Chapter: Essentials of Psychiatry: Delirium and Dementia
Dementia, Delirium and Other Cognitive Disorders
Dementia, Delirium and Other
Cognitive Disorders
Dementia
Dementia is defined in DSM-IV as a series of
disorders character-ized by the development of multiple cognitive deficits
(including memory impairment) that are due to the direct physiological effects
of a general medical condition, the persisting effects of a substance, or
multiple etiologies (e.g., the combined effects of a metabolic and a
degenerative disorder) (American Psychiatric Association, 1994). The disorders
constituting the dementias share a common symptom presentation and are
identified and classified on the basis of etiology. The cognitive deficits
exhibited in these disorders must be of significant severity to interfere with
either occupational functioning or the individual’s usual social activities or
relationships. In addition, the observed deficits must represent a decline from
a higher level of function and not be the consequence of a delirium. A delirium
can be superimposed on a dementia, however, and both can be diagnosed if the
dementia is observed when the delirium is not in evidence. Dementia typically
is chronic and occurs in the presence of a clear sensorium. If clouding of
con-sciousness occurs, the diagnosis of delirium should be considered. The
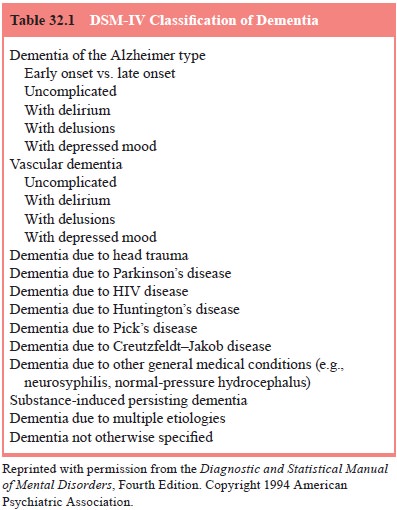
DSM-IV classification of dementia is reviewed in Table 32.1.
Epidemiology
The prevalence of dementias is not precisely known.
Estimates vary depending on the age range of the population studied and whether
the individuals sampled were in the general community, acute care facilities,
or long-term nursing institutions. A review of 47 sur-veys of dementia
conducted between 1934 and 1985 indicated that the prevalence of dementia
increased exponentially by age, dou-bling every 5 years up to age 95 years, and
that this condition was equally distributed among men and women, with
Alzheimer’s de-mentia (AD) much more common in women (Slaby and Erle, 1993). A
National Institute of Mental Health Multisite Epidemiological Catchment Area
study revealed a 6-month prevalence rate for mild dementia of 11.5 to 18.4% for
persons older than 65 years living in the community (Kallmann, 1989). The rate
for severe dementia was higher for the institutionalized elderly: 15% of the
elderly in retirement communities, 30% of nursing home residents and 54% of the
elderly in state hospitals (Cummings and Benson, 1983).
Studies suggest that the fastest growing segment of the US population consists of persons older than the age of 85 years, 15% of whom are demented (Henderson, 1990). Half of the US population currently lives to the age of 75 years and one quarter lives to the age of 85 (Berg et al., 1994). A study of 2000 con-secutive admissions to a general medical hospital revealed that 9% were demented and, among those, 41% were also delirious on admission (Erkinjuntii et al., 1986). The cost of providing care for demented patients exceeds $100 billion annually (about 10% of all health care expenditures), and the average cost to families in 1990 was $18 000 a year (Berg et al., 1994
Clinical Features
Essential to the diagnosis of dementia is the
presence of cognitive deficits that include memory impairment and at least one
of the following abnormalities of cognition: aphasia, agnosia, apraxia, or a
disturbance in executive function (American Psychiatric Association, 1994).
