Chapter: Biology of Disease: Disorders of Water, Electrolytes and Urate Balances
Disorders of Na+ Homeostasis
DISORDERS OF Na+
HOMEOSTASIS
Sodium ions are significant constituents of tissues, including
bone, they control the volume of ECF and are required for normal neuromuscular
functions. The intake of Na+ is variable, from less than 100 mmol to
more than 300 mmol day–1. Losses are also variable, but renal loss
is normally matched to intake. Small amounts of Na+ are lost via
skin and in feces and, under some circumstances, the GIT can be a major route
of Na+ loss, as in diarrhea.
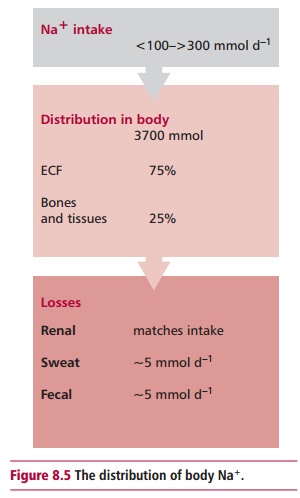
The average 70 kg man contains 3700 mmol of Na+ (Figure 8.5), of which 75% is found in
the ECF. Hyponatremia and hypernatremia refer to serum concentrations of Na+
below and above the reference range of 135–145 mmol dm–3.
Hyponatremia is caused by an excessive retention of water or the loss of Na+,
these two conditions resulting in different clinical features. The retention of
water produces behavioral disturbances, headaches, confusion, convulsions and
eventually coma. The symptoms associated with excessive loss of Na+
are weakness, apathy, dizziness, weight loss and hypotension. Hyponatremia due
to water retention is the more common. Water may be retained with or without an
increase in total body Na+. The former produces an edema, giving an edematous
hyponatremia, whereas the latter results in nonedematous hyponatremia.
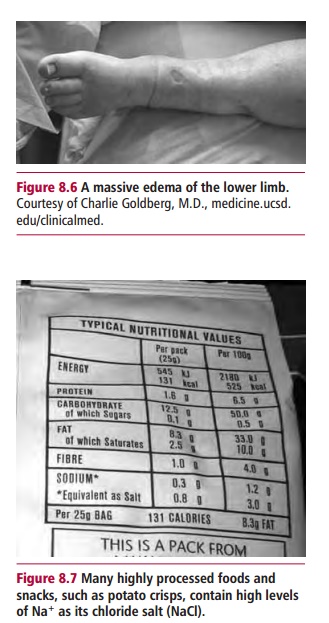
Edema is the excessive accumulation of fluid in interstitial
compartments of the body, resulting from an increase in the concentration of Na+
in the ECF. It results in swelling, which may be localized in, for example,
legs and ankles (Figure 8.6) but can
be more general in the chest cavity, abdomen and lungs. The major causes of
edematous hyponatremia are heart failure, nephrotic syndrome and liver disease.
All three reduce blood volume and stimulate aldosterone secretion, which, in
turn, stimulates the retention of Na+. The reduced blood volume also
stimulates release of ADH from the posterior pituitary. Both result in more
water than Na+ being retained, giving rise to hyponatremia.
Nephrotic syndrome leads to a loss of blood proteins to the urine, reduced
concentrations of albumin leading to edema. The commonest cause of nephrotic
syndrome is renal damage by diseases such as glomerulonephritis . The treatment
of edematous hyponatremia is aimed at its underlying cause, for example heart
failure, kidney or liver diseases, and at removing the excess water and Na+
using diuretics, and restricting water intake.
Nonedematous hyponatremia, the result of water overload without
an increase in total body Na+, is due to a decreased excretion of
water from the syndrome of inappropriate secretion of ADH (SIADH), a severe
renal failure or an increased intake by compulsive drinking or excessive
parenteral fluid. The SIADH is a common finding in clinical practice. Patients
present with reduced plasma osmolality, normal kidney function and a low output
of urine. This syndrome is associated with many conditions, including malignancies,
for example carcinoma of the lungs or bowel , infections, such as pneumonia and
tuberculosis , trauma following, for example abdominal surgery, or it may be
induced with drugs, such as chlorpropamide. All these conditions result in
SIADH with water retention and a low urinary output. The excessive water is
distributed between ICF and ECF and so the clinical signs of water overload,
edema, may be mild or absent. Treatment of SIADH is to reduce water intake to
less than 750 cm3 day–1 and to correct its underlying
cause.
Hyponatremia from loss of Na+ decreases the total
body Na+ of patients. The losses may occur from vomiting, diarrhea,
kidneys (aldosterone deficiency), the effects of drugs, such as spironolactone,
or a decreased dietary intake of Na+, although this is very rare.
The loss of Na+ is always accompanied by water loss; as the volume
of the ECF decreases the release of ADH is stimulated and the increased
reabsorption of water produces hyponatremia. The decreased volume of ECF means
that the patient presents with the clinical symptoms of dehydration. Treatment
is aimed at correcting the Na+ losses with intravenous infusions of
0.9% NaCl, and treating the underlying cause, for example steroid therapy for
aldosterone deficiency as in Addison’s disease .
Hypernatremia is caused by water depletion, water and Na+
depletion with the loss of water predominating, or to an excess of Na+
(Figure 8.7). Its clinical features
are variable but, in general, patients present with muscular weakness,
hypertension, intense thirst (polydipsia)
and polyuria. If fluid loss occurs, the features associated with dehydration
may be present. However, if Na+ is in excess, raised blood pressure
or edema may be seen.
Water depletion results from a decreased intake, such as in
comatose patients, infants or the elderly. The body conserves water by
producing a low volume of concentrated urine. Increased water losses can also
occur in diseases such as diabetes insipidus that result in large quantities of
dilute urine . Hypernatremia with water and Na+ depletion occurs
only if relatively more water than Na+ is lost. It is commonly
caused in children by excessive sweating or diarrhea. Patients respond by
producing low volumes of concentrated urine. The condition may also occur
during osmotic diuresis in patients with diabetes mellitus where both water and
Na+ are lost, together with other electrolytes in large volumes of
dilute urine, producing hypernatremia and a decreased ECF. An excess of Na+in
the ECF is caused by an increased intake or decreased excretion of Na+.
The intake may be oral, for example salt tablets or seawater, or parenteral as
in the treatment of Conn’s or Cushing’s syndromes . Both disorders produce
dilute urine due to retention of Na+ by the kidneys.
Hypernatremia is treated by oral administration of water. If
this is not possible, then 5% dextrose is administered parenterally. If
hypernatremia is due to an excessive Na+ intake, measures to remove
it must be considered.
Related Topics