Chapter: Essentials of Psychiatry: Delirium and Dementia
Delirium
Delirium
Delirium (also known as acute confusional state,
toxic metabolic encephalopathy) is the behavioral response to widespread
distur-bances in cerebral metabolism. Like dementia, delirium is not a disease
but a syndrome with many possible causes that result in a similar constellation
of symptoms. DSM-IV-TR describes five categories of delirium based on etiology.
These include delirium due to a general medical condition, substance
intoxication, with-drawl delirium, delirium due to muttiple etiologies and
delirium not otherwise specified.
Epidemiology
The overall prevalence of delirium in the community
is low, but delirium is common in hospitalized patients. Lipowski (Saito, 1987)
reported studies of elderly patients and suggested that about 40% of them
admitted to general medical wards showed signs of delirium at some point during
the hospitalization. Because of the increasing numbers of elderly in this
country and the influence of life-extending technology, the population of
hospitalized elderly is rising; and so is the prevalence of delirium. The
intensive care unit, geriatric psychiatry ward, emergency department, alcohol
treatment units and oncology wards have particularly high rates of delirium.
Massie and colleagues (Lipowski, 1987) reported that 85% of terminally ill
patients studied had symptoms that met criteria for delirium, as did 100% of
postcardiotomy patients in a study by Theobald (Lipowski, 1989). Overall, it is
estimated that 10% of hospitalized patients are delirious at any particular
point in time.
Predisposing factors in the development of delirium in-clude old age, young age (children), previous brain damage, prior episodes of delirium, malnutrition, sensory impairment (espe-cially vision) and alcohol dependence. In general, the mortality and morbidity of any serious disease are doubled if delirium en-sues. The risk of dying after a delirious episode is greatest in the first two years after the illness, with a higher risk of death from heart disease and cancer in women and from pneumonia in men. Overall, the 3-month mortality rate for persons who have an epi-sode of delirium is about 28%, and the 1-year mortality rate for such patients may be as high as 50%.
Pathophysiology
ACh is the primary neurotransmitter believed to be
involved in delirium, and the primary neuroanatomical site involved is the
reticular formation. Thus, one of the frequent causes of delirium is the use of
drugs with high anticholingeric potential. As the principal site of regulation
of arousal and attention, the reticular formation and its neuroanatomical
connections play a major role in the symptoms of delirium. The major pathway
involved in de-lirium is the dorsal tegmental pathway projecting from the
mes-encephalic reticular formation to the tectum and the thalamus.
Clinical Features
According to DSM-IV-TR, the primary feature of
delirium is a diminished clarity of awareness of the environment (American
Psychiatric Association, 1994). Symptoms of delirium are char-acteristically
global, of acute onset, fluctuating and of relatively brief duration. In most
cases of delirium, an often overlooked pro-drome of altered sleep patterns,
unexplained fatigue, fluctuating mood, sleep phobia, restlessness, anxiety and
nightmares occurs. A review of nursing notes for the days before the recognized
onset of delirium often illustrates early warning signs of the condition.
Several investigators have divided the clinical
features of delirium into abnormalities of 1) arousal, 2) language and
cognition, 3) perception, 4) orientation, 5) mood, 6) sleep and wake-fulness,
and 7) neurological functioning (Kaplan et
al., 1994
The state of arousal in delirious patients may be
increased or decreased. Some patients exhibit marked restlessness, height-ened
startle, hypervigilance and increased alertness. This pattern is often seen in
states of withdrawal from depressive substances (e.g., alcohol) or intoxication
by stimulants (phencyclidine, am-phetamine, lysergic acid diethylamide).
Patients with increased arousal often have such concomitant autonomic signs as
pallor, sweating, tachycardia, mydriasis, hyperthermia, piloerection and
gastrointestinal distress. These patients often require seda-tion with
neuroleptics or benzodiazepines. Hypoactive arousal states such as those
occasionally seen in hepatic encephalopathy and hypercapnia are often initially
perceived as depressed or de-mented states. The clinical course of delirium in
any particular patient may include both increased and decreased arousal states.