Memory function is divided into three compartments that can easily be evaluated
during a mental status examination. These are immediate recall (primary
memory), recent (secondary) memory and remote (tertiary) memory. Primary memory
is characterized by a limited capacity, rapid accessibility and a duration of
seconds to a minute (Karp, 1984). The anatomic site of destruction of primary
memory is the reticular activating system, and the principal activity of the
primary memory is the registration of new information. Primary memory is
generally tested by asking the individual to repeat immediately a series of
numbers in the order given. For instance, if the examiner mentions the numbers
1–2–3, the patient should be able to repeat them in the same order. This loss
of ability to register new information accounts in part for the confusion and
frustration the demented patient feels when confronted with unexpected changes
in daily routine. Secondary memory has a much larger capacity than primary
memory, a duration of minutes to years, and relatively slow accessibility. The
anatomic site of dysfunction for secondary memory is the limbic system, and
individuals with a lesion in this area may have little difficulty repeating
digits immediately, but show rapid decay of these new memories. In minutes, the
patient with limbic involvement may be totally unable to recall the digits or
even remember that a test has been administered (Karp, 1984). Thus, secondary
memory represents the retention and recall of information that has been
previously registered by primary memory. Clinically, secondary memory is tested
by having the individual repeat three objects afterhaving been distracted
(usually by the examiner’s continuation of the Mental Status Examination) for 3
to 5 minutes. Like primary memory, secondary recall is often impaired in
dementia. Often if the examiner gives the demented patient a clue (such as “one
of the objects you missed was a color”), the patient correctly identifies the
object. If this occurs the memory testing should be scored as “three out of
three with a cue”, which is considered to be a slight impairment. Giving clues
to the demented patient with a primary memory loss is pointless, because the
memories were never registered. Wernicke–Korsakoff syndrome is an example of a
condition in which primary memory may be intact while secondary recall is
impaired.
Tertiary (remote) memory has a capacity that is
probably unlimited, and such memories are often permanently retained. Access to
tertiary memories is slow, and the anatomical dys-function in tertiary memory
loss is in the association cortex (Karp, 1984). In the early stages of
dementia, tertiary memory is generally intact. It is tested by instructing the
individual to remember personal information or past material. The personal
significance of the information often influences the patient’s abil-ity to
remember it. For example, a woman who worked for many years as a seamstress
might remember many details related to that occupation, but could not recall
the names of past presidents or three large cities in the USA. Thus, a
patient’s inability to re-member highly significant past material is an ominous
finding. Collateral data from informants is essential in the proper assess-ment
of memory function. In summary, primary and secondary memories are most likely
to be impaired in dementia, with terti-ary memory often spared until late in
the course of the disease.
In addition to defects in memory, patients with
dementia often exhibit impairments in language, recognition, object nam-ing and
motor skills. Aphasia is an abnormality of language that often occurs in
vascular dementias involving the dominant hemi-sphere. Because this hemisphere
controls verbal, written and sign language, these patients may have significant
problems interact-ing with people in their environment. Patients with dementia
and aphasia may exhibit paucity of speech, poor articulation and a telegraphic
pattern of speech (nonfluent, Broca’s aphasia). This form of aphasia generally
involves the middle cerebral artery with resultant paresis of the right arm and
lower face. Despite faulty communication skills, patients having dementia with
non-fluent aphasia have normal comprehension and awareness of their language
impairment. As a result, such patients often present with significant
depression, anxiety and frustration.
By contrast, patients having dementia with fluent
(Wernicke’s) aphasia may be quite verbose and articulate, but much of the
language is nonsensical and rife with such parap-hasias as neologisms and clang
(rhyming) associations. Whereas nonfluent aphasias are usually associated with
discrete lesions, fluent aphasia can result from such diffuse conditions as
demen-tia of the Alzheimer type. More commonly, fluent aphasias oc-cur in
conjunction with vascular dementia secondary to temporal or parietal lobe CVA.
