Chapter: Essentials of Anatomy and Physiology: The Reproductive Systems
Female Reproductive System in Human
FEMALE REPRODUCTIVE SYSTEM
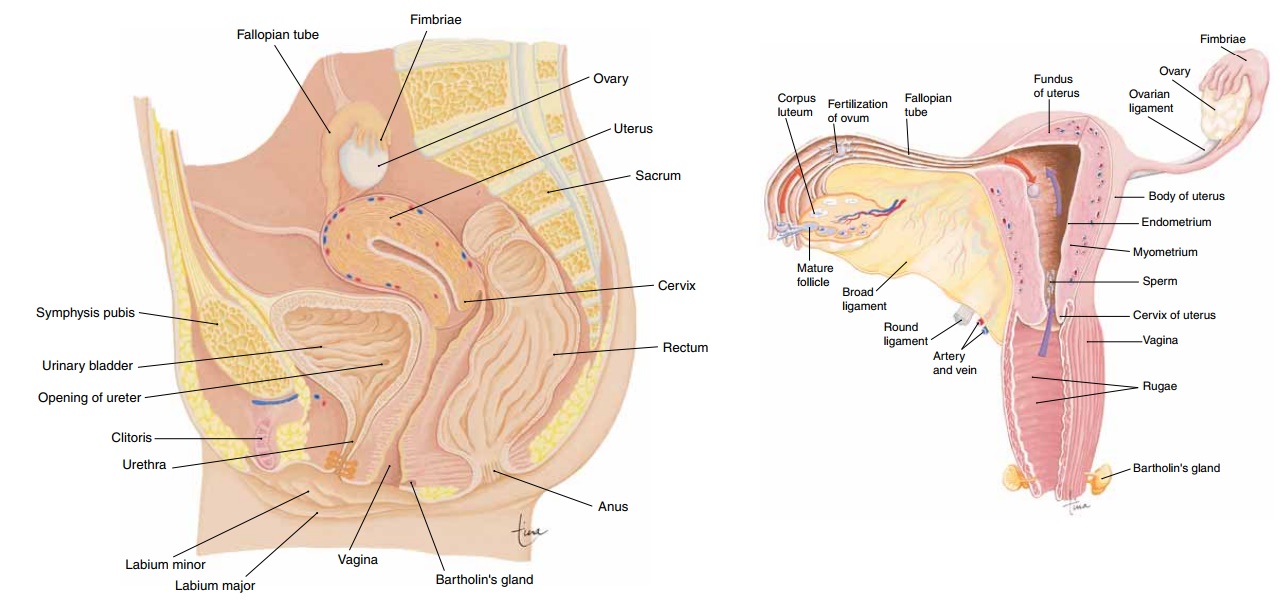
The female reproductive system consists of the paired ovaries and fallopian tubes, the single uterus and vagina, and the external genital structures (Fig. 20–5). Egg cells (ova) are produced in the ovaries and travel through the fallopian tubes to the uterus. The uterus is the site for the growth of the embryo-fetus.