Many such individuals display daytime sedation with nocturnal agitation and
behavioral problems (sundowning).
Perceptual abnormalities in delirium represent an inability to discriminate sensory stimuli and to integrate current percep-tions with past experiences. Consequently, patients tend to per-sonalize events, conversations and so forth that do not directly pertain to them, become obsessed with irrelevant stimuli and misinterpret objects in their environment. The misinterpreta-tions generally take the form of auditory and visual illusions. Patients with auditory illusions, for example, might hear the sound of leaves rustling and perceive it as someone whispering about them. Paranoia and sleep phobia may result. Typical visual illusions are that intravenous tubing is a snake or worm crawling into the skin, or that a respirator is a truck or farm vehicle about to collide with the patient. The former auditory illusion may lead to tactile hallucinations, but the most common hallucinations in delirium are visual and auditory.
Orientation is often abnormal in delirium.
Disorientation in particular seems to follow a fluctuating course, with
patients unable to answer questions about orientation in the morning, yet fully
oriented by the afternoon. Orientation to time, place, person and situation
should be evaluated in the delirious patient. Gener-ally, orientation to time
is the sphere most likely impaired, with orientation to person usually
preserved. Orientation to significant people (parents, children) should also be
tested. Disorientation to self is rare and indicates significant impairment.
The examiner should always reorient patients who do not perform well on any
portion of the orientation testing of the mental status examination, and serial
testing of orientation on subsequent days is important.
Language and Cognition
Patients with delirium frequently have abnormal
production and comprehension of speech. Nonsensical rambling and
incoherentspeech may occur. Other patients may be completely mute. Memory may
be impaired, especially primary and second-ary memory. Remote memory may be
preserved, although the patient may have difficulty distinguishing the present
from the distant past.
Mood
Patients with delirium are susceptible to rapid
fluctuations in mood. Unprovoked anger and rage reactions occasionally occur
and may lead to attacks on hospital staff. Fear is a common emo-tion and may
lead to increased vigilance and an unwillingness to sleep because of increased
vulnerability during somnolence. Apathy, such as that seen in hepatic
encephalopathy, depression, use of certain medications (e.g., sulfamethoxazole
[Bactrim]) and frontal lobe syndromes, is common as is euphoria secondary to
medications (e.g., corticosteroids, DDC, zidovudine) and drugs of abuse
(phencyclidine, inhalants).
Neurological Symptoms
Neurological symptoms often occur in delirium.
These include dysphagia as seen after a CVA, tremor, asterixis (hepatic
en-cephalopathy, hypoxia, uremia), poor coordination, gait apraxia, frontal
release signs (grasp, suck), choreiform movements seizures, Babinski’s sign and
dysarthria. Focal neurological signs occur less frequently.
Sleep–Wakefulness Disturbances
Sleeping patterns of delirious patients are usually
abnormal. During the day they can be hypersomnolent, often falling asleep in
midsentence, whereas at night they are combative and restless. Sleep is
generally fragmented, and vivid nightmares are com-mon. Some patients may
become hypervigilant and develop a sleep phobia because of concern that
something untoward may occur while they sleep.
Causes of Delirium
The cause of delirium may lie in intracranial
processes, extrac-ranial ones, or a combination of the two. The most common
etio-logical factors are as follows (Francis et al., 1990).
Infection Induced
Infection is a common cause of delirium in
hospitalized patients and typically, infected patients will display
abnormalities in he-matology and serology. Vital signs are noted except in
persons (elderly, chronic alcohol abusers, chemotherapy patients, those with
HIV spectrum disease) who may not be able to mount the typical response.
Bacteremic septicemia (especially that caused by gram-negative bacteria),
pneumonia, encephalitis and menin-gitis are common offenders. The elderly are
particularly suscep-tible to delirium secondary to urinary tract infections.