Because the demented patients with fluent aphasia have impaired comprehension,
they may seem apathetic and unconcerned with their language deficits if they
are, in fact, aware of them at all. They do not generally display the
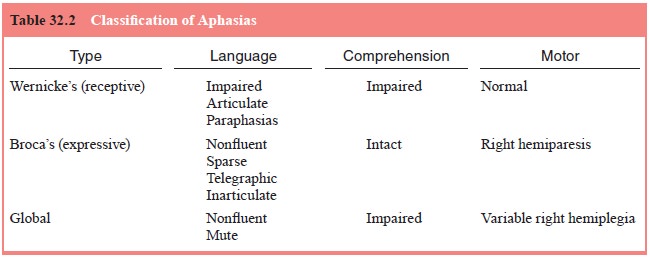
emo-tional distress of patients with dementia and nonfluent aphasia (Table
32.2).
Patients with dementia may also lose their ability
to rec-ognize. Agnosia is a feature of a dominant hemisphere lesion and
involves altered perception in which, despite normal sensations, intellect and
language, the patient cannot recognize objects. This
is in contrast to aphasia in which the patient with
dementia may not be able to name objects, but can recognize them. The type of
agnosia depends on the area of the sensory cortex that is in-volved. Some
demented patients with severe visual agnosia can-not name objects presented,
match them to samples, or point to objects named by the examiner. Other patients
may present with auditory agnosia and be unable to localize or distinguish such
sounds as the ringing of a telephone. A minority of demented patients may
exhibit astereognosis, inability to identify an ob-ject by palpation. Demented
patients may also lose their ability to carry out selected motor activities
despite intact motor abili-ties, sensory function and comprehension of the
assigned task (apraxia). Affected patients cannot perform such activities as
brushing their teeth, chewing food, or waving good-bye when asked to do so.
The two most common forms of apraxia in demented
pa-tients are ideational and gait apraxia. Ideational apraxia is the inability
to perform motor activities that require sequential steps and results from a
lesion involving both frontal lobes or the com-plete cerebrum. Gait apraxia,
often seen in such conditions as normal-pressure hydrocephalus, is the
inability to perform vari-ous motions of ambulation. It also results from
conditions that diffusely affect the cerebrum. Impairment of executive function
is the ability to think abstractly, plan, initiate and end complex behavior. On
Mental Status Examination, patients with dementia display problems coping with
new tasks. Such activities as sub-tracting serial sevens may be impaired.
Obviously, aphasia, agnosia, apraxia and impairment
of executive function can seriously impede the ability of the de-mented
patients to interact with their environment. An appro-priate mental status
examination of the patient with suspected dementia should include screening for
the presence of these abnormalities.
Associated Features and Behavior
In addition to the diagnostic features already
mentioned, patients with dementia display other identifying features that often
prove problematic. Poor insight and poor judgment are common in dementia and
often cause patients to engage in potentially dan-gerous activities or make
unrealistic and grandiose plans for the future. Visual–spatial functioning may
be impaired, and if pa-tients have the ability to construct a plan and carry it
out, suicide attempts can occur. More common is unintentional self-harm
re-sulting from carelessness, undue familiarity with strangers, and disregard
for the accepted rules of conduct.
Emotional lability, as seen in pseudobulbar palsy
after cer-ebral injury, can be particularly frustrating for caregivers, as are
occasional psychotic features such as delusions and hallucina-tions. Changes in
their environment and daily routine can be par-ticularly distressing for
demented patients, and their frustration can be manifested by violent behavior.
Course
The course of a particular dementia is influenced
by its etiology. Although historically the dementias have been considered
pro-gressive and irreversible, there is, in fact, significant variation in the
course of individual dementias. The disorder can be pro-gressive, static, or
remitting (American Psychiatric Association, 1994). In addition to the
etiology, factors that influence the course of the dementia include: 1) the
time span between the onset and the initiation of prescribed treatment, 2) the
degree of reversibil-ity of the particular dementia, 3) the presence of
comorbid psy-chiatric disorders, and 4) the level of psychosocial support. The
previous distinction between treatable and untreatable dementias has been
replaced by the concepts of reversible, irreversible and arrestable dementias.
