Chapter: Modern Medical Toxicology: Substance Abuse: Substances of Dependence and Abuse
Cocaine: Diagnosis, Treatment - Substances of Dependence and Abuse
Diagnosis
·
Blood or plasma cocaine levels are not clinically useful,
although they may be advisable to be done in medico-legal cases. Qualitative
urine tests using kits may be helpful in clinical diagnosis (by utilising
chromatography, radioim-munoassay, enzyme immunoassay, fluorescence
polarisa-tion immunoassay, and enzyme-multiplied immunoassay technique).
Cocaine metabolites can be identified in the urine and provide a method for
qualitatively identifying suspected cocaine poisoning or abuse.
Benzoylecgonine, the major metabolite of cocaine, can usually be detected in
urine for 48 to 72 hours after cocaine use.
·
Other diagnostic clues—
o Hair analysis: Cocaine benzoylecgonine and ecgo-nine methylester can be
analysed in hair samples by GC-MS and RIA. This can be done in adults, as well
as in any infant whose mother was a cocaine user. It must be noted that
external contamination of hair can occur from crack smoke, but that can be
washed off, whereas systemic exposure is not affected by washing the hair.![]()
o ECG: Non-Q-wave myocardial infarction, with the pres-ence of a
T-wave infarct ECG pattern is often seen in cocaine users. During acute cocaine
use abnormalities are more prevalent, and the QT interval is prolonged.
Two-dimensional echocardiography may be useful in detecting the presence of new
regional wall-motion abnormalities in patients experiencing cocaine-induced
chest pain.
o Troponin levels may be more useful
in evaluating potential myocardial injury than creatinine kinase.
o Acid-base abnormalities: Arterial blood gases incocaine
abusers show a pH varying from 7.35 to 7.5. Alkalosis (pH > 7.45) is caused
by hyperventilation, and is manifested by tachypnoea and low PaCO2.
About one third of patients show evidence of acidosis which may be the result
of hypoventilation secondary to depressed mental status or chest trauma.
Metabolic acidosis is not uncommon, and usually results from convulsions,
agitation, or trauma.
o Estimate serum creatine kinase for
evidence of rhab-domyolysis. Monitor renal function and urine output in
patients with elevated CPK.
o X-ray: Body packer syndrome can bediagnosed by plain films of the
abdomen in the supine and upright positions. However, false negatives have been
reported. Radiography may not detect cellophane-wrapped packets or crack vials.
Even false-negative abdominal CT scans have been reported. It is therefore
advisable to perform a contrast study of the bowel with follow-up X-rays 5
hours after the oral ingestion of a water-soluble contrast compound such as
meglumine amidotrizoate (50 ml). Daily views are performed there-after until
negative views coincide with the passage of two drug packet-free stools.
Treatment
Acute Poisoning
Activated
charcoal adsorbs cocaine in vitro under both acidic and alkaline conditions,
and can be administered in cases of ingestion.
a. Hyperthermia:
––
Minimise physical activity and sedate with benzo-diazepines.
––
Ice baths, packs, cool water with fans, etc. –– Oxygen D50W
(as necessary).
––
Diazepam 5 mg IV or lorazepam 2–4 mg IV titrated to effect.
––
Paracetamol 2000 mg (in the form of 500 mg rectal suppositories).
–– Severe, intractable cases may respond to dantrolene (1 mg/kg) every 6 hours. Alternatively, bromocrip-tine can be administered orally in a nasogastric tube.
b. Anxiety and agitation:
––
Diazepam 5–10 mg IV, or lorazepam 2–4 mg IV titrated to effect.
–– Physical restraints.
––
Antipsychotics such as haloperidol or droperidol, and phenothiazines are not
recommended since they can induce malignant hyperthermia and convul-sions.
c.
Convulsions:
––
Diazepam 5–10 mg IV, or lorazepam 2–4 mg IV titrated to effect.
–– Phenobarbitone 25–50 mg/min up to 10–20
mg/kg. –– If seizures are not controlled
by the above measures, consider continuous infusion of midazolam (0.2 mg/ kg
slow bolus, or 0.75 to 10 mcg/kg/min as infu-sion), or propofol (1 to 2 mg/kg,
followed by 2 to 10 mg/kg/hr) or pentobarbitone (10 to 15 mg/kg at a rate of 50
mg/min, followed by 0.5 to 1 mg/kg/hr).