Metabolic and Endocrine Disturbances
Metabolic causes of delirium include hypoglycemia,
electro-lyte disturbances and vitamin deficiency states. The most com-mon
endocrine causes are hyperfunction and hypofunction of the thyroid, adrenal,
pancreas, pituitary and parathyroid. Meta-bolic causes may involve consequences
of diseases of particu-lar organs, such as hepatic encephalopathy resulting
from liver disease, uremic encephalopathy and postdialysis delirium re-sulting
from kidney dysfunction, and carbon dioxide macrosis and hypoxia resulting from
lung disease. The metabolic dis-turbance or endocrinopathy must be known to
induce changes in mental status and must be confirmed by laboratory
deter-minations or physical examination, and the temporal course of the
confusion should coincide with the disturbance (Francis et al., 1990). In some
individuals, particularly the elderly, brain
injured and demented, there may be a significant lag time be-tween
correction of metabolic parameters and improvement in mental state.
Low-perfusion States
Any condition that decreases effective cerebral
perfusion can cause delirium. Common offenders are hypovolemia, congestive
heart failure and other causes of decreased stroke volume such as arrhythmias
and anemia, which decreases oxygen binding. Main-tenance of fluid balance and
strict measuring of intake and output are essential in delirious states.
Intracranial Causes
Intracranial causes of delirium include head
trauma, especially involving loss of consciousness, postconcussive states and
hem-orrhage; brain infections; neoplasms; and such vascular abnor-malities as
CVAs, subarachnoid hemorrhage, transient ischemic attacks and hypertensive
encephalopathy.
Postoperative States
Postoperative causes of delirium may include
infection, atel-ectasis, postpump confusion from maintenance on a heart–lung
machine, lingering effects of anesthesia, thrombotic and embolic phenomena, and
adverse reactions to postoperative analgesia. General surgery in an elderly
patient has been reported to be fol-lowed by delirium in 10 to 14% of cases and
may reach 50% after surgery for hip fracture (Lipowski, 1989).
Sensory and Environmental Changes
Many clinicians underestimate the disorienting
potential of an unfamiliar environment. The elderly are especially prone to de-velop
environment-related confusion in the hospital. Individuals with preexisting
dementia, who may have learned to compensate for cognitive deficits at home,
often become delirious once hos-pitalized. In addition, the nature of the
intensive care unit often lends itself to periods of high sensory stimulation
(as during a “code”) or low sensory input, as occurs at night. Often, patients
use such external events as dispensing medication, mealtimes, presence of
housekeeping staff, and physicians’ rounds to mark the passage of time. These
parameters are often absent at night, leading to increased rates of confusion
during night-time hours. Often, manipulating the patient’s environment or
removing the patient from the intensive care unit can be therapeutic.
Substance Intoxication Delirium
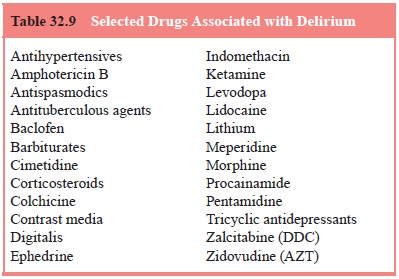
The list of medications that can produce the
delirious state is extensive (Table 32.9). The more common ones include such
antihypertensives as methyldopa and reserpine, histamine (H2)
receptor antagonists (cimetidine), corticosteroids, antide-pressants, narcotics
(especially opioid) and nonsteroidal anal-gesics, lithium carbonate, digitalis,
baclofen, anticonvulsants, antiarrhythmics, colchicine, bronchodilators,
benzodiazepines, sedative-hypnotics and anticholinergics. Of the narcotic
anal-gesics, meperidine can produce an agitated delirium with trem-ors,
seizures and myoclonus. These features are attributed to its active metabolite
normeperidine, which has potent stimulant and anticholingeric properties and
accumulates with repeated intravenous dosing. In general, adverse effects of
narcotics are more common in those who have never received such agents before
(the narcotically naive) or who have a history of a similar response to
narcotics.