Most reversible cases of dementia are as-sociated with shorter duration of
symptoms, mild cognitive im-pairment and superimposed delirium. Specifically,
the dementias caused by drugs, depression and metabolic disorders are most
likely to be reversible. Other conditions such as normal pressure
hydrocephalous, subdural hematomas and tertiary syphilis are more commonly
arrestable.
Although potentially reversible dementias should be
ag-gressively investigated, in reality, only 8% of dementias are par-tially
reversible and about 3% fully reversible (Kaufman, 1990b). There is some
evidence to suggest that early treatment of de-mented patients, particularly
those with Alzheimer’s type, with such agents as donepezil, which acts as an
inhibitor of acetylcho-linesterase, and galanthamine may slow the rate of
progression of the dementia.
Differential Diagnosis
Memory impairment occurs in a variety of conditions
includ-ing delirium, amnestic disorders and depression (American Psychiatric
Association, 1994). In delirium, the onset of altered memory is acute and the
pattern typically fluctuates (waxing and waning) with increased proclivity for
confusion during the night. Delirium is more likely to feature autonomic
hyperactivity and alterations in level of consciousness. In some cases a
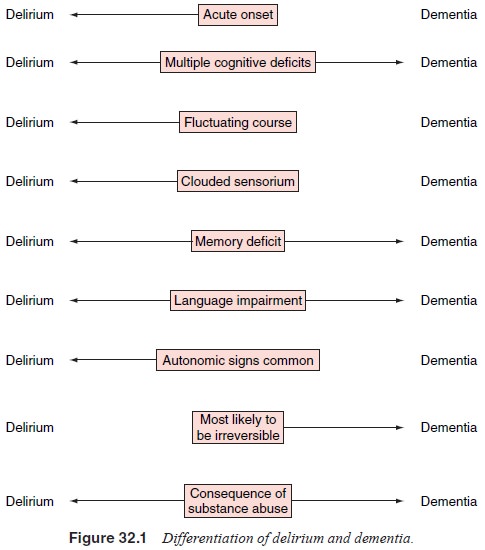
dementia can have a superimposed delirium (Figure 32.1
Patients with major depressive disorder often
complain of lapses in memory and judgment, poor concentration and seem-ingly
diminished intellectual capacity. Often these symptoms are mistakenly diagnosed
as dementia, especially in elderly patients. A thorough medical history and
mental status examination focus-ing on such symptoms as hopelessness, crying
episodes and un-realistic guilt, in conjunction with a family history of
depression, can be diagnostically beneficial. The term pseudodementia has been used to denote cognitive impairment
secondary to a func-tional psychiatric disorder, most commonly depression
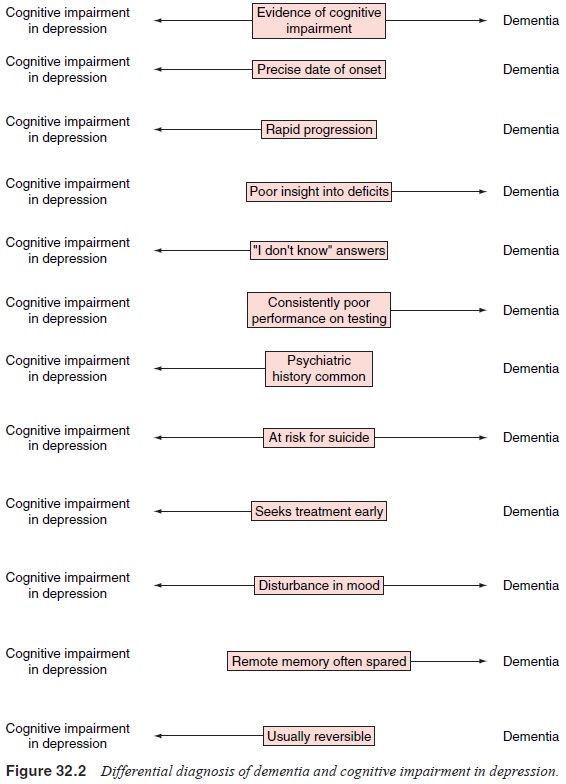
(Korvath et al., 1989). In comparison
with demented patients, those with depressive
pseudodementia exhibit better insight regarding their cognitive dysfunction,
are more likely to give “I don’t know” answers, and may exhibit neurovegetative
signs of depression. Pharmacological treatment of the depression should improve
the cognitive dysfunction as well. Because of the rapid onset of their
antidepressant action, the use of psychostimulants (methylpheni-date,
dextroamphetamine) to differentiate between dementia and pseudodementia has
been advocated by some authors (Frierson et
al., 1991). Some authors have proposed abandonment of the term pseudodementia, suggesting that
most patients so diag-nosed have both genuine dementia and a superimposed
affective disorder (Figure 32.2).
