Chapter: Essentials of Psychiatry: Delirium and Dementia
Dementia Due to HIV Diseases
Dementia Due to HIV Diseases
Initially, the behavioral abnormalities observed in
HIV-positive patients were attributed to the emotional reaction to the disease.
Subsequent investigations demonstrated that neurological com-plications occur
in 40 to 45% of patients with AIDS, and in about 10% of cases neurological
signs are the first feature of the disease (Berg et al., 1994). The neurological signs present in AIDS are believed
to be related to both the direct effects of the virus on cells (such as
macrophages) that enter the central nervous system and the neurological
conditions that opportunistically affect these patients. Ho and colleagues
(1987) reported that 90% of the brains of AIDS patients examined showed
neuropathological abnormalities. AIDS dementia must be considered in the
differ-ential diagnosis of dementia in older patients, because about 10% of
AIDS patients are older than 50 years of age.
Patients with AIDS dementia present with
impairments of cognitive, behavioral and motor systems. The cognitive disorders
include memory impairment, confusion and poor concentration. Behavioral
features include apathy, reclusivity, anhedonia, de-pression, delusions, and
hallucinations. Motor symptoms include incoordination, lower extremity paresis,
unsteadiness, and diffi-culty with fine motor movements like handwriting and
buttoning clothes. As the disease progresses, parkinsonism and myoclonus
develop.
Localizing signs such as tremors, focal seizures,
abnormal reflexes and hemiparesis can result. The protozoan Toxoplasma gondii commonly infects the central nervous system and can be diagnosed by CT or by increased
toxoplasmosis antibody titers. Discrete cerebral lesions are also produced by
fungi such as Can-dida and Aspergillus, Mycobacterium tuberculosis, and viruses such as cytomegalovirus and papovavirus. Papovavirus causes
progressive multifocal leukoencephalopathy. Tertiary syphilis has increased
significantly since the advent of AIDS, and neo-plasms such as lymphomas,
metastatic Kaposi’s sarcoma and gliomas are also causes of AIDS dementia.
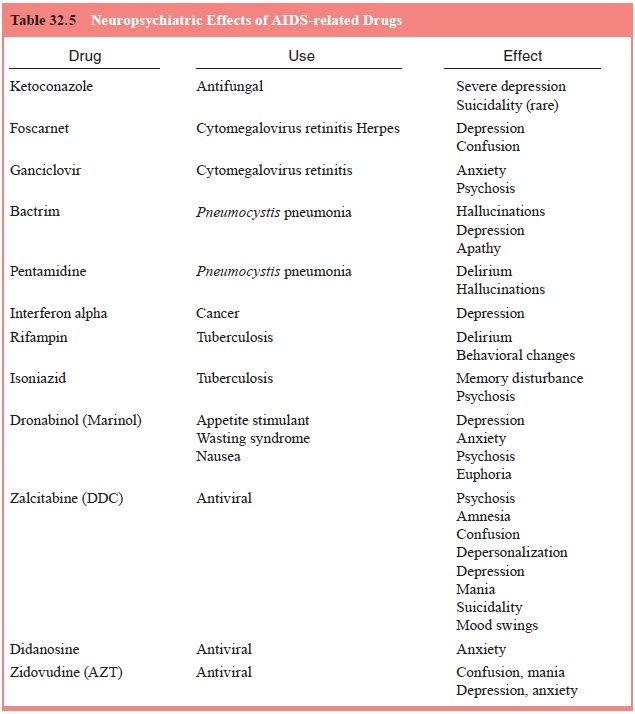
Many confounding factors can increase cognitive
dys-function in AIDS, including a high incidence of drug and alcohol abuse;
medications such as histamine H2 receptor antagonists (cimetidine),
corticosteroids, narcotics and antiviral drugs (e.g., zidovudine [formerly
azidothymidine, AZT]) that increase con-fusion; and coexistent depression
(Table 32.5).
