.
·
A new method (electron-impact mass fragmentography) enables
detection and even quantitation of methampheta-mine in hair, nails, sweat and
saliva.
·
Hair analysis may provide documentation of metham-phetamine
or other drug exposure for several months or longer. The condition of the hair
(wet, dry, dirty, permed or dyed) does not affect results. To obtain hair
samples, a new disposable scissors should be used to cut a very small amount of
hair (100 mg total, about the width of a pencil) from about 10 different
places. The hair must be cut as close to the scalp as possible.
Usual Fatal Dose
The fatal dose of amphetamines is
highly variable, and while death can occur with as little as 1.5 mg/kg of
methamphetamine, survival has been recorded with 28 mg/kg. This in fact
repre-sents the usual range of amphetamine’s lethal dose—150 mg to 2 grams.
However, because of tolerance, addicts can tolerate up to 5 grams (single IV
dose), or 15 gm/day (smokable meth-amphetamine).
Lethal blood level is said to be
around 0.2 mg per 100 ml, though addicts can tolerate much higher levels with
hardly any toxic effects.
Treatment
1. Acute Poisoning:
a. Stabilisation:
–– IV line, cardiac monitoring. ––
Oxygen.
–– Evaluate blood glucose, BUN, and
electrolyte levels.
–– Consider the necessity of a CBC,
urinalysis, coagu-lation profile, chest X-ray, CT scan of head, and lumbar
puncture, depending on the presentation.
––
Measure core temperature.
–– Shock is a poor prognostic sign
and needs to be managed effectively. Consider the need for right-sided heart
catheterisation to measure right-sided filling pressure and cardiac output.
b. Supportive Measures:
–– Airway management, ventilatory
support. –– Rapid rehydration.
–– Mannitol diuresis promotes
myoglobin clearance to prevent renal failure.
––
Assess psychological and neurological status.
–– Gastric decontamination (in cases
of ingestion) with appropriate tracheal protection. Activated charcoal is
beneficial.
c. Specific Measures:
–– Anxiety, agitation, and
hyperactivity can usually be controlled with benzodiazepines. Diazepam is the
drug of choice, and is administered in a dose of 10 mg IV at intervals (up to a
maximum of 100 mg). Much larger doses (hundreds of milligrams) may be required
to obtain adequate sedation. Titrate dose to clinical response. Control of
agitation is an important aspect to the treatment of amphetamine overdose,
since it often leads to hyperthermia, a common cause of mortality in
amphetamine overdose. Neuroleptics are generally not preferred since they may
aggravate hyperthermia, convulsions, and cardiac arrhythmias. Physical restraint
is inadvisable, since resistance against such measures will aggravate
rhabdomyolysis and hyperthermia.
–– Extreme agitation and
hallucinations may require the administration of IV droperidol (up to 0.1 mg/
kg). Since haloperidol lowers the seizures threshold, and is associated with
neuroleptic malignant syndrome, it is not advisable.
––
Convulsions can be managed with benzodiaz-epines (IV diazepam),
phenytoin, or barbiturates.
Refractory cases may require
curarisation.
–– Hyperthermia should be tackled
aggressively with hypothermic blankets, ice baths, and dantrolene infu-sions.
Large IV doses of benzodiazepines can help. Refractory cases must be subjected
to neuromuscular paralysis and mechanical ventilation.
–– Tachycardia can be managed with
beta blockers (atenolol). Labetolol which has combined alpha and beta blocking
effects, may be preferable if tachycardia is associated with hypertension.
Sedation with intra-venous benzodiazepines (diazepam 5 to 10 mg IV repeated
every 5 to 10 minutes as needed) is usually sufficient for treating
hypertension. A short acting, titratable agent such as sodium nitroprusside
should be considered if unresponsive to benzodiazepines.
––
For ventricular arrhythmias: Lignocaine and amiodarone are generally
first line agents for stable monomorphic ventricular tachycardia. Sotalol is a
good alternative. Amiodarone and sotalol should be used with caution if the QT
interval is prolonged, or if torsades de pointes is involved in the overdose.
Unstable rhythms require
cardioversion. Atropine may be used when severe bradycardia is present, and
PVCs are thought to represent an escape complex.
–– For rhabdomyolysis: Early
aggressive fluid replace-ment is the mainstay of therapy, and may help prevent
renal insufficiency. Diuretics such as mannitol or furosemide may be needed to
maintain urine output. Urinary alkalinisation is not routinely recommended.
–– Diazepam and chlorpromazine have
been effective in treating amphetamine-induced chorea.
–– Other complications should be
anticipated and treated as and when they arise.
–– Although peritoneal dialysis and
haemodialysis have been demonstrated to enhance elimination of amphetamine, the
clinical efficacy of these procedures in human overdose has not been proven and
they are rarely if ever clinically indicated. Acidification of urine enhances
amphetamine excretion, but may precipitate acute renal failure in patients with
myoglobinuria and is therefore contraindicated.
Chronic Poisoning:
a. Most casual users of amphetamines
do not need treat-ment. Those with moderately severe dependence can be treated
on an outpatient basis without using drugs. Strategies range from residential
and ambulatory detoxi-fication to day treatment, multistep activities, and case
management. It is preferable to provide a structured and manualised cognitive
behavioural treatment, making use of a combination of group and individual
counselling.![]()
b. A wide variety of pharmacological
agents have been tried as adjuncts to (or major elements in) the treatment of
amphetamine dependence. These include drugs such as imipramine and fluoxetine,
but results have been disappointing.
c. In some European countries,
low-dose amphetamines are administered to addicts as part of the detoxification
programme in the initial stages, to assist the subject over-come the phase of
“craving”. There are however doubts expressed by other investigators over such
an approach.
Related Topics