Chapter: Medicine and surgery: Hepatic, biliary and pancreatic systems
Gallstone disease (cholelithiasis) - Disorders of the gallbladder
Disorders of the gallbladder
Gallstone disease (cholelithiasis)
Definition
Gallstones form from bile constituents in the gallbladder and bile ducts.
Incidence/prevalence
The most common disease affecting the biliary tract and is increasing in frequency. It affects more than 20% of women and 8% of men in the United Kingdom, although >70% remain asymptomatic.
Age
Increases with age, most patients >40 years.
Sex
F > M (2:1)
Geography
More common in developed world.
Aetiology
Gallstones may be cholesterol stones (more common in the developed world), pigment stones (more common in the Far East) or mixed stones.
Cholesterol stones are predisposed to by supersaturation of bile with cholesterol. Normally bile salts and lecithin keep the cholesterol soluble, forming micelles.
· Increased cholesterol: Obesity and rich, fatty diets can cause cholesterol-rich bile to be secreted. Conversely, sudden weight reduction and cholesterol-reducing diets may precipitate gallstones by mobilising cholesterol stores from the liver. However, hypercholesterolaemia has not been associated with gallstones.
· Increased concentration: Stone formation is more likely when the bile is concentrated, due to stasis, reduced gallbladder contractility or a reduced bile salt pool.
· Precipitants: Gallstone formation may be around a focus or ‘nucleus’ such as bacteria, cells or other particulate matter.
· Reduced bile salt pool: Bile salts are normally recycled by reabsorption at the terminal ileum through the enterohepatic circulation. Malabsorption (e.g. in cystic fibrosis, Crohn’s disease or resection of the terminal ileum) can lead to reduced amounts of bile and predispose to nucleation.
· Hormonal influences have been implicated: Pregnancy, the oral contraceptive pill and hormone replacement therapy all increase the incidence of stone formation.
· Pigment stones mainly consist of calcium bilirubinate. Predisposing factors:
· Increased production of bilirubin: Chronic haemolysis such as in congenital spherocytosis, haemo-globinopathies and malaria leads to increased production of conjugated bilirubin.
· Cirrhosis, biliary stasis and chronic biliary infections also predispose, although the mechanism is unknown.
Bacterial action on bilirubin has been postulated. Mixed stones are associated with anatomical abnormalities, stasis and previous surgery.
Pathophysiology
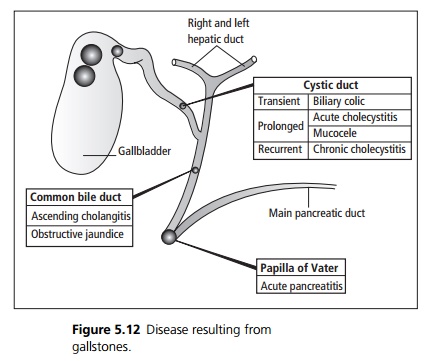
Several different patterns of disease may result from gall-stones depending on where the gallstones are located (see Fig. 5.12).
Clinical features
Gallstones in the gallbladder are asymptomatic in 90% of cases.
Impaction of a gallstone in the outlet of the gallbladder or in the cystic duct produces biliary colic, a severe colicky pain in the epigastrium and right hypochondrium, radiating to the back. Onset is often after a meal or in the evening, the pain is variable in intensity over several hours. Associated features are nausea, vomiting and retching. Jaundice may occur.
Acute cholecystitis may result from gallstone obstruction. Inflammation is initially caused by concentrated bile. Secondary infection is common usually due to Escherichia coli, Klebsiella aerogenes and Streptococcus faecalis. Patients develop acute onset of severe griping pain in the right upper quadrant radiating to the right subscapular region and occasionally to the right shoulder. Associated features include fever, tachycardia, nausea, vomiting and occasionally jaundice. On examination there is abdominal tenderness and guarding in the right upper quadrant, which may become generalised due to peritonitis, a gallbladder mass may be felt due to wrapped omentum. Murphy’s sign is usually present (inspiration during right hypochondrial palpation causes pain and arrest of inspiration as the inflamed gallbladder moves downwards and impinges on the fingers).
Chronic cholecystitis probably results from a combination of gallstones, chemical inflammation due to bile and repeated attacks of acute cholecystitis. Patients complain of a vague intermittent right upper quadrant discomfort, with feelings of distension flatulence and an aversion to fatty foods.
Patients may also present with ascending cholangitis (abdominal pain, high fever and obstructive jaundice) or acute pancreatitis.
Macroscopy
Cholesterol stones are yellow to green in colour with a rough surface, typically rounded, faceted and large (usually up to 3 cm in size). Pigment stones are often multiple, small and irregular in shape. They are usually <1 cm across.
Complications
A mucocele occurs when long-standing obstruction occurs without infection, the bile is resorbed and instead the epithelium secretes clear mucus. Acute cholecystitis may lead to empyema (pusfilled gallbladder), perforation with abscess formation and biliary peritonitis (chemical and bacterial).
Investigations
Full blood count (and investigation for haemolytic anaemia in pigment gallstones). Liver function tests, blood cultures, inflammatory markers and amylase should be sent.
ERCP (endoscopic retrograde cholangiopancreatography) is used for the detection and removal of stones from the common bile duct or papilla of Vater.
Ultrasound can demonstrate the presence of gallstones and detect dilatation of ducts.
Plain abdominal X-ray demonstrates radioopaque stones (15%).
Management
Patients with asymptomatic gallstones are usually managed conservatively.
Patients with impacted stones or acute cholecystitis require adequate analgesia and antibiotics to prevent or treat cholangitis. Stones impacted at the papilla of Vater may need to be removed at ERCP.
Patients with empyema or acute ascending cholangitis may require drainage procedures.
Cholecystectomy may be performed as an open or laparoscopic procedure. It may be performed as an emergency (severe or complicated acute cholangitis), early elective (during initial admission for acute cholangitis) or delayed elective (following biliary colic, acute pancreatitis, acute cholangitis or chronic cholangitis)
Prognosis
In acute cholecystitis 90% of patients settle with conservative management within 4–5 days. Ascending cholangitis has a mortality of up to 20% in severe cases requiring emergency decompression.
Related Topics