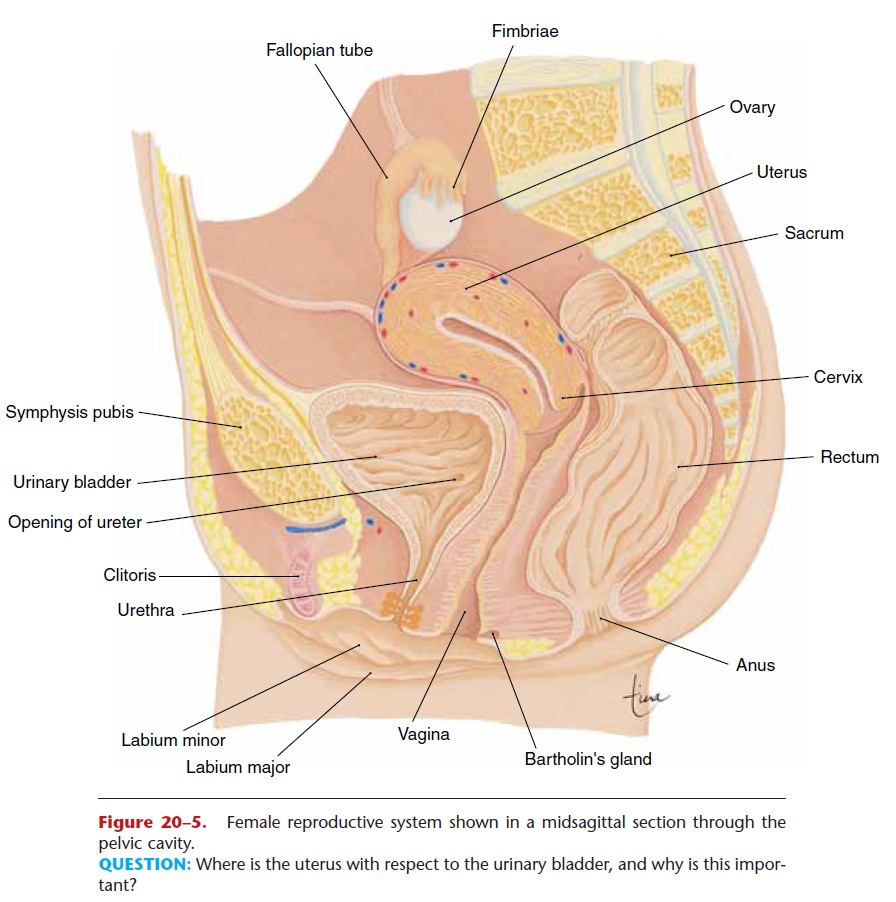
Figure 20–5. Female reproductive system shown in a midsagittal section through the pelvic cavity.
OVARIES
The ovaries are a pair of oval structures about 1.5 inches (4 cm) long on either side of the uterus in the pelvic cavity (Fig. 20–6). The ovarian ligament extends from the medial side of an ovary to the uter-ine wall, and the broad ligament is a fold of the peritoneum that covers the ovaries. These ligaments help keep the ovaries in place.
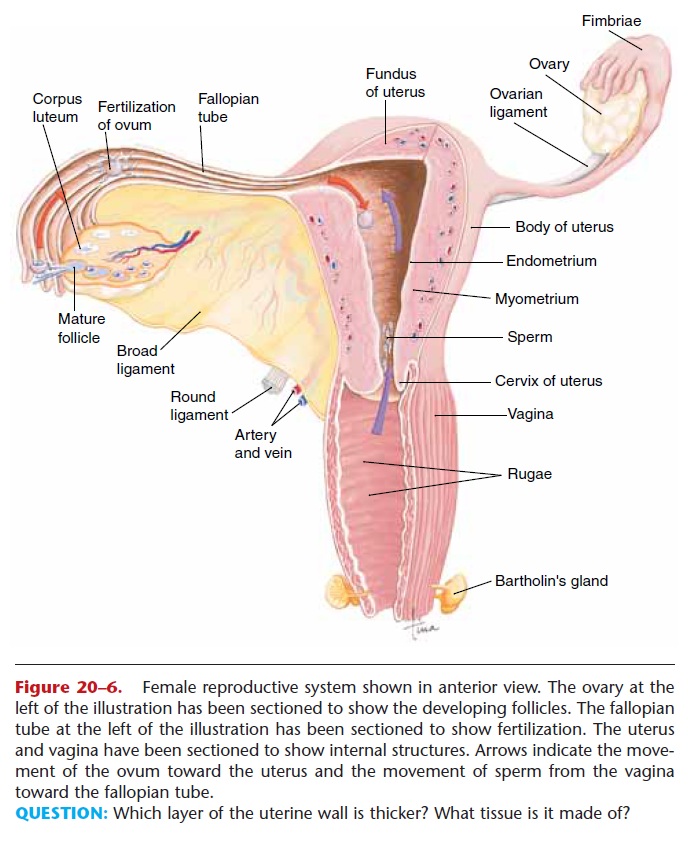
Figure 20–6. Female reproductive system shown in anterior view. The ovary at the left of the illustration has been sectioned to show the developing follicles. The fallopian tube at the left of the illustration has been sectioned to show fertilization. The uterus and vagina have been sectioned to show internal structures. Arrows indicate the move-ment of the ovum toward the uterus and the movement of sperm from the vagina toward the fallopian tube.
QUESTION: Which layer of the uterine wall is thicker? What tissue is it made of?
