Chapter: Medical Surgical Nursing: Assessment and Management of Patients With Endocrine Disorders
Adrenocortical Insufficiency (AddisonŌĆÖs Disease) - Management of Patients With Adrenal Disorders
ADRENOCORTICAL
INSUFFICIENCY (ADDISONŌĆÖS DISEASE)
Pathophysiology
AddisonŌĆÖs disease, or adrenocortical insufficiency, results
whenadrenal cortex function is inadequate to meet the patientŌĆÖs need for
cortical hormones. Autoimmune or idiopathic atrophy of the adrenal glands is
responsible for 80% of cases (Rakel & Bope, 2001). Other causes include
surgical removal of both adrenal glands or infection of the adrenal glands.
Tuberculosis and histoplasmosis are the most common infections that de-stroy
adrenal gland tissue. Although autoimmune destruction has replaced tuberculosis
as the principal cause of AddisonŌĆÖs dis-ease, tuberculosis should be considered
in the diagnostic workup because of its increasing incidence. Inadequate
secre-tion of ACTH from the pituitary gland also results in adrenal
insufficiency because of decreased stimulation of the adrenal cortex.
Therapeutic
use of corticosteroids is the most common cause of adrenocortical insufficiency
(Coursin & Wood, 2002). The symptoms of adrenocortical insufficiency may
also result from the sudden cessation of exogenous adrenocortical hormonal
therapy, which suppresses the bodyŌĆÖs normal response to stress and inter-feres
with normal feedback mechanisms. Treatment with daily administration of
corticosteroids for 2 to 4 weeks may suppress function of the adrenal cortex;
therefore, adrenal insufficiency should be considered in any patient who has
been treated with corticosteroids.
Clinical Manifestations
AddisonŌĆÖs
disease is characterized by muscle weakness, anorexia, gastrointestinal symptoms,
fatigue, emaciation, dark pigmenta-tion of the skin, knuckles, knees, elbows,
and mucous mem-branes, hypotension, and low blood glucose levels, low serum
sodium levels, and high serum potassium levels. Mental status changes such as
depression, emotional lability, apathy, and con-fusion are present in 60% to
80% of patients. In severe cases, the disturbance of sodium and potassium
metabolism may be marked by depletion of sodium and water and severe, chronic
dehydration.
With
disease progression and acute hypotension, the patient develops addisonian crisis, which is
characterized by cyanosis and the classic signs of circulatory shock: pallor,
apprehension, rapid and weak pulse, rapid respirations, and low blood pressure.
In ad-dition, the patient may complain of headache, nausea, abdominal pain, and
diarrhea and show signs of confusion and restlessness. Even slight
overexertion, exposure to cold, acute infections, or a decrease in salt intake
may lead to circulatory collapse, shock, and death if untreated. The stress of
surgery or dehydration resulting from preparation for diagnostic tests or
surgery may precipitate an addisonian or hypotensive crisis.
Assessment and Diagnostic Findings
Although
the clinical manifestations presented appear specific, the onset of AddisonŌĆÖs
disease usually occurs with nonspecific symptoms. The diagnosis is confirmed by
laboratory test results. Laboratory findings include decreased blood glucose
(hypoglyce-mia) and sodium (hyponatremia) levels, an increased serum potas-sium
(hyperkalemia) level, and an increased white blood cell count (leukocytosis).
The
diagnosis is confirmed by low levels of adrenocortical hor-mones in the blood
or urine and decreased serum cortisol levels. If the adrenal cortex is
destroyed, baseline values are low, and ACTH administration fails to cause the
normal rise in plasma cortisol and urinary 17-hydroxycorticosteroids. If the
adrenal gland is normal but not stimulated properly by the pituitary, a normal
response to repeated doses of exogenous ACTH is seen, but no response follows
the administration of metyrapone, which stimulates endogenous ACTH.
Medical Management
Immediate
treatment is directed toward combating circulatory shock: restoring blood
circulation, administering fluids and corticosteroids, monitoring vital signs,
and placing the patient in a recumbent position with the legs elevated.
Hydrocortisone (Solu-Cortef) is administered intravenously, followed with 5%
dextrose in normal saline. Vasopressor amines may be required if hypotension persists.
Antibiotics
may be administered if infection has precipitated adrenal crisis in a patient
with chronic adrenal insufficiency. Ad-ditionally, the patient is assessed
closely to identify other factors, stressors, or illnesses that led to the
acute episode.
Oral
intake may be initiated as soon as tolerated. Gradually, intravenous fluids are
decreased when oral fluid intake is adequate to prevent hypovolemia. If the
adrenal gland does not regain function, the patient needs lifelong replacement
of corticosteroids and mineralocorticoids to prevent recurrence of adrenal
insuffi-ciency. The patient will require additional supplementary ther-apy with
glucocorticoids during stressful procedures or significant illnesses to prevent
addisonian crisis (Coursin & Wood, 2002). Additionally, the patient may
need to supplement dietary intake with added salt during times of
gastrointestinal losses of fluids through vomiting and diarrhea.
Nursing Management
ASSESSING THE PATIENT
The
health history and examination focus on the presence of symptoms of fluid
imbalance and on the patientŌĆÖs level of stress. To detect inadequate fluid
volume, the nurse monitors the blood pressure and pulse rate as the patient
moves from a lying to a standing position. The nurse assesses the skin color
and turgor for changes related to chronic adrenal insufficiency and
hypovolemia. Other key assessments include checking for weight changes, mus-cle
weakness, and fatigue and investigating any illness or stress that may have
precipitated the acute crisis.