The CT scan shows cerebral atrophy and MRI reveals
nonspecific white matter abnormalities (Kaufman, 1990b). Neo-plasms and lesions
such as toxoplasmosis are also visible. Lum-bar puncture reveals a pleocytosis
and elevated protein levels, and autopsy demonstrates an atrophic brain with
demyelina-tion, multinuclear giant cells and gliosis of the cerebral cortex
(Kaufman, 1990b).
Treatment
The increase in life span of patients affected by HIV is directly related to improvements in treating the opportunistic conditions that occur. Aerosol pentamidine as prophylaxis for P. carinii pneumonia and ganciclovir for cytomegalovirus retinitis are ex-amples of effective intervention. The use of antiviral agents has generated some controversy. Zidovudine, the first antiviral treat-ment for AIDS approved by the USFDA, increased or stabilized CD41 cell concentrations in early studies. Later investigations revealed that zidovudine has a narrow window of effectiveness and may not be appropriate immediately after such exposure as a needle stick. Side effects of zidovudine include blood dyscrasias, peripheral neuropathy, seizures, lymphomas, confusion, anxi-ety, mania and a Wernicke–Korsakoff type of picture (Kaufman, 1990b).
Studies suggest that administration of zidovudine
to HIV-positive patients during pregnancy, intravenously during deliv-ery, and
to the neonate for 6 weeks after birth can decrease the percentage of infants
who seroconvert from 30% to as low as 10%. However, results of studies of the
effectiveness of zidovu-dine in children already HIV-positive have been
disappointing. Subsequent antiviral agents such as dideoxyinosine and
dideoxy-cytidine (DDC) have been associated with painful neuropathy and
pancreatic disorders. DDC in particular can produce seri-ous neuropsychiatric
complications. Combined therapy with two antiviral agents may be more effective
than single-drug therapy. Many pharmaceutical companies are combining two
antivirals into a single pill, and the development of protease inhibitor agents
such as indinavir and nelfinavir have been especially effective in retarding
the progression of the disease. The treat-ment of neuropsychiatric disorders in
AIDS involves utilizing agents that are least likely to interfere with other
medications prescribed, or to exacerbate the symptoms of the disease.
AIDS-related depression has responded well to the selective serotonin reuptake
inhibitors (SSRIs) and to psychostimulants. Some HIV drugs can have
interactions with SSRIs, particularly ritonavir and the SSRIs themselves,
especially paroxetine and fluoxetine can interact with other agents the HIV
patient may have been prescribed, such as antiarrhythmics, benzodiazepines and
anti-convulsants by inhibiting the cytochrome P-450 enzyme system. Some
individuals have suggested that citalopram is less likely to inhibit this
enzyme system. Careful attention to drug–drug interactions, using lower
starting doses of certain psychiatric drugs, and monitoring of blood levels of
affected medications are recommended. Among the psychostimulants, methylphenidate
is preferred to dextroamphetamine because of the latter’s tendency to produce
dyskinesias. Use of stimulants for treating patients with a history of
substance abuse is not recommended. Antichol-ingeric agents have a number of
side effects such as mydriasis, decreased gastrointestinal motility and
postural hypotension. However, low dose tricyclic antidepressants are often
used for their sedative, analgesic and appetite stimulant properties. Most
antidepressants and some mood stabilizers and antipsychotics can cause bone
marrow suppression so they should be used with care, and hematologic parameters
routinely monitored. Lithium carbonate, which produces a leukocytosis, may be
of benefit in recurrent unipolar and treatment resistant depression, but may
potentiate AIDS-related diarrhea. Many of the drugs used to treat AIDS-related
conditions may produce untoward psychiatric ef-fects. Depression has been well
documented as a side effect of indinavir and nelfinavir has been associated
with anxiety, de-pression, mood lability and even suicidality. St John’s Wort
may decrease the concentration of many of the protease inhibitors and is
therefore contraindicated in patients taking these agents. In summary, AIDS
dementia is best treated by identifying the as-sociated medical condition,
instituting appropriate therapy and managing behavior in the interim.
Related Topics