An amnestic disorder also presents with a
significant memory deficit, but without the other associated features such as
aphasia, agnosia and apraxia. If cognitive impairment occurs only in the
context of drug use, substance intoxication or sub-stance withdrawal is the
appropriate diagnosis. Although mental of age and abnormalities of memory do
not always occur. Mental retardation must be considered in the differential
diagnosis of dementias of childhood and adolescence along with such dis-orders
as Wilson’s disease (hepatolenticular degeneration), lead intoxication,
subacute sclerosing panencephalitis, HIV spectrum disorders and substance
abuse, particularly abuse of inhalants. If an individual develops dementia
before age 18 years and has an IQ in the mentally retarded range (i.e., below
70), an additional diagnosis of mental retardation may be justified.
Patients with schizophrenia may also exhibit a
variety of cognitive abnormalities, but this condition also has an early onset,
a distinctive constellation of other symptoms (e.g., delu-sions,
hallucinations, disorganized speech), and does not result from a medical
condition or the persisting effects of a substance. Factitious disorder and
malingering must be distinguished from dementia. The patient with factitious
disorder and psychological symptoms may have some apparent cognitive deficits
reminis-cent of a dementia.
Dementia must also be distinguished from
age-related cognitive decline (also known as benign senescence). Only when such
changes exceed the level of altered function to be expected for the patient’s
age is the diagnosis of dementia warranted (American Psychiatric Association,
1994).
Physical and Neurological Examinations in Dementia
The physical examination may offer clues to the etiology of the dementia; however, in the elderly, one must be aware of the normal changes associated with aging and differentiate them from signs of dementia. Often the specific physical examination findings indicate the area of the central nervous system affected by the etiological process. Parietal lobe dysfunction is suggested by such symptoms as astereognosis, constructional apraxia, ano-sognosia and problems with two-point discrimination (Kaufman, 1990a). The dominant hemisphere parietal lobe is also involved in Gerstmann’s syndrome, which includes agraphia, acalculia, finger agnosia and right–left confusion.
Reflex changes such as hyperactive deep tendon
reflexes, Babinski’s reflex and hyperactive jaw jerk are indicative of cerebral
injury. However, primitive reflexes such as the palmar–mental re-flex (tested
by repeatedly scratching the base of the patient’s thumb, with a positive
response being slight downward movement of the lower lip and jaw), which occurs
in 60% of normal elderly people, and the snout reflex, seen in a third of
elderly patients, are not diag-nostically reliable for dementia (Wolfson and
Katzman, 1983).
Ocular findings such as nystagmus (as in brain stem
lesions), ophthalmoplegia (Wernicke–Korsakoff syndrome), anisocoria papilledema
(hypertensive encephalopathy), cortical blindness (Anton’s syndrome), visual
field losses (CVA hemianopia), Kayser–Fleischer rings (Wilson’s disease) and
Argyll Robertson pupils (syphilis, diabetic neuropathy) can offer valuable
clues to the etiology of the cognitive deficit (Victor and Adams, 1974).
