Chapter: Basic Radiology : Radiology of the Urinary Tract
Exercise: Adrenal Masses
EXERCISE 9-1.
ADRENAL MASSES
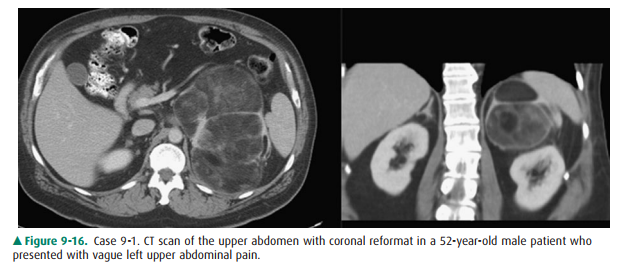
9-1. In Case 9-1 (Figure
9-16), the most likely diagnosis is
A.
adrenal metastasis.
B.
renal angiomyolipoma.
C.
adrenal myelolipoma.
D.
retroperitoneal liposarcoma.
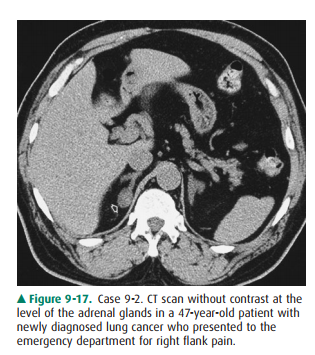
9-2. Regarding Case 9-2
(Figure 9-17), in a patient with a primary neoplasm elsewhere, the most common
ad-renal mass is
A.
metastasis.
B.
adenoma.
C.
adrenal carcinoma.
D.
acute adrenal hemorrhage.
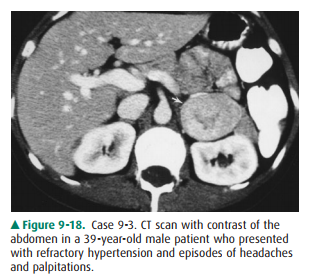
9-3. In Case 9-3 (Figure
9-18), the most likely diagnosis is
A.
pheochromocytoma.
B.
metastasis.
C.
adrenal cyst.
D.
adrenal lymphoma.
Radiologic Findings
In Case 9-1 (Figure 9-16), a
10-cm mass in the left upper ab-domen contains areas of macroscopic fat. The
mass lies just medial to the spleen and on coronal images is separated from the
kidney by a plane of retroperitoneal fat (B is incorrect). Although subtle, the
thin rim of tissue surrounding the lesion demarcates the mass and
differentiates it from normal adjacent retroperitoneal fat. The fatty nature of
the lesions is confirmed by the low-density tissue within the mass, similar to
that of adjacent normal retroperitoneal and subcutaneous fat. Fat is rare
within adrenal metastasis (A is incorrect). Although the retroperitoneal
sarcoma is a differential consideration for a heterogenous retroperitoneal
fatty mass, the location of the lesion and commonality of myelolipoma make
adrenalmyelolipoma the most likely diagnosis (C is the correct answer to
Question 9-1).
Regarding Case 9-2 (Figure 9-17),
the diagnosis or exclusion of metastatic adrenal disease is one of the most
important is-sues facing the radiologist in daily practice. The diagnosis of
metastatic disease allows appropriate therapy for the patient including the
possible prevention of unnecessary surgery. Perhaps more importantly,
misdiagnosing a benign lesion as metastatic disease may mistakenly prevent
potentially curative therapies such as surgery. In Case 9-2, there is a small
2-cm homogeneous mass arising from the medial limb of the adrenal gland. Recall
that the density of a lesion can be quantitated on CT with Hounsfield unit
measurements (although not shown, the Hounsfield unit measurements of the mass
was 8 HU). Acute adrenal hematomas are high-density masses on non-contrast CT
scan measuring between 50 and 90 Hounsfield units (D is incorrect). Adrenal
carcinomas are typically large heterogeneous lesions and are quite rare (C is
incorrect). The distinction between adrenal metastasis and adenoma is a
crit-ical one. Although there can be overlap in their appearances, certain
imaging characteristics of adrenal adenomas allow a confident diagnosis in the
vast majority of cases, as we see later. Even with a known primary malignancy,
however, statisti-cally the most likely etiology of a small adrenal mass is
benign adrenal adenoma (B is the correct answer to Question 9-2). There are
methods to more confidently differentiate ade-noma from metastasis which are
covered later.