––
Intractable convulsions may require neuromuscular paralysis with intubation and
mechanical
ventila-tion.
d. Cerebrovascular accidents:
Neurosurgical consultation is mandatory.
e. Hypertension: It is usually
short-lived and often followed by significant hypotension. Mild hypertension
generally responds to sedation with benzodiazepines. For severe hypertension—
––
Without tachycardia:
-- Phentolamine 0.02 to 0.1 mg/kg IV
-- Nifedipine 0.1 to 0.2 mg/kg IV
--
Nitroprusside 2 to 10 mcg/kg/min IV
–– With tachycardia: If the above
measures are not effective, the following may be used—
-- Labetolol 10 to 20 mg IV,
repeated every 10 minutes (max: 300 mg).
-- Nitroglycerine IV titrated to
effect. –– With chest pain—
--
Nitroglycerine drip.
-- Oxygen by nasal cannula (5
L/min). -- Monitor cardiac status.
-- If systolic BP is higher than 120
mmHg, admin-ister nitroglycerine sublingually (up to 3 tablets or 3 sprays of
0.4 mg each).
-- If pain does not respond to
nitroglycerine, use morphine (2 mg IV titrated to pain relief).
--
Obtain ECG.
--
If chest pain is strongly suggestive of a myocar-dial infarction,
consider thrombolytic therapy.
-- Diazepam 5 mg IV, or lorazepam
2–4 mg IV titrated to effect can prevent excess production of catecholamines by
the CNS.
--
Mechanical reperfusion (angioplasty).
f. Arrhythmias:
–– Sinus tachycardia: -- Observation
-- Oxygen
--
D50W (as necessary)
--Diazepam 5–10 mg IV, or lorazepam
2–4 mg IV titrated to effect (if indicated).
–– Supraventricular tachycardia: --
Observation
--
Oxygen
--
D50W ( as neccesary)
-- Diltiazem 20 mg IV, or verapamil
5 mg IV -- Adenosine 6–12 mg IV for AV node re-entry -- Cardioversion (if
necessary).
–– Ventricular arrhythmias: Obtain
an ECG, institute continuous cardiac monitoring and administer oxygen. Evaluate
for hypoxia, acidosis, and electrolyte disorders (particularly hypokalaemia,
hypocalcaemia, and hypomagnesaemia).
--
Oxygen
--
D50W (as necessary)
-- Hypertonic sodium bicarbonate:
Sodium bicarbonate may be useful in the treatment of QRS widening and
ventricular arrhythmias associated with acute cocaine use. A reason-able
starting dose is 1 to 2 mEq/kg repeated as needed. Monitor arterial blood
gases, maintain pH 7.45 to 7.55.
-- Diazepam 5 mg IV, or lorazepam
2–4 mg IV. -- Lignocaine 1.5 mg/kg IV bolus, followed by 2 mg/min infusion.
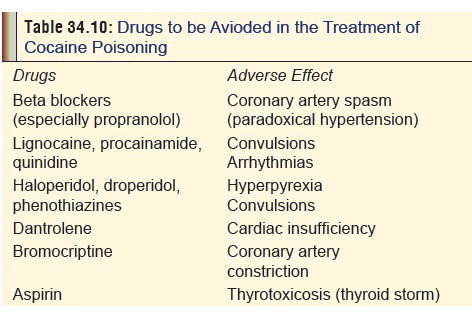
Watch out for adverse effects (Table
34.10). Procainamide may also be used with caution.
--
Defibrillation (if haemodynamically unstable).
g. Myocardial infarction: Acute
myocardial infarction due to cocaine toxicity must be treated on the same lines
as myocardial infarction in non-cocaine users, except for the use of beta
blockers. The following measures are recommended:
–– IV line –– Oxygen
–– Aspirin to inhibit platelet
aggregation. Watch out for increased thyroxine levels.
–– For systolic BP higher than 100
mmHg, administer sublingual nitroglycerine or nifedipine 10 mg orally, or
phentolamine 1 to 5 mg IV (followed by a drip of 10 mg in 1 litre of D5W
at 10 ml/min).
--For life-threatening arrhythmias,
use of type IA antiarrhythmic agents may be considered (with caution).
