Chapter: Biology of Disease: Disorders of Water, Electrolytes and Urate Balances
Disorders of Water Homeostasis
DISORDERS OF WATER HOMEOSTASIS
Water is necessary to maintain the volumes of body
compartments, for excretion of waste products and as a medium in which
biochemical reactions occur. Water intake is variable and can depend, to some
extent, on social habits but is supplied in the diet, from food as well as
water and as a product of oxidative metabolism. Its loss is variable although
an almost fixed amount, called the insensible loss, occurs from the GIT, skin
and lungs. An average 70 kg man has 42 dm3 of water distributed
between various body compartments (Figure
8.4). Water accounts for 60% of body weight in men but only 55% in women
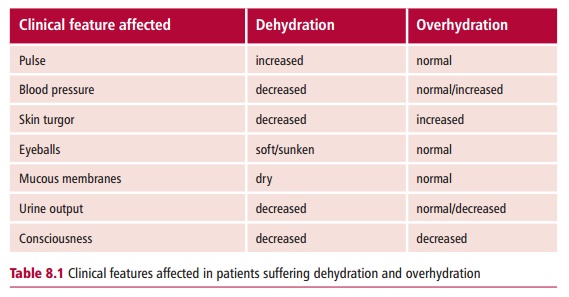
given they have a higher proportion of fat. In disease, patients can be dehydrated, where water loss caused by
vomiting and diarrhea exceeds gain,or overhydrated,
with an accumulation of water in body compartments. The clinical features of
dehydration and over hydration are listed in Table 8.1. A reduced extracellular fluid (ECF) volume causes a
decline in blood circulation with decreased excretion of wastes and reduced
oxygen and nutrient supply to the cells. Humans deprived of fluid intake die
after a few days because the reduced total body fluid leads to a circulatory
collapse.
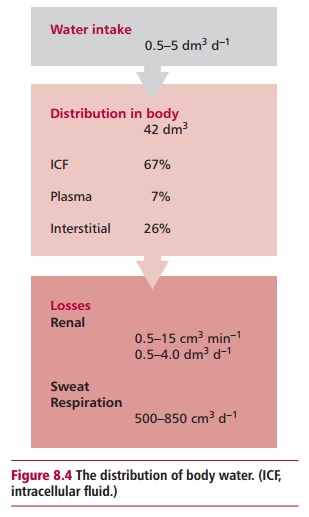
The kidneys regulate water balance by varying the output of
urine from 0.5 to 15 cm3 min–1 to match water intake.
When there is an excess of water, the kidneys lose water rapidly but in times
of shortage it is conserved. The total body water is therefore kept constant.
Water loss from the kidneys can be regulated by the hormone arginine
vasopressin also called antidiuretic hormone (ADH). Antidiuretic hormone acts
by altering the permeability to water of the collecting ducts in the kidneys.
Osmoreceptor cells in the hypothalamus detect an increase or decrease in
osmolality between the intracellular fluid (ICF) and ECF. An increase in the
osmolality of the ECF stimulates the receptors and these, in turn, stimulate
the release of ADH from the posterior pituitary gland . Antidiuretic hormone
then stimulates the kidneys to retain water and produce a more concentrated urine.
The retention of water helps return the osmolality of the ECF back to normal.
If the osmolality of the ECF is low, the osmoreceptors are not stimulated and
ADH is not released. This results in water loss from the kidneys in dilute
urine. The loss of water helps to increase the osmolality of the ECF back to
normal values. A low blood or ECF volume can be detected by baroreceptors in
the aortic arch and carotid sinus . These receptors also stimulate a release of
ADH and, indeed, this mechanism can override the release of ADH by osmolality
to maintain blood volume and therefore circulation. Antidiuretic hormone
interacts with a second hormone, aldosterone to maintain the normal volume and
concentration of the ECF. Aldosterone, a steroid hormone, is produced by the
adrenal cortex and released in response to a low ECF volume or blood pressure.
It stimulates retention of Na+ together with water in the kidneys
returning the ECF volume back to normal.
There are distinctive signs and symptoms associated with loss of
water from body compartments. For example, loss of water from the ICF results
in cell dysfunction that presents clinically as confusion, lethargy and coma.
Loss of water from the ECF decreases blood pressure, leading to renal shutdown
and shock. A reduction in total body water (ICF and ECF) produces a combination
of both effects.
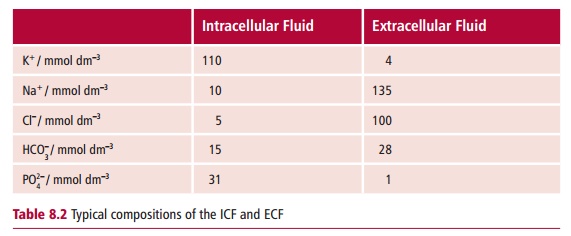
All body fluids contain electrolytes (Table 8.2). The regulation of water content by ADH helps to
maintain normal electrolyte concentrations within the body. The concentration
of Na+ and K+ in the ICF and ECF are maintained largely
by the activity of the plasma membrane Na+/K+-ATPase .
This enzyme acts as an energy-dependent pump that expels Na+ from
the cell in exchange for an intake of K+ to maintain both at
physiological concentrations. The concentrations of these ions are maintained
within narrow ranges and, since water can flow freely through most membranes,
the concentrations of Na+ and K+ are responsible for maintaining
the appropriate osmolalities of these compartments. The movement of water from
one compartment to another is mainly responsible for determining their volumes.
Homeostatic mechanisms exist to minimize changes in
body water and electrolyte composition and are particularly important in
maintaining the
The assessment of fluid and electrolyte disorders in
patients is a significant workload in the hospital pathology laboratory. In
most cases, clinical tests to determine the concentrations of electrolytes in
blood must be interpreted in conjunction with a clinical examination which
involves taking the patient’s clinical history, looking for signs and symptoms
of hydration or dehydration and assessing kidney function.
Related Topics