Within an ovary are several hundred thousand pri-mary follicles, which are present at birth. During a woman’s childbearing years, only 300 to 400 of these follicles will produce mature ova. As with sperm pro-duction in men, the supply of potential gametes far exceeds what is actually needed, but this helps ensure the continuation of the human species.
Each primary ovarian follicle contains an oocyte, a potential ovum or egg cell. Surrounding the oocyte are the follicle cells, which secrete estrogen. Matura-tion of a follicle, requiring FSH and estrogen, was described previously in the section on oogenesis. A mature follicle may also be called a graafian follicle, and the hormone LH from the anterior pituitary gland causes ovulation, that is, rupture of the mature follicle with release of the ovum. At this time, other developing follicles begin to deteriorate; these are called atretic follicles and have no further purpose.
Under the influence of LH, the ruptured follicle becomes the corpus luteum and begins to secrete progesterone as well as estrogen. Hormones produced in smaller amounts by the corpus luteum are inhibin and relaxin.
FALLOPIAN TUBES
There are two fallopian tubes (also called uterine tubes or oviducts); each is about 4 inches (10 cm) long.
The lateral end of a fallopian tube encloses an ovary, and the medial end opens into the uterus. The end of the tube that encloses the ovary has fimbriae, fringe-like projections that create currents in the fluid sur-rounding the ovary to pull the ovum into the fallopian tube.
Because the ovum has no means of self-locomotion (as do sperm), the structure of the fallopian tube ensures that the ovum will be kept moving toward the uterus. The smooth muscle layer of the tube contracts in peristaltic waves that help propel the ovum (or zygote, as you will see in a moment). The lining (mucosa) is extensively folded and is made of ciliated epithelial tissue. The sweeping action of the cilia also moves the ovum toward the uterus.
Fertilization usually takes place in the fallopian tube. If not fertilized, an ovum dies within 24 to 48 hours and disintegrates, either in the tube or the uterus. If fertilized, the ovum becomes a zygote and is swept into the uterus; this takes about 4 to 5 days.
Sometimes the zygote will not reach the uterus but will still continue to develop. This is called an ectopic pregnancy; ectopic means “in an abnormal site.” The developing embryo may become implanted in the fal-lopian tube, the ovary itself, or even elsewhere in the abdominal cavity. An ectopic pregnancy usually does not progress very long, because these other sites are not specialized to provide a placenta or to expand to accommodate the growth of a fetus, as the uterus is. The spontaneous termination of an ectopic pregnancy is usually the result of bleeding in the mother, and sur-gery may be necessary to prevent maternal death from circulatory shock. Occasionally an ectopic pregnancy does go to full term and produces a healthy baby; such an event is a credit to the adaptability of the human body and to the advances of medical science.
UTERUS
The uterus is shaped like an upside-down pear, about 3 inches long by 2 inches wide by 1 inch deep (7.5 cm by 5 cm by 2.5 cm), superior to the urinary bladder and between the two ovaries in the pelvic cavity (see Fig. 20–5). The broad ligament also covers the uterus (see Fig. 20–6). During pregnancy the uterus increases greatly in size, contains the placenta to nour-ish the embryo-fetus, and expels the baby at the end of gestation.
The parts and layers of the uterus are shown in Fig. 20–6. The fundus is the upper portion above the entry of the fallopian tubes, and the body is the large central portion. The narrow, lower end of the uterus is the cervix, which opens into the vagina.
The outermost layer of the uterus, the serosa or epimetrium, is a fold of the peritoneum. The myome-trium is the smooth muscle layer; during pregnancy these cells increase in size to accommodate the grow-ing fetus and contract for labor and delivery at the end of pregnancy.
The lining of the uterus is the endometrium, which itself consists of two layers. The basilar layer, adjacent to the myometrium, is vascular but very thin and is a permanent layer. The functional layer is regenerated and lost during each menstrual cycle. Under the influence of estrogen and progesterone from the ovaries, the growth of blood vessels thick-ens the functional layer in preparation for a possible embryo. If fertilization does not occur, the functional layer sloughs off in menstruation. During pregnancy, the endometrium forms the maternal portion of the placenta.
VAGINA
The vagina is a muscular tube about 4 inches (10 cm) long that extends from the cervix to the vaginal orifice in the perineum (pelvic floor). It is posterior to the urethra and anterior to the rectum (see Fig. 20–5). The vaginal opening is usually partially covered by a thin membrane called the hymen, which is ruptured by the first sexual intercourse or by the use of tampons during the menstrual period.