--Thrombolytic therapy may be
necessary if myocardial infarction is not amenable to relief by nitrates,
calcium channel blockers, or phentolamine. Caution about the use of
throm-bolytics in cocaine-associated acute myocar-dial infarction (AMI) is
generally advocated. Thrombolytics should be avoided in patients with
cocaine-induced myocardial infarction and uncontrolled hypertension, because of
the increased risk of intracranial haemorrhage. However, some investigators
feel that the risk is often exaggerated.
h. Aortic dissection: The
hypertension that precipitated aortic dissection must be controlled immediately
with nitroprusside and calcium channel blockers.
i. Pulmonary oedema:
––
Frusemide 20–40 mg IV.
–– Morphine sulfate 2 mg IV titrated
to pain relief. –– Nitroglycerine drip titrated to blood pressure or
respiratory status.
–– Phentolamine or nitroprusside (if
necessary). –– Incubate and ventilate.
––
Monitor fluids with pulmonary artery catheter.
j. Rhabdomyolysis: Early aggressive
fluid replacement is the mainstay of therapy and may help prevent renal
insufficiency. Diuretics such as mannitol or furosemide may be needed to
maintain urine output. Urinary alka-linisation is not routinely recommended.
––
Cardiac monitoring.
––
Serial potassium determinations.
–– Serial serum creatine kinase and
urine myoglobin studies.
–– IV hydration (urine output must
be maintained at 3 ml/kg/hr).
–– Dopamine (3 mcg/kg/day) and
frusemide (60 mg three times a day) may reduce renal vascular resist-ance and
help in reducing the number of haemodi-alysis required to reverse oliguria.
k. Acidosis: Correction of acidaemia
through supportive care measures such as hyperventilation, sedation, active
cooling, and sodium bicarbonate infusion can have beneficial effects on
conduction defects.
l. Elimination enhancement measures:
Cocaine is rapidly metabolised. Forced diuresis, urine acidifica-tion,
dialysis, and haemoperfusion are ineffective in significantly altering
elimination. Increasing the level of butyrylcholinesterase in the blood (which
metabolises cocaine to inactive compounds) could help in rapidly inactivating
cocaine in acute intoxications.
Chronic Poisoning
A number of psychological and
pharmacological approaches to the treatment of cocaine dependence have been
tried with varying degrees of success. A combined approach judiciously tailored
to the needs of individual patients offers the best hope of preventing
relapses.![]()
a. Psychotherapy: This involves
cognitive-behavioural, psychodynamic, and general supportive techniques.
One example of a
cognitive-behavioural method uses contingency contracting, in which it is
agreed in advance that for a specified period of time (e.g. 3 months), if the
patient uses cocaine (as detected by supervised urine testing), the therapist
will initiate action that will result in serious adverse consequences for the
patient, such as informing the employer.
b. Group psychotherapy:
–– Interpersonal group therapy
focuses on relation-ships, and uses the group interactions to illustrate the
interpersonal causes of individual distress, and to offer alternative
behaviours.
–– Modified dynamic group therapy is
concerned with emphasising character as it manifests itself indi-vidually and
intrapsychically, and in the context of interpersonal relationships with a
focus on affect, self-esteem and self-care.
c. Group counselling: The most
widely used form of psychosocial treatment for cocaine dependence is group
counselling, in which the group is open-ended with rolling admissions; the
group leaders are drug counsellors, many of whom are recovering from addiction,
and the emphasis is on providing a supportive atmosphere, discussing problems
in recovery, and encouraging participation in multistep programmes.
d. Pharmacotherapy:
–– Several drugs have been tried to
help ameliorate the manifestations of cocaine withdrawal. Many of these
(fenfluramine, trazodone, neuroleptic agents, etc.) have either not
demonstrated clinical efficacy, or have produced serious side effects.
––
Bromocriptine has successfully reduced cocaine craving and decreased
withdrawal symptoms in several studies. Oral doses of 0.625 mg given 4 times
daily may produce a rapid decrease in psychiatric symptoms. When given in a
single dose of 1.25 mg, bromocriptine has been found to decrease cocaine
craving. In one study, the dosage suggested was 1.25 mg orally twice daily,
with titration up to 10 mg per day within the first 7 days.
Dose can be decreased in patients
experiencing adverse effects.