Movement disorders including tremors (Parkinson’s
dis-ease, drug intoxication, cerebellar dysfunction, Wilson’s disease), chorea
(Huntington’s disease, other basal ganglia lesions), myo-clonus (subacute
sclerosing panencephalitis, Creutzfeldt–Jakob disease, Alzheimer’s disease,
anoxia) and asterixis (hepatic disease, uremia, hypoxia, carbon dioxide
retention) should be noted.
Gait disturbances, principally apraxia
(normal-pressure hydrocephalus, inhalant abuse, cerebellar dysfunction) and
pe-ripheral neuropathy (Korsakoff’s syndrome, neurosyphilis, heavy metal
intoxication, solvent abuse, isoniazid or phenytoin toxicity, vitamin
deficiencies and HIV spectrum illnesses), are
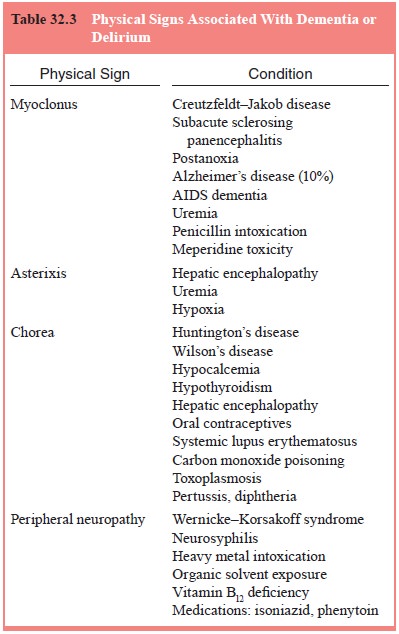
also common in dementia. Extrapyramidal symptoms in
the ab-sence of antipsychotics may indicate substance abuse, especially
phencyclidine abuse, or basal ganglia disease. Although the many and varied
physical findings of dementia are too numer-ous to mention here in any detail,
it should be obvious that the physical examination is an invaluable tool in the
assessment of dementia (Table 32.3).
Mental Status Examination
The findings on the Mental Status Examination vary
depending on the etiology of the dementia. Some common abnormalities have been
discussed previously (see earlier section on clinical features). In general,
symptoms seen on the Mental Status Ex-amination, whatever the etiology, are
related to the location and extent of brain injury, individual adaptation to
the dysfunction, premorbid coping skills and psychopathology, and concurrent
medical illness.
Disturbance of memory, especially primary and
second-ary memory, is the most significant abnormality. Confabulation may be
present as the patient attempts to minimize the memory impairment.
Disorientation and altered levels of consciousness may occur, but are generally
not seen in the early stages of de-mentia uncomplicated by delirium. Affect may
be affected as in the masked facies of Parkinson’s disease and the expansive
affect
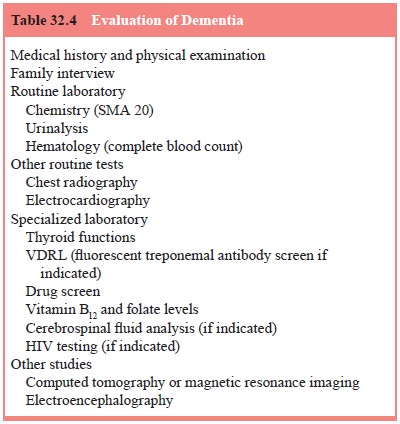
and labile mood of pseudobulbar palsy after
cerebral injury. The affect of patients with hepatic encephalopathy is often
described as blunted and apathetic. Lack of inhibition leading to such behavior
as exposing oneself is common, and some conditions such as tertiary syphilis
and untoward effects of some medication can precipitate mania. The Mental Status
Examination, in conjunction with a complete medical history from the patient
and informants and an adequate physical examination, is essential in the
evaluation and differential diagnosis of dementia (Table 32.4).
Related Topics