The functions of the vagina are to receive sperm from the penis during sexual intercourse, to provide the exit for menstrual blood flow, and to become the birth canal at the end of pregnancy.
The vaginal mucosa after puberty is stratified squamous epithelium, which is relatively resistant to pathogens. The normal flora (bacteria) of the vagina creates an acidic pH that helps inhibit the growth of pathogens.
EXTERNAL GENITALS
The female external genital structures may also be called the vulva (Fig. 20–7), and include the clitoris, labia majora and minora, and the Bartholin’s glands (see Fig. 20–5).
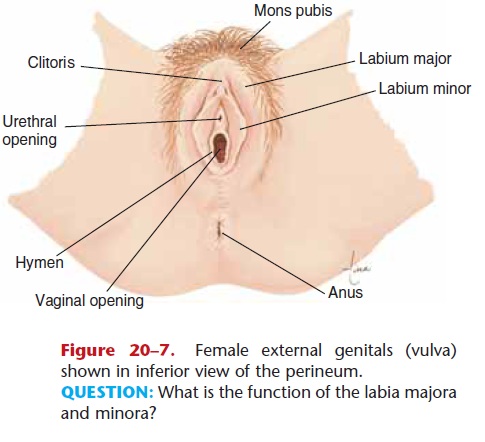
Figure 20–7. Female external genitals (vulva) shown in inferior view of the perineum. QUESTION: What is the function of the labia majora and minora?
The clitoris is a small mass of erectile tissue ante-rior to the urethral orifice. The only function of the clitoris is sensory; it responds to sexual stimulation, and its vascular sinuses become filled with blood.
The mons pubis is a pad of fat over the pubic sym-physis, covered with skin and pubic hair. Extending posteriorly from the mons are the labia majora (lat-eral) and labia minora (medial), which are paired folds of skin. The area between the labia minora is called the vestibule and contains the openings of the urethra and vagina. The labia cover these openings and prevent drying of their mucous membranes.
Bartholin’s glands, also called vestibular glands (see Figs. 20–5 and 20–6), are within the floor of the vestibule; their ducts open onto the mucosa at the vaginal orifice. The secretion of these glands keeps the mucosa moist and lubricates the vagina during sexual intercourse.
MAMMARY GLANDS
The mammary glands are structurally related to the skin but functionally related to the reproductive sys-tem because they produce milk for the nourishment of offspring. Enclosed within the breasts, the mammary glands are anterior to the pectoralis major muscles; their structure is shown in Fig. 20–8.
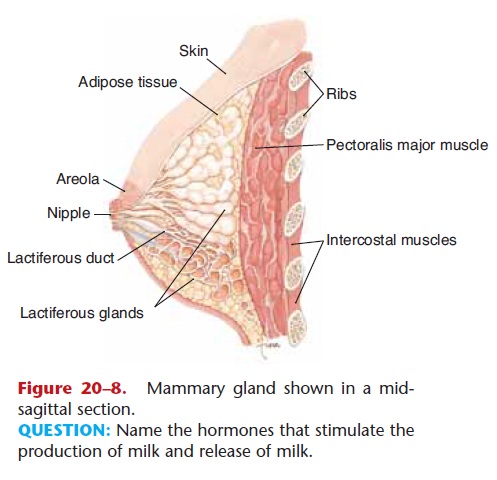
Figure 20–8. Mammary gland shown in a mid-sagittal section.
QUESTION: Name the hormones that stimulate the production of milk and release of milk.
The glandular tissue is surrounded by adipose tis-sue. The alveolar glands produce milk after preg-nancy; the milk enters lactiferous ducts that converge at the nipple. The skin around the nipple is a pig-mented area called the areola.
The formation of milk is under hormonal control. During pregnancy, high levels of estrogen and proges-terone prepare the glands for milk production. Prolactin from the anterior pituitary gland causes the actual synthesis of milk after pregnancy. The sucking of the infant on the nipple stimulates the hypothala-mus to send nerve impulses to the posterior pituitary gland, which secretes oxytocin to cause the release of milk. The effects of these hormones on the mammary glands are summarized in Table 20–2.