–– Amantadine, a dopamimetic agent, increases dopaminergic transmission and has been found to be useful in the treatment of early withdrawal symptoms and short-term abstinence. The usual dose recommended is 200 mg to 400 mg orally, daily, for up to 12 days. It is probably as effective as bromocriptine, and less toxic.
–– Tricyclic antidepressants may be useful for selected cocaine users with comorbid depression or intra-nasal use.
–– Initial studies with fluoxetine promised good results, but craving actually worsened in some patients. Several studies indicated better effi-cacy with carbamazepine for controlling craving. Carbamazepine at doses of 200 to 800 mg orally, 2 to 4 times daily has benefited some patients. Phenytoin also shows promise in helping to sustain abstinence from cocaine in some patients.
–– Recent approaches include the
employment of agents that selectively block or stimulate dopa-mine receptor
subtypes (e.g. selective D1 agonists), and drugs that can
selectively block the access of cocaine to the dopamine transporters, and yet
still permit the transporters to remove cocaine from the synapse.
–– Another approach is aimed at
preventing cocaine from reaching the brain by using antibodies to bind cocaine
in the blood stream (“cocaine vaccine”).
e. Acupuncture: Use of auricular
acupuncture to treat cocaine abuse has become popular of late, though
controlled studies of its efficacy have not shown convincing results. Herbal
teas are often consumed as part of the treatment. Unfortunately, drop-out rates
are generally high.
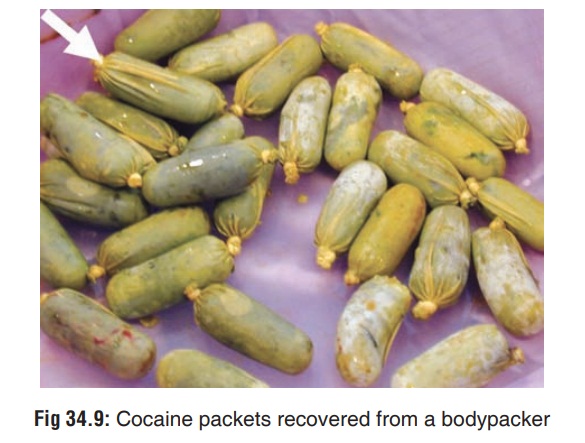
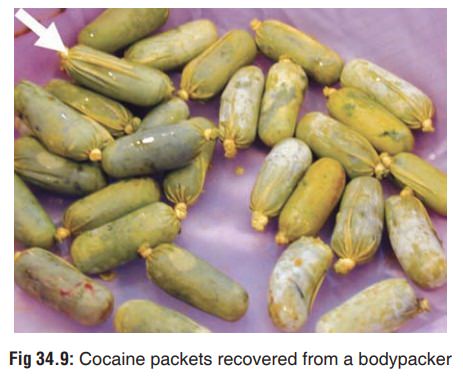
Bodypacker Syndrome
The practice of swallowing balloons,
condoms, or plastic packets filled with illegal drugs for the purpose of
smuggling is called “body packing”, (Fig
34.9) and the individual who does this is referred to as a “mule”. This
must be differentiated from “body stuffing” in which an individual who is on
the verge of being arrested for possession of illegal drugs, swallows his illicit
contraband to conceal the evidence. Leaking from these poorly wrapped packets
can produce cocaine toxicity. Sudden death due to massive overdose can occur in
either a bodypacker or a bodystuffer, if one or more of the ingested packages
burst within the gastrointestinal tract. Fatal cocaine poisoning has occurred
with the rupture of just a single package.
a. Diagnosis
b. Treatment:
–– Emesis, lavage, charcoal, as applicable.
–– Cathartic/whole bowel irrigation
to flush the pack-ages out of the intestines.
–– Symptomatic patients should be
considered a medical emergency, and be evaluated for surgical removal of the
packets.
–– Asymptomatic patients should be
monitored in an intensive care unit until the cocaine packs have been
eliminated. This must be confirmed by follow-up plain radiography and barium
swallows.
–– Bowel obstruction in asymptomatic
patients may necessitate surgery. Endoscopic removal has been successful in
some cases.