Lithium-induced delirium occurs at blood levels
greater than 1.5 mEq/L and is associated with early features of lethargy,
stuttering and muscle fasciculations. The delirium may take as long as 2 weeks
to resolve even after lithium has been discon-tinued, and other neurological signs
such as stupor and seizures commonly occur. Maintenance of fluid and
electrolyte balance is essential in lithium-induced delirium. Facilitation of
excretion with such agents as aminophylline and acetazolamide helps, but
hemodialysis is often required.
Principles to remember in cases of drug-induced
delirium include the facts that 1) blood levels of possibly offending agents
are helpful and should be obtained, but many persons can be-come delirious at
therapeutic levels of the drug, 2) drug-induced delirium may be the result of
drug interactions and polypharmacy and not the result of a single agent, 3)
over-the-counter medica-tions and preparations (e.g., agents containing
caffeine or phenyl-propanolamine) should also be considered, and 4) delirium can
be caused by the combination of drugs of abuse and prescribed medications
(e.g., cocaine and dopaminergic antidepressants).
The list of drugs of abuse that can produce
delirium is ex-tensive. Some such agents have enjoyed a resurgence after years
of declining usage. These include lysergic acid diethylamide, psi-locybin
(hallucinogenic mushrooms), heroin and amphetamines. Other agents include
barbiturates, cannabis (especially depend-ent on setting, experience of the
user and whether it is laced with phencyclidine [“superweed”] or heroin),
jimsonweed (highly an-ticholingeric) and mescaline. In cases in which
intravenous use of drugs is suspected, HIV spectrum illness must be ruled out
as an etiological agent for delirium.
The physical examination of a patient with
suspected illicit drug-induced delirium may reveal sclerosed veins, “pop” scars
caused by subcutaneous injection of agents, pale and atrophic na-sal mucosa
resulting from intranasal use of cocaine, injected con-junctiva and pupillary
changes. Toxicological screens are helpful but may not be available on an
emergency basis.
Substance Withdrawal Delirium
Alcohol and certain sedating drugs can produce a
withdrawal delirium when their use is abruptly discontinued or signifi-cantly
reduced. Withdrawal delirium requires a history of use of a potentially
addicting agent for a sufficient amount of time to produce dependence. It is
associated with such typical physical findings as abnormal vital signs,
pupillary changes, tremor, dia-phoresis, nausea and vomiting, and diarrhea.
Patients generally
complain of abdominal and leg cramps, insomnia,
nightmares, chills, hallucinations (especially visual) and a general feeling of
“wanting to jump out of my skin”. Some varieties of drug with-drawal, although
uncomfortable, are not life threatening (e.g., opioid withdrawal). Others such
as alcohol withdrawal delirium are potentially fatal. Withdrawal delirium is
much more common in hospitalized patients than in patients living in the
community. The incidence of delirium tremens, for example, is found in 1% of
all alcoholics, but in 5% of hospitalized alcohol abusers. Im-provement of the
delirium occurs when the offending agent is reintroduced or a cross-sensitive
drug (e.g., a benzodiazepine for alcohol withdrawal) is employed. The causes of
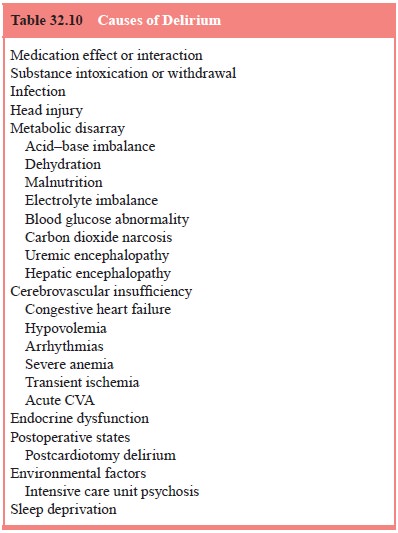
delirium are summarized in Table 32.10).
