Chapter: Medical Surgical Nursing: Assessment and Management of Patients With Endocrine Disorders
Thyroid Cancer - Management of Patients With Thyroid Disorders
THYROID
CANCER
Cancer
of the thyroid is much less prevalent than other forms of cancer; however, it
accounts for 90% of endocrine malignancies. According to the American Cancer
Society (2002), about 20,700 new cases of thyroid cancer are diagnosed each
year. Women account for 15,800 of the new cases and men 4,900. About 800 women
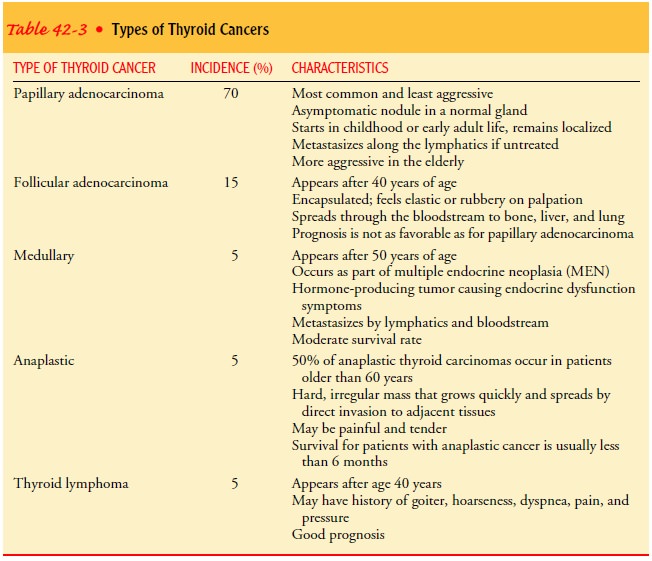
and 500 men die annually from this malig-nancy. There are several types of
cancer of the thyroid gland; the type determines the course and prognosis
(Table 42-3).
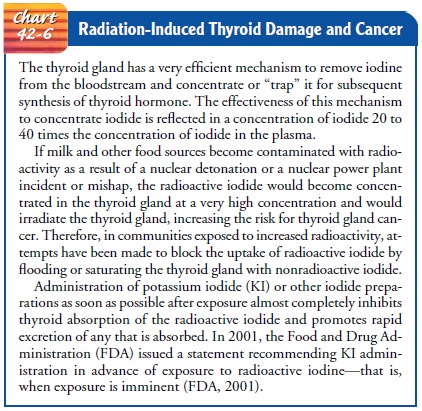
External
radiation of the head, neck, or chest in infancy and childhood increases the
risk of thyroid carcinoma. Between 1940 and 1960, radiation therapy was
occasionally used to shrink en-larged tonsillar and adenoid tissue, to treat
acne, or to reduce an enlarged thymus. For people exposed to external radiation
in childhood, there appears to be an increased incidence of thyroid cancer 5 to
40 years after irradiation. Consequently, people who underwent such treatment
should consult a physician, request an isotope thyroid scan as part of the
evaluation, follow recom-mended treatment of abnormalities of the gland, and
continue with annual checkups (Chart 42-6).
Assessment and Diagnostic Findings
Lesions
that are single, hard, and fixed on palpation or associated with cervical
lymphadenopathy suggest malignancy. Thyroid function tests may be helpful in
evaluating thyroid nodules and masses; however, their results are rarely
conclusive. Needle biopsy of the thyroid gland is used as an outpatient
procedure to make a diagnosis of thyroid cancer, to differentiate cancerous
thyroid nod-ules from noncancerous nodules, and to stage the cancer if
de-tected. The procedure is safe and usually requires only a local anesthetic.
Patients who undergo the procedure are followed closely, however, because
cancerous tissues may be missed during the procedure. A second type of
aspiration or biopsy uses a large-bore needle rather than the fine needle used
in standard biopsy; it may be used when the results of the standard biopsy are
incon-clusive, or with rapidly growing tumors. Additional diagnostic studies
include ultrasound, MRI, CT scans, thyroid scans, radio-active iodine uptake
studies, and thyroid suppression tests.
Medical Management
The
treatment of choice for thyroid carcinoma is surgical re-moval. Total or
near-total thyroidectomy is performed when possible. Modified neck dissection
or more extensive radical neck dissection is performed if there is lymph node
involvement.