THE MENSTRUAL CYCLE
The menstrual cycle includes the activity of the hor-mones of the ovaries and anterior pituitary gland and the resultant changes in the ovaries (ovarian cycle) and uterus (uterine cycle). These are all incorporated into Fig. 20–9, which may look complicated at first, but refer to it as you read the following.
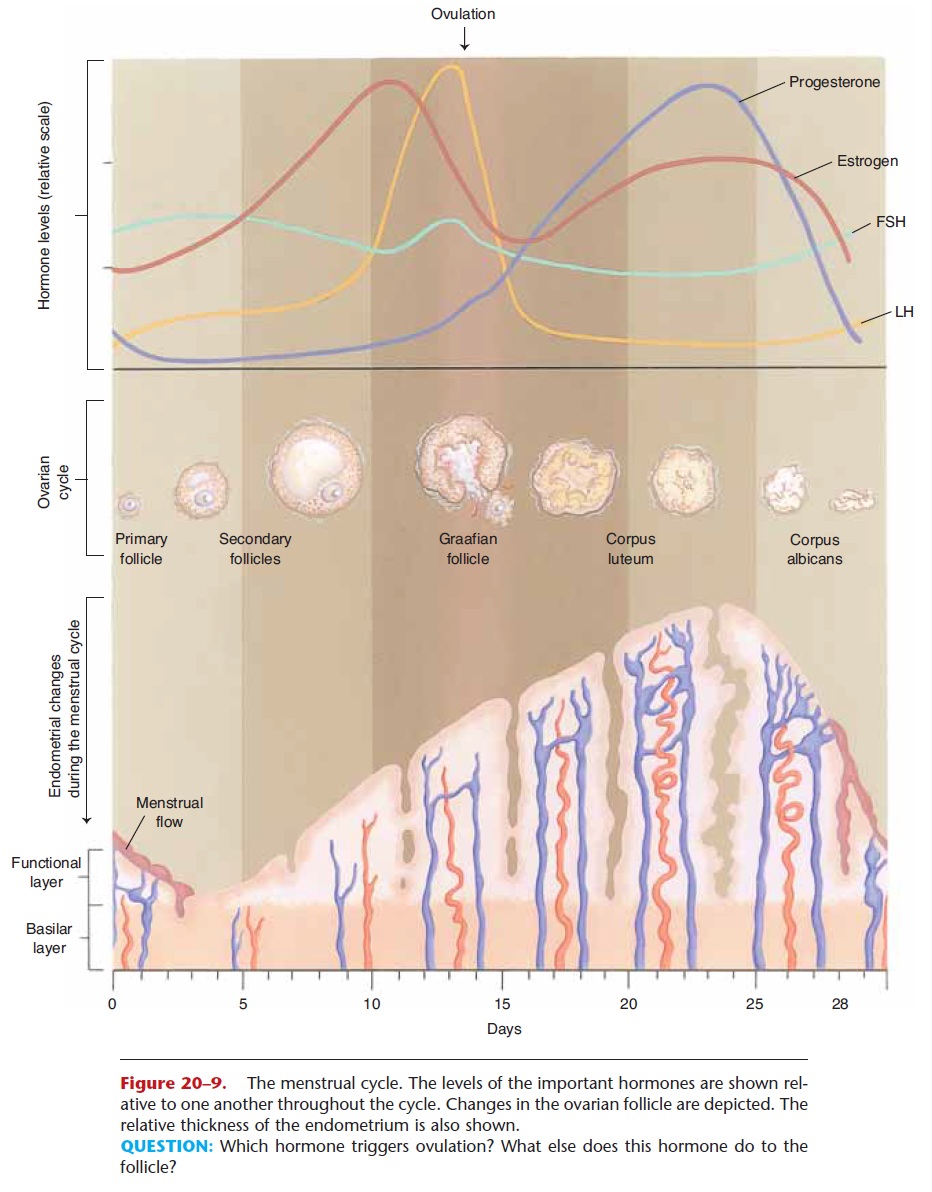
Figure 20–9. The menstrual cycle. The levels of the important hormones are shown rel-ative to one another throughout the cycle. Changes in the ovarian follicle are depicted. The relative thickness of the endometrium is also shown.
QUESTION: Which hormone triggers ovulation? What else does this hormone do to the follicle?