Case 9-3 (Figure 9-18) demonstrates a 4-cm solid appearing just anterior to the left kidney. Note the fat plane that clearly shows that the mass does not arise from the kidney. No specific characteristics such as fat are seen. The lesion is denser than sur-rounding muscle, making a cyst unlikely (C is incorrect). Adrenal lymphoma is typically bilateral, usually shows diffuseenlargement of the adrenal glands, and is typically accompa-nied by retroperitoneal adenopathy (D is incorrect). Although metastatic disease can have variable appearances and cannot be radiographically excluded, the lesion is also typical for a pheochromocytoma and, given the clinical history, this is the most likely diagnosis (A is the correct answer to Question 9-3).
Discussion
The adrenal mass is a common
problem for the radiologist and is being incidentally diagnosed with greater
frequency with the increased utilization of cross-sectional imaging techniques,
especially CT and MRI. In fact, the term “adrenal incidentaloma” has been
coined for the small adrenal mass identified on imaging studies obtained for
other reasons. Although there are many causes of adrenal masses, the most
common include benign adenomas, metastatic disease, adre-nal carcinoma, and
myelolipomas.
The most common adrenal mass is
the adrenal adenoma. Although they can be hyperfunctioning and result in
clinical syndromes, the majority of adrenal adenomas are nonhyper-functioning
and are diagnosed incidentally. Distinguishing these “incidentalomas” from more
significant pathology is critical. Fortunately, most adenomas have specific
character-istics that allow a confident diagnosis. Many adenomas are similar to
normal adrenal cortical tissue in that they contain a high proportion of
cellular lipid material. This results in a low-density appearance and
Hounsfield measurements on unenhanced CT that are highly specific for adenoma.
Certain adenomas have a paucity of lipid, however, and may be oth-erwise
differentiated from other masses by their enhance-ment characteristics.
Specifically, contrast enhancement is rapidly lost in adenomas on delayed
images, a phenomenon known as “washout.” MRI can be used to demonstrate
lipid-rich adenomas by using special imaging sequences that reveal
intracellular lipid. MRI is no better than CT for demonstrat-ing the
characteristic washout of the adenoma. Given the widespread availability and
reliability of CT, CT remains the primary modality for evaluating a nonspecific
adrenal lesion.
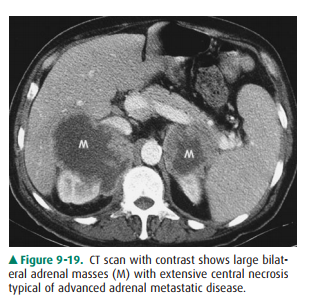
The adrenal gland is a common
site of metastatic disease, with breast and lung being the most common sources.
The im-aging characteristics of metastatic disease are quite variable. Lesions
may be unilateral or bilateral, homogeneous or hetero-geneous in appearance
(Figure 9-19). The larger the metastatic lesion, generally, the more necrosis
and hemorrhage and the more heterogeneous the lesion appears. Smaller lesions
tend to be more uniform. Fortunately, unlike adenomas, metastatic disease does
not contain high intracellular lipid and thus does not show the lipid-type
imaging changes that characterize ade-nomas. However, metastatic disease can be
indistinguishable from other adrenal pathology and histologic confirmation with
biopsy may be necessary.
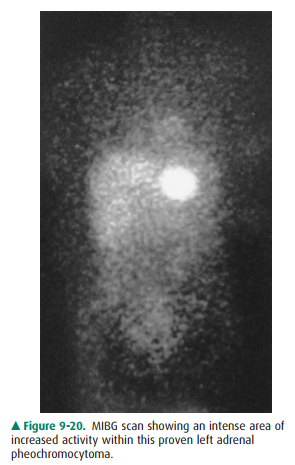
Pheochromocytomas are an unusual
catecholamine-producing tumor arising from the sympathetic innervation of the
adrenal gland most commonly originating in the adre-nal medulla, although in
10% of cases they may arise in an ex-traadrenal location. Most tumors arise
sporadically, although a small percentage occur in certain syndromes. Most
pheo-chromocytomas produce a constellation of symptoms referable to their
catecholamine production, including hypertension and episodic headaches and
palpitations. Most pheochromocy-tomas appear as a nonspecific adrenal mass on CT.
Many of these lesions are fairly homogeneous solid masses. However, necrosis,
calcification, and cystic formation all occur. On MRI, the diagnosis may be
suggested by the fairly specific finding of very bright adrenal mass on
T2-weighted images. Finally, MIBG, which collects in adrenal medullary-type
tissue, can provide important information about these tumors. Although they may
be used to confirm the diagnosis of a suspected ad-renal pheochromocytoma, a
more important role for MIBG imaging is in the evaluation of metastatic disease
or recurrent tumor, or for the localization of extraadrenal lesions. The MIBG
scan typically shows a brightly intense area of activity at the site of the
lesion (Figure 9-20).
Related Topics