MONITORING AND MANAGING ADDISONIAN CRISIS
The
patient at risk is monitored for signs and symptoms indica-tive of addisonian
crisis. These symptoms are often the manifes-tations of shock: hypotension;
rapid, weak pulse; rapid respiratory rate; pallor; and extreme weakness. The
patient with addisonian crisis is at risk for circulatory collapse and shock;
therefore, physical and psy-chological stressors must be avoided. These include
exposure to cold, overexertion, infection, and emotional distress.
The
patient with addisonian crisis requires immediate treat-ment with intravenous
administration of fluid, glucose, and elec-trolytes, especially sodium;
replacement of missing steroid hormones; and vasopressors. During acute
addisonian crisis, the patient must avoid exertion; therefore, the nurse
anticipates the patientŌĆÖs needs and takes measures to meet them.
Careful
monitoring of symptoms, vital signs, weight, and fluid and electrolyte status
is essential to monitor the patientŌĆÖs progress and return to a precrisis state.
To reduce the risk of future episodes of addisonian crisis, efforts are made to
identify and re-duce the factors that may have led to the crisis.
RESTORING FLUID BALANCE
To
provide information about fluid balance and the adequacy of hormone
replacement, the nurse assesses the patientŌĆÖs skin turgor, mucous membranes,
and weight while instructing the patient to report increased thirst, which may
indicate impending fluid im-balance. Lying, sitting, and standing blood
pressures also provide information about fluid status. A decrease in systolic
pressure (20 mm Hg or more) may indicate depletion of fluid volume, es-pecially
if accompanied by symptoms. The nurse encourages the patient to consume foods
and fluids that will assist in restoring and maintaining fluid and electrolyte
balance; along with the dietitian, the nurse assists the patient to select
foods high in sodium during gastrointestinal disturbances and very hot weather.
The
nurse instructs the patient and family to administer hor-mone replacement as
prescribed and to modify the dosage dur-ing illness and other stressful
occasions. Written and verbal instructions are provided about the
administration of mineralo-corticoid (Florinef) or corticosteroid (prednisone)
as prescribed.
IMPROVING ACTIVITY TOLERANCE
Until
the patientŌĆÖs condition is stabilized, the nurse takes pre-cautions to avoid
unnecessary activity and stress that could pre-cipitate another hypotensive
episode. Efforts are made to detect signs of infection or the presence of other
stressors. Even minor events or stressors may be excessive in patients with
adrenal in-sufficiency. During the acute crisis, the nurse maintains a quiet,
nonstressful environment and performs all activities (eg, bathing, turning) for
the patient. Explaining all procedures to the patient and family will reduce
their anxiety. Explaining the rationale for minimizing stress during the acute
crisis assists the patient to in-crease activity gradually.
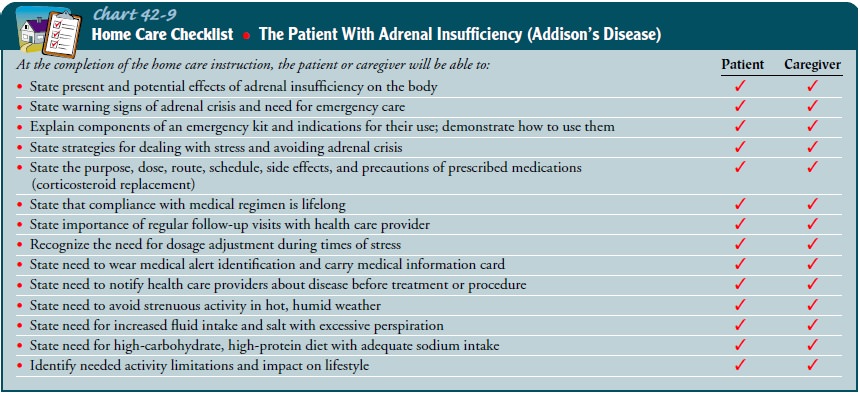
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care.
Because of
the need for lifelong re-placement of adrenal cortex hormones to prevent
addisonian crises, the patient and family members receive explicit verbal and
written instructions about the rationale for replacement therapy and proper
dosage. Additionally, they are instructed about how to modify the medication
dosage and increase salt intake in times of illness, very hot weather, and
other stressful situations. The pa-tient also learns how to modify diet and
fluid intake to help main-tain fluid and electrolyte balance.
The
patient and family are frequently prescribed preloaded, single-injection
syringes of corticosteroid for use in emergencies. Careful instructions about
how and when to use the injection are also provided. It is important to
instruct the patient to inform other health care providers, such as dentists,
about the use of cor-ticosteroids, to wear a medical alert bracelet, and to
carry in-formation at all times about the need for corticosteroids. If the
patient with AddisonŌĆÖs disease requires surgery, careful adminis-tration of
fluids and corticosteroids is necessary before, during, and after surgery to
prevent addisonian crisis.
The
patient and family need to know the signs of excessive or insufficient hormone
replacement. The development of edema or weight gain may signify too high a
dose of hormone; postural hypotension (decrease in systolic blood pressure,
lightheadedness,dizziness on standing) and weight loss frequently signify too
low a dose (Chart 42-9).
Continuing Care.
Although
most patients can return to their joband family responsibilities soon after
hospital discharge, others cannot do so because of concurrent illnesses or
incomplete recov-ery from the episode of adrenal insufficiency. In these
circum-stances, a referral for home care enables the home care nurse to assess
the patientŌĆÖs recovery, monitor hormone replacement, and evaluate stress in the
home. The nurse assesses the patientŌĆÖs and familyŌĆÖs knowledge about medication
therapy and dietary modi-fications. A home visit also allows the nurse to
assess the patientŌĆÖs plans for follow-up visits to the clinic or physicianŌĆÖs
office. The nurse reminds the patient and family about the importance of
par-ticipating in health promotion activities and health screening.
Related Topics