Notice first the four hormones involved: FSH and LH from the anterior pituitary gland, estrogen from the ovarian follicle, and progesterone from the cor-pus luteum. The fluctuations of these hormones are shown as they would occur in an average 28-day cycle. A cycle may be described in terms of three phases: menstrual phase, follicular phase, and luteal phase.
Menstrual phase—The loss of the functional layer of the endometrium is called menstruation or the menses. Although this is actually the end of a menstrual cycle, the onset of menstruation is eas-ily pinpointed and is, therefore, a useful starting point. Menstruation may last 2 to 8 days, with an average of 3 to 6 days. At this time, secretion of FSH is increasing, and several ovarian follicles begin to develop.
Follicular phase—FSH stimulates growth of ovarian follicles and secretion of estrogen by the follicle cells. The secretion of LH is also in-creasing, but more slowly. FSH and estrogen pro-mote the growth and maturation of the ovum, and estrogen stimulates the growth of blood vessels in the endometrium to regenerate the functional layer.
This phase ends with ovulation, when a sharp increase in LH causes rupture of a mature ovarian follicle.
Luteal phase—Under the influence of LH, the ruptured follicle becomes the corpus luteum and begins to secrete progesterone as well as estrogen. Progesterone stimulates further growth of blood vessels in the functional layer of the endometrium and promotes the storage of nutrients such as glycogen.
As progesterone secretion increases, LH secre-tion decreases, and if the ovum is not fertilized, the secretion of progesterone also begins to decrease. Without progesterone, the endometrium cannot be maintained and begins to slough off in menstrua-tion. FSH secretion begins to increase (as estrogen and progesterone decrease), and the cycle begins again.
Also secreted by the corpus luteum during a cycle are the hormones inhibin and relaxin. Inhibin inhibits the secretion of FSH, and perhaps LH as well, from the anterior pituitary gland. Relaxin is believed to inhibit contractions of the myometrium (as does pro-gesterone), which would help make implantation of the early embryo successful.
The 28-day cycle shown in Fig. 20–9 is average. Women may have cycles of anywhere from 23 to 35 days, the normal range. Women who engage in stren-uous exercise over prolonged periods of time may experience amenorrhea, that is, cessation of menses. This seems to be related to reduction of body fat. Apparently the reproductive cycle ceases if a woman does not have sufficient reserves of energy for herself and a developing fetus. The exact mechanism by which this happens is not completely understood at present. Amenorrhea may also accom-pany states of physical or emotional stress, anorexia nervosa, or various endocrine disorders.
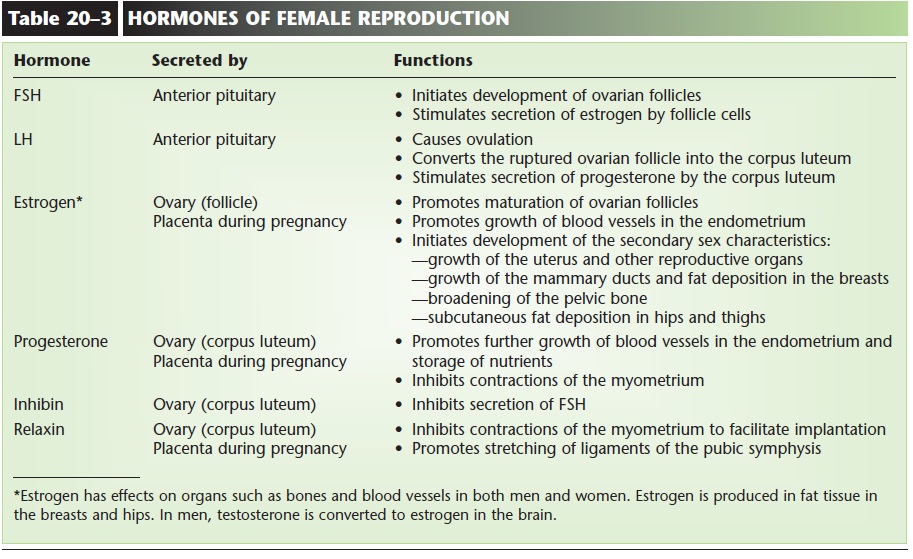
The functions of the hormones of female repro-duction are summarized in Table 20–3.
Related Topics