Autopsy Features
·
There are no specific findings at autopsy, except for nasal
septal ulceration and perforation if the deceased had been a long-term abuser
of cocaine. Histological study of nasal septal mucosa in such cases may reveal
characteristic changes including arteriolar thickening, increased perivas-cular
deposition of collagen and glycoprotein, and chronic inflammatory cellular
infiltration.
·
Histopathology of heart may demonstrate microfocal
lymphocytic infiltrates, acute coronary thrombosis, early coagulation necrosis
of myocardial fibres, and non-athero-sclerotic coronary obstruction due to
intimal proliferation.
·
Cocaine can be recovered by sampling from recent injec-tion
sites, or by swabs from the nasal mucosa. It can also be recovered from the
liver and especially brain, where cocaine may be found not only in
dopamine-rich areas such as caudate, putamen, and nucleus accumbens, but also
in other extra-striatal regions. Specimens obtained postmortem should be
preserved with sodium fluoride, refrigerated, and analysed quickly. Tissue
specimens should be frozen.
Forensic Issues
·
Cocaine has been abused for centuries, but its toxic proper-
ties have been studied extensively only in the last couple of decades. In the current drug subculture,
cocaine has become the “champagne drug”
because of its cost and relative scarcity. Cocaine is a “rich man’s drug” since
the poorer classes cannot afford to sustain a drug habit that costs thousands
of rupees every week. Therefore in India, cocaine abuse is restricted mainly to
the affluent classes of society. The prevalence and extent of the problem among
newer generation Indian film actors in recent times has become apparent with
the arrest of several filmstars for possession of cocaine. Several high profile
artists, socialites, and even politicians have been caught with cocaine
possession.
·
Cocaine has always been popular with musicians (espe- cially
jazz and rock), other artistes, and film personalities. There are innumerable
rock songs eulogising the drug directly or indirectly.
·
Today cocaine has made inroads into the general popula-tion,
especially adolescents. After the cocaine epidemic of the 1970s (“snorting
seventies”) in the West, there had been relative lull in the 1980s and early
1990s. A recent survey shows the cocaine resurgence of the 21st century has not
only affected Western countries, but even poorer countries such as India. In
fact a sizeable chunk of youth (including girls) from well-to-do families in
metropolitan cities such as
·
Mumbai, Delhi, and Bangalore have no qualms about drug
abuse, and even openly admit to using “party drugs” such as cocaine as a “cool”
mode of recreation. Since cocaine has a reputation of enhancing sexual
pleasure, such wide-spread abuse has also led to increased spread of sexually
transmitted diseases such as AIDS because of high-risk sexual practices among
the users.
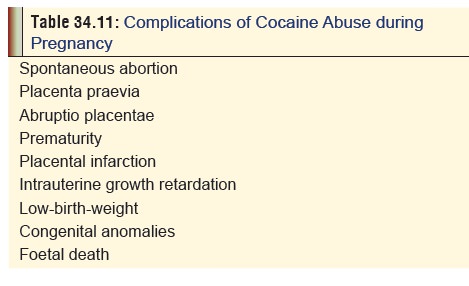
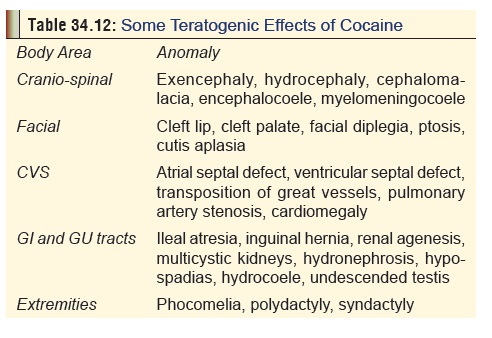
·
Cocaine abuse by pregnant mothers can lead to devastating
effects on the foetus and the new-born (Table
34.11). There is convincing evidence that cocaine is teratogenic and can
play an important role in the causation of several serious congenital anomalies
(Table 34.12).
·
Cocaine abuse is well known for its propensity to cause
sudden death not only due to its deleterious effects onhealth (cerebrovascular
accidents, myocardial infarction, malignant hyperthermia, renal failure), but
also due to its capacity to provoke the user to commit acts of aggression and
violence. Deaths due to massive overdose are especially common among those who
smuggle the drug within their bodies (“cocaine packers”).
· Cocaine toxicity has been reported in children receiving topical adrenaline and cocaine for local anaesthesia.
Related Topics