Diagnosis
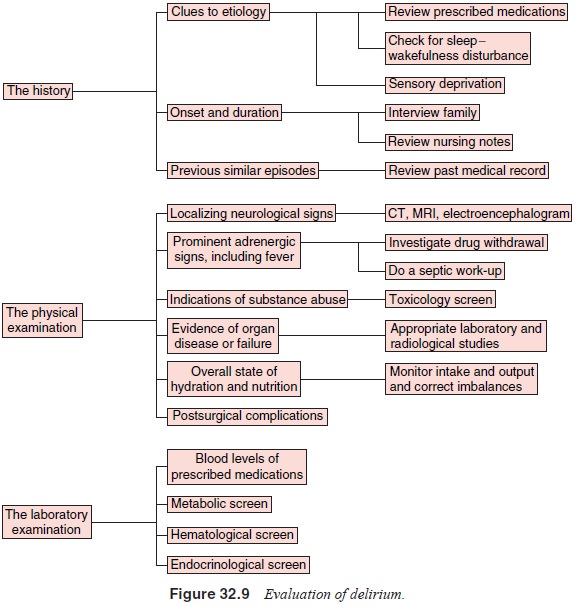
Appropriate workup of delirious patients includes a
complete physical status, mental status and neurological examination.
History taking from the patient, any available
family, pre-vious physicians, the old chart and the patient’s current nurse is
essential. Previous delirious states, etiologies identified in the past and
interventions that proved effective should be elucidated. The appropriate
evaluation of the delirious patient is reviewed in Figure 32.9
Differential Diagnosis
Delirium must be differentiated from dementia
because the two conditions may have different prognoses. In contrast to the
changes in dementia, those in delirium have an acute onset. The symptoms in
dementia tend to be relatively stable over time, whereas clinical features of
delirium display wide fluctuation with periods of relative lucidity. Clouding
of consciousness is an essential feature of delirium, but demented patients are
usu-ally alert. Attention and orientation are more commonly dis-turbed in
delirium, although the latter can become impaired in advanced dementia.
Perception abnormalities, alterations in the sleep–wakefulness cycle, and
abnormalities of speech are more common in delirium. Most important, a delirium
is more likely to be reversible than is a dementia.
Delirium and dementia can occur simultaneously; in
fact, the presence of dementia is a risk factor for delirium. Some stud-ies
suggest that about 30% of hospitalized patients with dementia have a
superimposed delirium.
Delirium must often be differentiated from
psychotic states related to such conditions as schizophrenia or mania and
factitious disorders with psychological symptoms or malinger-ing. Generally,
the psychotic features of schizophrenia are more constant and better organized
than are those in delirium, and pa-tients with schizophrenia seldom have the
clouding of conscious-ness seen in delirium. The “psychosis” of patients with
factitious disorder or malingering is inconsistent, and these persons do not
exhibit many of the associated features of delirium. Apathetic and lethargic
patients with delirium may occasionally resemble depressed individuals, but
tests such as EEG distinguish between the two. The EEG demonstrates diffuse
slowing in most delirious states, except for the low-amplitude, fast activity
EEG pattern seen in alcohol withdrawal. The EEG in a functional depression or
psychosis is normal.
