Chapter: Essentials of Psychiatry: Delirium and Dementia
Amnestic Disorders
Amnestic Disorders
The amnestic disorders are characterized by a
disturbance in memory related to the direct effects of a general medical
condi-tion or the persisting effects of a substance (American Psychiatric
Association, 1994). The impairment should interfere with social and
occupational functioning and represent a significant decline from the previous
level of functioning. The amnestic disorders are differentiated on the basis of
the etiology of the memory loss. These disorders should not be diagnosed if the
memory deficit is a feature of a dissociative disorder, is associated with
demen-tia, or occurs in the presence of clouded sensorium, as in delir-ium.
Amnestic disorders are predominately comprised of those caused by a general
medical condition or those whose etiology is substance-induced.
Epidemiology
The exact prevalence and incidence of the amnestic
disorders are unknown (Kaplan et al.,
1994). Memory disturbances related to specific conditions such as alcohol
dependence and head trauma have been studied and these appear to be the two
most common causes of amnestic disorders. Kaplan and coworkers (Torres et al., 2001) reported that in the
hospital setting the incidence of alcohol-induced
amnestic disorders is decreasing while that of amnestic disorders, secondary to
head trauma, is on the rise. This may be related to rigorous efforts by
hospital personnel to decrease the incidence of iatrogenic amnestic disorder by
giving thiamine before glucose is administered to a patient with chronic
alcohol dependence and nutritional deficiencies.
Etiology
Amnesia results from generally bilateral damage to
the areas of the brain involved in memory. The areas and structures so
in-volved include the dorsomedial and midline thalamic nuclei, such temporal
lobe-associated structures as the hippocampus, amy-gdala and mamillary bodies.
The left hemisphere may be more important than the right in the occurrence of
memory disorders. Frontal lobe involvement may be responsible for such commonly
seen symptoms as apathy and confabulation.
The specific causes of amnestic disorders include
1) sys-temic medical conditions such as thiamine deficiency; 2) brain
conditions, including seizures, cerebral neoplasms, head injury, hypoxia,
carbon monoxide poisoning, surgical ablation of tem-poral lobes,
electroconvulsive therapy and multiple sclerosis; 3) altered blood flow in the
vertebral vascular system, as in tran-sient global amnesia; and 4) effects of a
substance (drug or alco-hol use and exposure to toxins).
Conditions that affect the temporal lobes such as
herpes infection and Kluver–Bucy syndrome can produce amnesia. Among drugs that
can cause amnestic disorders, triazolam has received the most attention, but
all benzodiazepines can produce
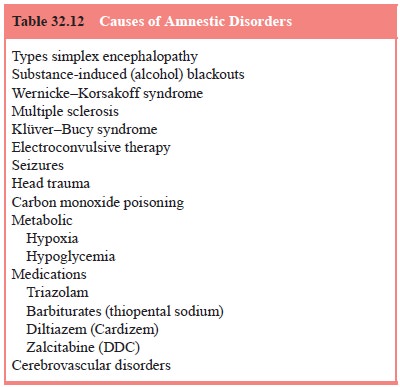
memory impairment, with the dose utilized being the
determin-ing factor (Kirk et al.,
1990) (Table 32.12).
Clinical Features
Patients with amnestic disorder have impaired
ability to learn new information (anterograde amnesia) or cannot remember
ma-terial previously learned (retrograde amnesia). Memory for the event that
produced the deficit (e.g., a head injury in a motor ve-hicle accident) may
also be impaired.
Remote recall (tertiary memory) is generally good, so pa-tients may be able to relate accurately incidents that occurred during childhood but not remember what they had for breakfast. As illus-trated by such conditions as thiamine amnestic syndrome, immedi-ate memory is often preserved. In some instances, disorientation to time and place may occur, but disorientation to person is unusual.
The onset of the amnesia is determined by the
precipitant and may be acute as in head injury or insidious as in poor
nu-tritional states. DSM-IV characterizes short-duration amnestic disorder as
lasting less than 1 month and long-duration disorder lasting 1 month or longer.
Often individuals lack insight into the memory deficit and vehemently insist
that their inaccurate re-sponses on a Mental Status Examination are correct.
Selected Amnestic Disorders
Blackouts
Blackouts are periods of amnesia for events that
occur during heavy drinking (Tarter and Schneider, 1976). Typically, a person
awakens the morning after consumption and does not remember what happened the
night before. Unlike delirium tremens, which is related to chronicity of
alcohol abuse, blackouts are more a measure of the amount of alcohol consumed
at any one time. Thus, blackouts are common in binge pattern drinkers and may
occur the first time a person ingests a large amount of alcohol. Blackouts are
generally transient phenomena, but some patients may continue to have blackouts
for weeks even after they have stopped using alcohol. These memory lapses are
similar to black-outs experienced while using alcohol. With continued sobriety,
the blackouts should end, but information forgotten during past blackouts is
never remembered. Blackouts may also be produced by agents with
cross-sensitivity to alcohol, such as benzodi-azepines. Blackouts should not be
confused with alcohol-induced dementia, which presents with cortical atrophy on
CT scans, as-sociated features of dementia and a usually irreversible course.
Korsakoff’s Syndrome
Korsakoff’s syndrome is an amnestic disorder caused
by thia-mine deficiency. Although generally associated with alcohol abuse, it
can occur in other malnourished states such as maras-mus, gastric carcinoma and
HIV spectrum disease (Reulen et al.,
1985; Victor, 1987). This syndrome is usually associated with Wernicke’s
encephalopathy, which involves ophthalmoplegia, ataxia and confusion.
Korsakoff’s syndrome is often associated with a neuropathy and occurs in about
85% of untreated patients with Wernicke’s disease (Kaplan et al., 1994). Complete recovery from Korsakoff’s syndrome is rare.
Head Injury
Head injuries can produce a wide variety of
neurological and psy-chiatric disorders, even in the absence of radiological
evidence of structural damage. Delirium, dementia, mood disturbances,
behavioral disinhibition, alterations of personality and amnestic disorders may
result (Torres et al., 2001). Amnesia
in head injury is for events preceding the incident and the incident itself,
lead-ing some physicians to consider these patients as having facti-tious
disorders or being malingerers. The eventual duration of the amnesia is related
to the degree of memory recovery that occurs in the first few days after the
injury. Amnesia after head injury has become a popular plot device in novels
and motion pictures, many of which are depictions that erroneously suggest that
a sec-ond blow to the head is curative
Differential Diagnosis
Amnestic disorders must be differentiated from the
less disrup-tive changes in memory that occur in normal aging, the memory
impairment that is accompanied by other cognitive deficits in dementia, the
amnesia that might occur with clouded conscious-ness in delirium, the
stress-induced impairment in recall seen in dissociative disorders, and the
inconsistent amnestic deficits seen in factitious disorder and malingering.
Treatment
As in delirium and dementia, the primary goal in
the amnestic dis-orders is to discover and treat the underlying cause. Because
some of these causes of amnestic disorder are associated with dangerous
self-damaging behavior (e.g., suicide attempts by hanging, carbon monoxide
poisoning, deliberate motor vehicle accidents, self-in-flicted gunshot wounds
to the head and chronic alcohol abuse), some form of psychiatric involvement is
often necessary. In the hospital, continuous reorientation by means of verbal
redirection, clocks and calendars can allay the patient’s fears. Supportive
indi-vidual psychotherapy and family counseling are beneficial.
Related Topics