SURGICAL MANAGEMENT
Efforts
are made to spare parathyroid tissue to reduce the risk for postoperative
hypocalcemia and tetany. After surgery, ablation procedures are carried out
with radioactive iodine to eradicate residual thyroid tissue if the tumor is
radiosensitive. Radioactive iodine also maximizes the chance of discovering
thyroid metasta-sis at a later date if total-body scans are carried out.
After surgery, thyroid hormone is administered in suppressive doses to lower the levels of TSH to a euthyroid state (Thyroid Carcinoma Guidelines, 2001). If remaining thyroid tissue is in-adequate to produce sufficient thyroid hormone, thyroxine is re-quired permanently.
Several
routes are available for administering radiation to the thyroid or tissues of
the neck, including oral administration of ra-dioactive iodine and external
administration of radiation therapy. The patient who receives external sources
of radiation therapy is at risk for mucositis, dryness of the mouth, dysphagia,
redness of the skin, anorexia, and fatigue. Chemotherapy is infrequently used
to treat thyroid cancer.Patients whose thyroid cancer is detected early and who
are appropriately treated usually do very well. Patients who have had papillary
cancer, the most common and least aggressive tumor, have a 10-year survival
rate greater than 90%. Long-term survival is also common in follicular cancer,
a more aggressive form of thyroid cancer (Tierney et al., 2001). Continued
thyroid hor-mone therapy and periodic follow-up and diagnostic testing,
however, are important to ensure the patient’s well-being (Thy-roid Carcinoma
Guidelines, 2001).
Postoperatively,
the patient is instructed to take exogenous thyroid hormone to prevent
hypothyroidism. Later follow-up in-cludes clinical assessment for recurrence of
nodules or masses in the neck and signs of hoarseness, dysphagia, or dyspnea.
Total-body scans are performed 2 to 4 months after surgery to detect residual
thyroid tissue or metastatic disease. Thyroid hormones are stopped for about 6
weeks before the tests. Care must be taken to avoid iodine-containing foods and
contrast agents. A repeat scan is done 1 year after the initial surgery. If
measurements are stable, a final scan is obtained in 3 to 5 years.
FT4, TSH, serum calcium,
and phosphorus levels are moni-tored to determine whether the thyroid hormone
supplementation is adequate and to note whether calcium balance is maintained.
Although
local and systemic reactions to radiation may occur and may include neutropenia
or thrombocytopenia, these com-plications are rare when radioactive iodine is
used. Patients who undergo surgery that is combined with radioiodine have a
higher survival rate than those undergoing surgery alone. Patient teach-ing
emphasizes the importance of taking prescribed medications and following recommendations
for follow-up monitoring. The patient who is undergoing radiation therapy is
also instructed in how to assess and manage side effects of treatment.
Partial or complete thyroidectomy may be carried out as pri-mary treatment of thyroid carcinoma, hyperthyroidism, or hyper-parathyroidism. The type and extent of the surgery depend on the diagnosis, goal of surgery, and prognosis. Thyroidectomy may be the treatment of choice for patients with symptomatic hyper-parathyroidism (see later discussion), kidney stones, or bone disease.
The
patient undergoing surgery for treatment of hyperthy-roidism is given
appropriate medications to return the thyroid hormone levels and metabolic rate
to normal and to reduce the risk for thyroid storm and hemorrhage during the
postoperative period. Medications that may prolong clotting (eg, aspirin) are
stopped several weeks before surgery to minimize the risk for postoperative
bleeding.
Nursing Management
Important
preoperative goals are to gain the patient’s confidence and reduce anxiety.
Often, the patient’s home life has become tense because of his or her
restlessness, irritability, and nervous-ness secondary to hyperthyroidism.
Efforts are necessary to pro-tect the patient from such tension and stress to
avoid precipitating thyroid storm. If the patient reports increased stress when
with family or friends, suggestions are made to limit contact with them. Quiet
and relaxing forms of recreation or occupational therapy may be helpful.
PROVIDING PREOPERATIVE CARE
The
nurse instructs the patient about the importance of eating a diet high in
carbohydrates and proteins. A high daily caloric in-take is necessary because
of the increased metabolic activity and rapid depletion of glycogen reserves.
Supplementary vitamins, particularly thiamine and ascorbic acid, may be
prescribed. The patient is reminded to avoid tea, coffee, cola, and other
stimulants.
The
nurse also informs the patient about the purpose of pre-operative tests, if
they are to be performed, and explains what pre-operative preparations to
expect. The information should help to reduce the patient’s anxiety about the
surgery. In addition, spe-cial efforts are made to ensure a good night’s rest
before surgery, although many patients are admitted to the hospital on the day
of surgery.
