Chapter: Basic Radiology : Radiology of the Urinary Tract
Exercise: Hematuria
EXERCISE 9-4.
HEMATURIA
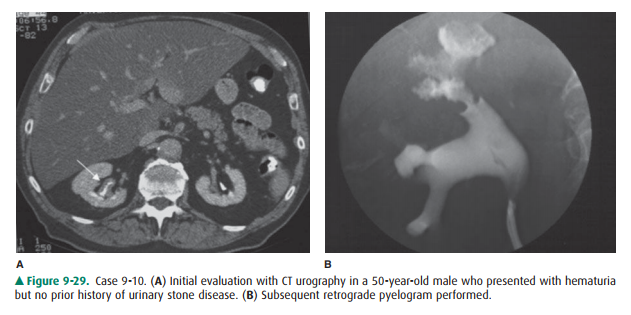
9-10. Based on the two
images from Case 9-10 (Figure 9-29), what is the most likely diagnosis?
A.
Squamous cell carcinoma
B.
Renal stone
C.
Urothelial cell carcinoma
D.
Blood clot
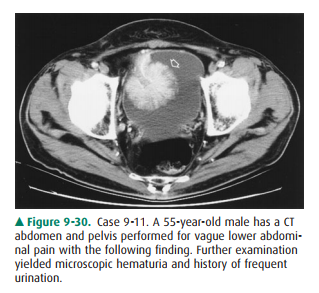
9-11. What would be the
recommended next step in the evaluation and management of the lesion in Case
9-11 (Figure 9-30)?
A.
Cystoscopy
B.
Retrograde cystogram
C.
PET/CT
D.
MRI
Radiographic Findings
In Case 9-10, the first image
from the excretory phase of a CT urogram (Figure 9-29 A) shows thickening of
the mucosal surface (arrow) of the right renal pelvis, compared to the
con-tralateral kidney where the wall is imperceptibly thin. On the retrograde
pyelogram (Figure 9-29B), the upper pole calyces are irregular in contour,
having a “moth-eaten” appearance.
Blood clots are typically
intraluminal filling defects (D is incorrect). Although squamous cell carcinoma
is a differen-tial consideration, this is much less common than urothelial cell
carcinoma. Additionally, clots often are associated with calcifications and
recurrent infections (A is incorrect). This lesion is highly suggestive of
urothelial cell carcinoma, the most common malignancy of the urinary collecting
tract and bladder (C is the correct answer to Question 9-10). Therefore,
further urologic evaluation with cystoscopy and ureteroscopy is recommended.
Regarding the patient in Case
9-11, the image taken from a CT scan (Figure 9-30) of the pelvis shows an
en-hancing, pedunculated mass (arrow) arising from the ante-rior wall of the
urinary bladder. A retrograde cystogram would effectively demonstrate the
presence of a bladder mass, but would do little to narrow the differential (B
is in-correct). PET/CT can prove useful for the detection of metastatic
disease, but is of limited use for evaluating a pri-mary uroepithelial neoplasm
because of the presence of FDG in the excreted urine, which can mask lesion
uptake (C is incorrect). MRI is coming into use to establish depth of invasion
into the bladder wall, but this would be at the dis-cretion of the surgical
oncologist following the establish-ment of a diagnosis. The gold standard for
evaluation of a known bladder mass is cystoscopy (A is the correct answer to
Question 9-11), which allows direct visualization and biopsy for a definitive
diagnosis.
Discussion
Urothelial cell carcinoma
(formally known as transitional cell carcinoma or TCC) is the most common
neoplasm of the urinary tract, and up to 90% of all neoplasms of the bladder
itself. Although TCCs can occur anywhere that there is tran-sitional
epithelium, from the renal collecting system to the urethra, they are most
commonly found in the urinary blad-der. This is felt to be due to several
factors, including the large surface area of the bladder. Also, because the
bladder acts as a temporary storage site prior to excretion, carcinogens remain
in contact with the epithelium of the bladder for a longer period of time than
they do with that of the remainder of the urinary tract. TCC is associated with
numerous chemical car-cinogens as well as cigarette smoking. Bladder urothelial
cell carcinoma usually initially presents with hematuria, which is most
commonly microscopic. A TCC can obstruct the vesi-coureteral junction and cause
obstructive symptoms as well. TCC of the bladder spreads by local invasion and
by lym-phatic and hematogenous spread. Most TCCs are superficial at
presentation, with only about 1 in 4 displaying muscle in-vasion and 1 in 20
having distant metastases at the time of diagnosis.
Plain films are most often
unremarkable in urothelial carcinoma of the bladder, with less than 1%
displaying some stippled calcifications. TCCs can be seen as filling defects in
a contrast-filled bladder, particularly when greater than 1 cm in size. Filling
defects within the bladder on cystography are somewhat nonspecific, with
considerations including tumor, radiolucent stones, fungus balls, and blood
clots. However, transitional cell cancers have a characteristic stippled and
frondlike appearance. Ultrasound can show ex-ophytic soft-tissue lesion within
the bladder. CT urography is the imaging modality of choice for evaluation of
possible bladder masses, because the size of the mass itself, as well as the
extent of invasion through the bladder wall into adjacent pelvic structures,
can be evaluated. The use of urographic phase imaging and reformats allows the
detection of even small, sessile lesions in the bladder, ureters, or renal
pelvis. CT also allows evaluation of abdominal and pelvic lymph nodes and
posttreatment examination for tumor recurrence. MRI can assess depth of bladder
tumor invasion, but is not currently routinely used in tumor staging. Although
the foregoing imaging findings strongly suggest the diagnosis of TCC,
cystoscopy is important to confirm the histologic di-agnosis. Cystoscopy is
also indicated when CT urography does not demonstrate a source for hematuria.
Other less common tumors of the bladder include malignancies such as squamous
cell carcinoma and adenocarcinoma, uncom-mon benign lesions, and some masslike
manifestations of inflammatory processes.
Related Topics