Management
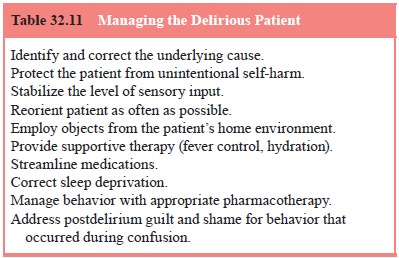
Once delirium has been diagnosed, the etiological
agent must be identified and treated. For the elderly, the first step generally
involves discontinuing or reducing the dosage of potentially of-fending
medications. Some delirious states can be reversed with medication, as in the
case of physostigmine administration for anticholinergic delirium. However,
most responses are not as immediate, and attention must be directed toward
protecting the patient from unintentional self-harm, managing agitated and
psy-chotic behavior, and manipulating the environment to minimize additional
impairment. Supportive therapy should include fluid and electrolyte maintenance
and provision of adequate nutrition. Reorienting the patient is essential and
is best accomplished in a well-lit room with a window, clock and visible wall
calendar. Familiar objects from home such as a stuffed animal, favorite
blanket, or photographs are helpful. Patients who respond incor-rectly to
questions of orientation should be provided with the correct answers. Because
these individuals often see many con-sultants, physicians should introduce
themselves and state their purpose for coming at every visit. Physicians must
take into ac-count that impairments of vision and hearing can produce
confu-sional states, and the provision of appropriate prosthetic devices may be
beneficial. Around-the-clock accompaniment by hospi-tal-provided “sitters” or
family members may be required (see Table 32.11).
these conservative interventions, the delirious pa-tient often requires pharmacological intervention. The liaison psy-chiatrist is the most appropriate person to recommend such treat-ment. The drug of choice for the agitated delirious patients has traditionally been haloperidol. It is particularly beneficial when given by the intravenous route and some authors have reported using dosages as high as 260 mg/day without adverse effect. Ex-trapyramidal symptoms may be less common with haloperidol administered intravenously as opposed to orally and intramuscu-larly. In general, doses in the range of 0.5 to 5 mg intravenously are used, with the frequency of administration depending on a variety of factors including the patient’s age. An electrocardio-gram should be obtained before administering haloperidol. If the QT interval is greater than 450, use of intravenous haloperidol can precipitate an abnormal cardiac rhythm known as Torsades de pointes. Lorazepam has also been proven effective in doses of 0.5 to 2 mg intravenously. Some authors have suggested that haloperidol and lorazepam act synergistically when given to the agitated delirious patient. If the delirium is secondary to drug or alcohol abuse, benzodiazepines or clonidine should be used
For patients who are mildly agitated or amenable to
taking medi-cations by mouth, oral haloperidol or lorazepam is appropriate.
Recent studies have advocated the use of newer atypical antipsy-chotics for
management of behavior and psychotic features in de-lirium. Such agents as
quetiapine, olanzapine, and risperdal and ziprasidone have been used
successfully to treat delirium. Newer agents may have lower incidences of
dystonias and dyskinesias, but still carry the risk of QT interval
prolongation, particularly in patients with electrolyte abnormalities.
Quetiapine and olanzap-ine are quite sedating, and occasionally a combination
of bedtime olanzapine and “as needed” haloperidol is utilized. Olanzapine may
raise blood glucose levels and precipitate weight gain, but is available as a
Zydis preparation, which is absorbed through the oral mucosa and can therefore
be given to patients who are unable to take medications by mouth. A parenteral
form of ziprasidone is also available. Whatever antipsychotic is chosen, the
patient should be carefully monitored for muscle rigidity, unexplained fever,
tremor and other warning signs of neuroleptic side effects.
Outcome of Delirium
After elimination of the cause of the delirium, the
symptoms gradually recede within 3 to 7 days. Some symptoms in certain
populations may take weeks to resolve. The age of the patient and the period of
time during which the patient was delirious affect the symptom resolution time.
In general, the patient has a spotty memory for events that occurred during
delirium. These remem- brances are reinforced by comments from the staff (“You’re
not as confused today”), or the presence of a sitter, or use of wrist
restraints. Patient should be reassured that they were not respon-sible for
their behavior while delirious, and that no one hates or resents them for the
behavior they may have exhibited. As men-tioned earlier, delirious patients
have an increased risk of mortal-ity in the year following their first episode.
Patients with underly-ing dementia show residual cognitive impairment after
resolution of delirium, and it has been suggested that a delirium may merge
into a dementia (Kaplan et al.,
1994).
Related Topics