Preoperative
teaching includes demonstrating to the patient how to support the neck with the
hands after surgery to prevent stress on the incision. This involves raising
the elbows and plac-ing the hands behind the neck to provide support and reduce
strain and tension on the neck muscles and the surgical incision.
PROVIDING POSTOPERATIVE CARE
The
nurse periodically assesses the surgical dressings and rein-forces them when
necessary. When the patient is in a recumbent position, the nurse observes the
sides and the back of the neck as well as the anterior dressing for bleeding.
In addition to moni-toring the pulse and blood pressure for any indication of
internal bleeding, it is also important to be alert for complaints of a
sen-sation of pressure or fullness at the incision site. Such symptoms may
indicate hemorrhage and hematoma formation subcuta-neously and should be
reported.
Difficulty
in respiration occurs as a result of edema of the glot-tis, hematoma formation,
or injury to the recurrent laryngeal nerve. This complication requires that an
airway be inserted. Therefore, a tracheostomy set is kept at the bedside at all
times, and the surgeon is summoned at the first indication of respiratory
distress. If the res-piratory distress is due to hematoma, surgical evacuation
is required.
The
intensity of pain is assessed and analgesic agents are ad-ministered as
prescribed for pain. The nurse should anticipate ap-prehension in the patient
and should inform him or her that oxygen will assist breathing. When moving and
turning the patient, the nurse carefully supports the head and avoids tension
on the sutures. The most comfortable position is the semi-Fowler’s position,
with the head elevated and supported by pillows.
Intravenous
fluids are administered during the immediate postoperative period. Water may be
given by mouth as soon as nausea subsides. Usually, there is a little
difficulty in swallowing; initially, cold fluids and ice may be taken better
than other fluids. Often, patients prefer a soft diet to a liquid diet in the
immedi-ate postoperative period.
The
patient is advised to talk as little as possible to reduce edema to the vocal
cords, but when the patient does speak, any voice changes are noted because
they might indicate injury to the recurrent laryngeal nerve, which lies just
behind the thyroid next to the trachea.
An
overbed table may be used to provide easy access to items that are needed
frequently, such as paper tissues, water pitcher and glass, and a small emesis
basin. These are kept within easy reach so that the patient will not need to
turn the head to reach for them. It is also convenient to use this table when
vapor-mist inhalations are prescribed for the relief of excessive mucous secretions.
The patient is usually permitted out of bed
as soon as possible and is encouraged to eat foods that are easily eaten. A
well-balanced, high-calorie diet may be prescribed to promote weight gain.
Su-tures or skin clips are usually removed on the second day. The pa-tient is
usually discharged from the hospital the day of surgery or soon afterward if
the postoperative course is uncomplicated.
MONITORING AND MANAGINGPOTENTIAL COMPLICATIONS
Hemorrhage,
hematoma formation, edema of the glottis, and in-jury to the recurrent
laryngeal nerve are complications that have been reviewed previously.
Occasionally in thyroid surgery the parathyroid glands are injured or removed,
produc-ing a disturbance in calcium metabolism. As the blood calcium level
falls, hyperirritability of the nerves occurs, with spasms of the hands and
feet and muscle twitching. This group of symp-toms is termed tetany, and the
nurse must immediately report its appearance because laryngospasm, although
rare, may occur and obstruct the airway. Tetany of this type is usually treated
with in-travenous calcium gluconate. This calcium abnormality is usually
temporary after thyroidectomy.
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care.
The patient
may be discharged theevening of surgery or within 1 or 2 days. Therefore, the
patient and family need to be knowledgeable about the signs and symptoms of the
complications that may occur and those that should be re-ported. Strategies are
suggested for managing postoperative pain at home and for increasing
humidification. The nurse explains to the patient and family the need for rest,
relaxation, and nutrition. The patient is permitted to resume his or her former
activities and re-sponsibilities completely once recovered from surgery.
Continuing Care.
If
indicated, a referral to home care is made.The home care nurse assesses the
patient’s recovery from surgery. The nurse also assesses the surgical incision
and reinforces in-struction about limiting activities that put strain on the incision
and sutures. Family responsibilities and factors relating to the home
environment that produce emotional tension have often been implicated as
precipitating causes of thyrotoxicosis. A home visit provides an opportunity to
evaluate these factors and to sug-gest ways to improve the home and family
environment. The nurse gives specific instructions regarding follow-up visits
to the physician
or the clinic, which are important for monitoring the thyroid status.
Related Topics